Pneumopericardium is defined as the nearness of air inside the pericardial space. It rarely happens after blunt or penetrating chest trauma and may likewise occur iatrogenically. ‘Simple’ pneumopericardium provides no perceptible circulatory collapse and patient are asymptomatic; nonetheless, simple pneumopericardium in 37% of cases complicate to circulatory collapse and so called ‘tension’ pneumopericardium. Tension pneumopericardium requires rapid evacuation of the pericardial sac by percutaneous or open drainage strategy. Inability to accomplish rapid effective drainage may bring about cardiac arrest. Diagnosis is done through an erect chest X-ray. Echocardiography and chest computed tomography scans can also support the diagnosis. We are here to report a patient with clinically and radiologically affirmed pneumopericardium caused by chest blunt trauma that was spontaneously relieved.
El neumopericardio se define como la proximidad de aire dentro del espacio pericárdico. Raramente ocurre tras traumatismos contundentes o penetrantes, y puede producirse iatrogénicamente. El neumopericardio ‘simple’ no aporta colapso circulatorio perceptible, y los pacientes son asintomáticos; sin embargo, en el 37% de los casos el neumopericardio simple se complica con colapso circulatorio y el denominado neumopericardio a ‘tensión’, que requiere una evacuación rápida del saco pericárdico mediante estrategia percutánea o de drenaje abierto. La imposibilidad de acometer un drenaje rápido efectivo puede derivar en paro cardiaco. El diagnóstico se realiza mediante placa de tórax en posición erguida. La ecocardiografía y la CT de tórax pueden respaldar también el diagnóstico. Reportamos aquí el caso de un paciente con neumopericardio confirmado clínica y radiológicamente, causado por traumatismo contundente de tórax, que se resolvió espontáneamente.
Pneumopericardium is defined as the nearness of air inside the pericardial space which results from many reasons like: positive pressure ventilation, thoracic procedures/pericardial fluid evacuation, penetrative trauma, blunt trauma (rare), pericarditis with gas-forming organisms, or connection between the pericardium and an adjacent air-containing organ such as stomach or esophagus. It is not as common as pneumothorax or pneumomediastinum1,2 pneumopericardium may be ‘Simple’ without circulatory collapse and patients are asymptomatic; however, simple pneumopericardium in 37% of cases advances to produce circulatory collapse, when it is termed ‘tension’ pneumopericardium. Tension pneumopericardium requires rapid evacuation of the pericardial sac by percutaneous or open drainage strategy. Pneumopericardium can be diagnosed by an erect chest X-ray in minutes. Treating the condition relies upon the clinical seriousness. This report describes a multi trauma patient with pneumopericardium.
Case reportA multi trauma male patient of 32 years old caused by motor car accident presented to our hospital. His primary survey showed a patent airway, central trachea and equal air entry bilateral, soft and undistended abdomen, the pelvis was stable and no long bones fracture was noticed. Vital signs were fair and the patient was hemodynamic stable with Glasgow coma score on arrival was 15/15, a foley catheter was inserted showing hematuria.
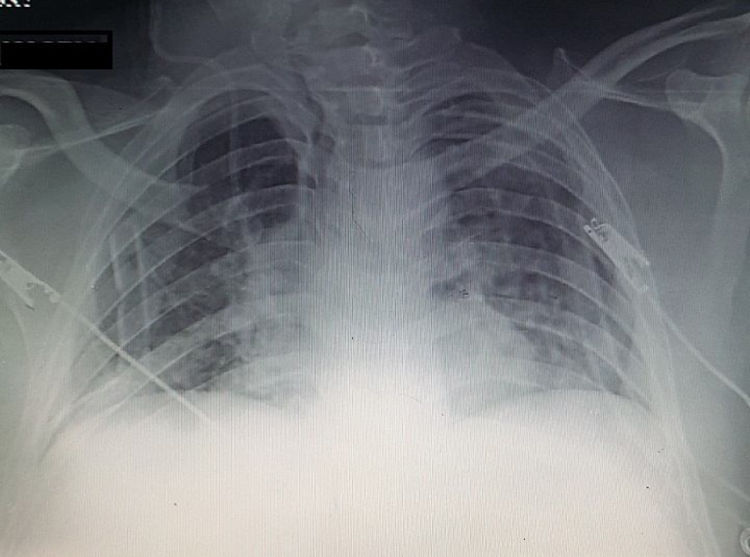
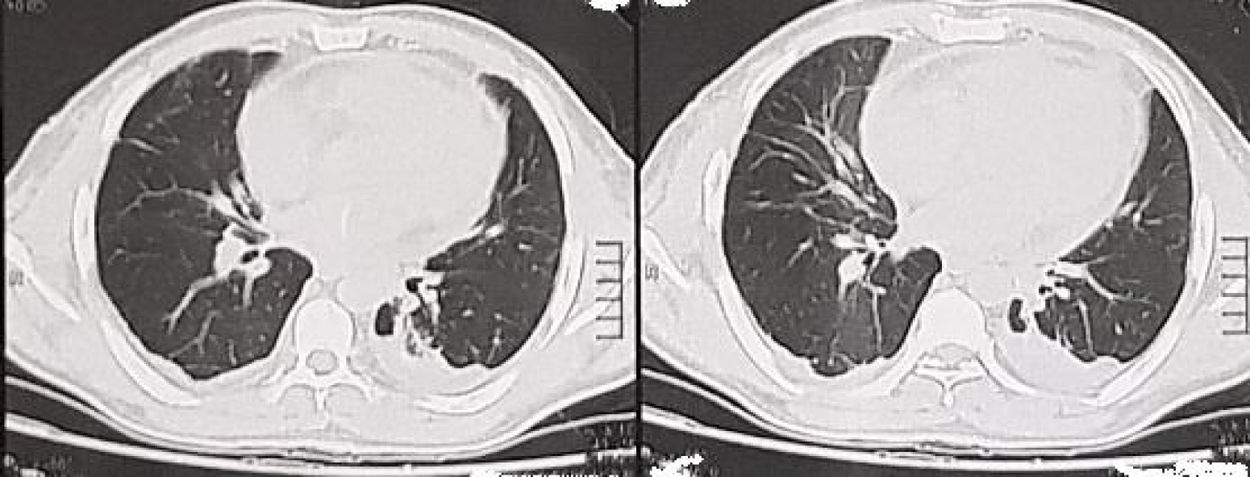
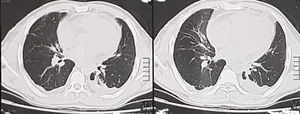
Abdominal Ultrasound noticed mild to moderate intra-peritoneal collection, CT chest showed pneumopericardium (Fig. 1), an echocardiogram was done to assess the ejection fraction and echo signs of cardiac tamponade, CT abdomen with intra-venous contrast showed urinary bladder injury.
