Introducción: Se realizó un estudio con el objetivo de identificar determinantes sociales de mortalidad infantil en zonas rurales en México, y recomendar estrategias para disminuir esta mortalidad.
Métodos: Se tomó una muestra por conveniencia de 16 municipios de bajo índice de desarrollo humano. Se identificaron fallecimientos de menores de un año de edad a través de registros oficiales y de entrevistas con autoridades civiles, personal de salud y líderes comunitarios. También se realizaron entrevistas a las madres de menores fallecidos.
Resultados: En casi todos los casos confluyeron determinantes intermedios relacionados con condiciones de vida y servicios de salud. Los eslabones críticos de la atención más frecuentes fueron el de los programas preventivos, y la demora de mayor ocurrencia fue en la provisión de atención en las unidades de salud. Se encontraron deficiencias en las políticas públicas intersectoriales que garanticen el acceso efectivo a los servicios.
Conclusiones: Para reducir la mortalidad infantil en áreas rurales de México, es imprescindible mejorar el acceso geográfico y cultural a los servicios de salud, así como incrementar los recursos y las competencias técnicas y de interculturalidad del personal de salud.
Background: The aim of this study was to identify determinants of infant mortality in rural areas in Mexico and recommend strategies for its decrease.
Methods: A study was conducted in a sample of 16 municipalities among those with the lowest index of human development. Infant deaths were identified through official data, records and through interviews with civil authorities, health workers and community leaders. Mothers of children who died were also interviewed.
Results: In most cases, deaths were related with intermediate social determinants (living conditions and health services converged). The most important critical factors were the prevention programs and delays in receiving healthcare. Deficiencies in intersectorial policies to guarantee effective access to health services were found.
Conclusions: To decrease infant mortality in rural areas of Mexico, geographic access has to be improved as well as investment in resources and training health personnel in intercultural competence and primary health care skills
Pagina nueva 1 1. Introduction
Mexico pledged to reduce mortality in children <5 years of age by two-thirds by the year 2015 with respect to the mortality rate in 1990.1 The population living in rural areas is the most affected.2,3 There are five main causes of infant mortality in Mexico: respiratory distress of the newborn, other respiratory disorders, congenital malformations of the circulatory system, influenza and pneumonia.4,5 The order and magnitude of these causes show variations among the states, and within the entities large inequalities are seen.6,7
Mexico has an indigenous population of ~15 million people, which corresponds to ~13% of the population. Most (60.7%) are located in the first quintile of poverty and with low social security coverage.8 A maternal mortality ratio three times higher has been reported among indigenous peoples, and infant mortality rate 1.7 times higher than in the rest of country.9 By the time of the study, the municipalities of lower human development index (HDI) were mainly located in seven states with large indigenous population (Veracruz, Puebla, Guerrero, Oaxaca, Chiapas, Chihuahua and Durango), similar to the situation in 2014.10
The conditions of housing, road development, access and quality of health services and some maternal characteristics (extreme ages, low education, multiparity and malnutrition) have been documented among the determinants of child mortality. Among the cultural factors, the subordinate position of women, ethnic discrimination and other factors related to community participation, income, institutional fragility and the social and economic development are mentioned.8-16
To reduce infant mortality, the Economic Conference for Latin America and the Caribbean (ECLAC) recommends improving health interventions aimed at women before and during pregnancy, increasing breastfeeding and improving sanitary conditions.17 In 1982, the United Nations Fund for Children (UNICEF) suggested growth monitoring, oral rehydration, breastfeeding and immunization, food supplements for mothers and children and family planning.18 A review of the initiatives for child survival in Latin America in 2005 showed progress in these areas, but drew attention to neonatal diseases and acute respiratory infections and proposed focusing on the poorest population. PAHO has identified the inequities between urban and rural; disregard for indigenous groups; the absence of participatory models and provision of specific services for these vulnerable groups, lack of access to quality services from the first level of care; and guarantee of continuity of care.18-20
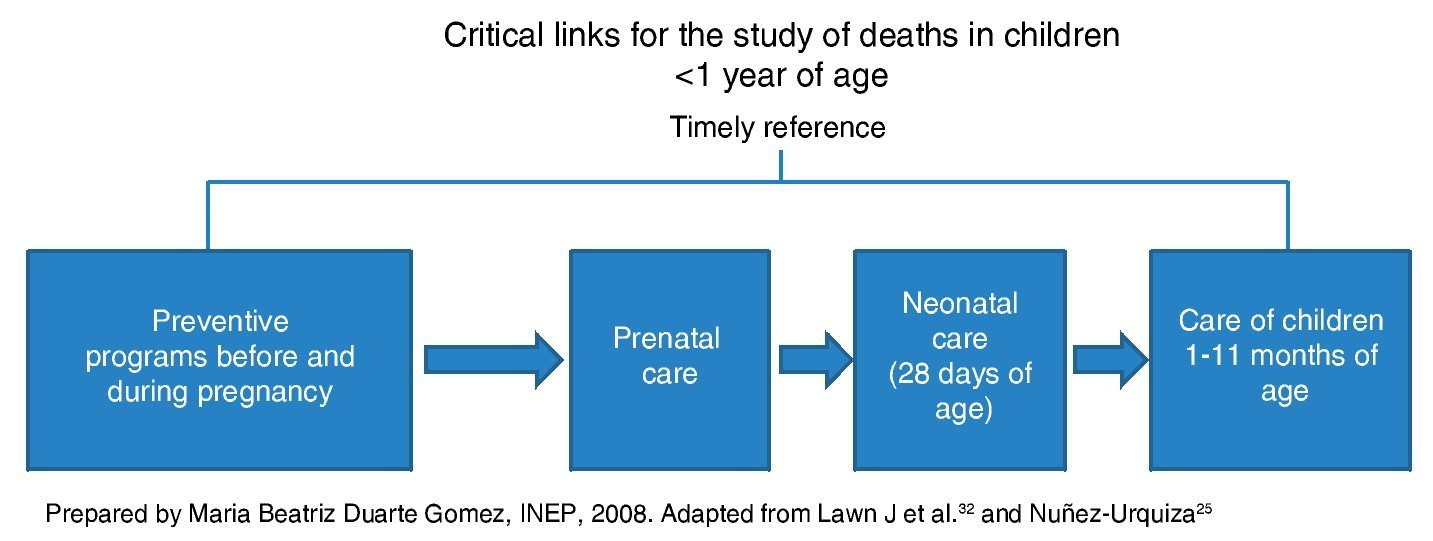