Patient was hemodynamic stable and there was no need for urgent pericardial drainage, bilateral chest tube thoracostomy were done as a prophylactic maneuver to prevent developing of tension pneumothorax as a complication of pneumopericardium especially that this patient is going to be under general anesthesia for laparotomy, in correlation with CT abdomen findings a mini laparotomy was done in which the bladder injury was repaired.
Patient was admitted to intensive care unit for monitoring of vital signs post-operatively and prevent sudden collapse that may caused by tension pneumopericardium. Patient was followed up regularly with erect chest X-ray to assess resolving of pneumopericardium and follow up the patient (Fig. 2).
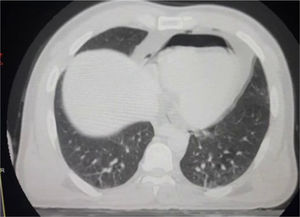
4 days later one chest tube was removed and another 2 days later the other tube was removed. 10 days after the accident a CT chest was done to the patient showing total resolve of the pneumopericardium (Fig. 3).
DiscussionPneumopericardium is defined as the presence of air into the pericardial space. The major etiology is trauma, most of which blunt chest trauma. It is a rare condition, associated with a high mortality rate (up to 57%) when causing cardiac tamponade, or to associated trauma, considering it is generally found in high-energy accidents. Air may enter the pericardial space by various ways. Without a direct communication, it has been suggested that pulmonary interstitial air may follow along the pulmonary peri-vascular sheaths from destroyed alveoli (the Macklin effect) or by a congenital pleura-pericardial connection. Another mechanism would consist in direct apposition of tracheobronchial and pericardial tears. Since our patient did not present pneumothorax upon arrival, his pneumopericardium probably resulted from the Macklin effect or from the rupture of a non-primary bronchus.3
Significant pneumopericardium that causes cardiovascular unsteadiness is called ‘tension pneumopericardium’ and it rarely causes hemodynamic instability. This may result from a ‘single-direction valve’ mechanism within a pleuropericardial fistula, permitting the rising pleural pressures associated with positive pressure ventilation to be transmitted into the pericardial sac (although effective pleural evacuation with thoracostomy tubes).4 Treatment of “Simple pneumopericardium” may be conservative, but tension pneumopericardium mandates decompression by percutaneous or open drainage.4
Simple pneumopericardium may advance to tension pneumopericardium. This has been accounted for to happen in up to 37% of cases and is unequivocally associated with positive pressure ventilation.5,6 Transformation to ‘tension’ often happens especially in ventilated patients, so prophylactic drainage of the pericardial sac is reasonable. Transformation to tension pneumopericardium happens in more than 70% of cases mostly the neonates undergoing mechanical ventilation but it is very rare in trauma patients.5
Some reported that prophylactic pericardial decompression of simple pneumopericardium before starting mechanical ventilation is mandatory.4 On the other hand, others advice that the patient can be closely monitored without intervention.3 Both percutaneous and open drainage of the pericardial sac are intrusive maneuvers with considerable risk of morbidity and mortality that should be saved for patients complicated with hemodynamic collapse due to cardiac tamponade. Ventilated patients are of higher risks of course.7
Tension pneumopericardium demands rapid evacuation of the pericardial sac. This may be done by percutaneous or open technique. This case demonstrates that simple pneumopericardium may be treated conservatively by close monitoring of the patient and rapid detection of any hemodynamics collapse.8
ConclusionSimple pneumopericardium can be treated conservatively with no need of prophylactic drainage of pericardial sac.
Ethical considerationThe study was approved by the ethical committee of the faculty of medicine Suez Canal University.
Informed verbal voluntary consent from participants was obtained.
The participant was informed that he/she has the opportunity to decide to consent or not without intervention of any element of force, fraud, deceit, duress, or undue influence on the subject decision.
Information confidentiality should be kept in analysis and data collection.
The techniques used in data collection, investigations shouldn’t be harmful to screened population
The research material and information was shared with others aiming advances in medical knowledge.
Feedback of the results of the study was given to the faculty of medicine Suez Canal University.
Conflict of interestsThe authors declare no conflict of interest.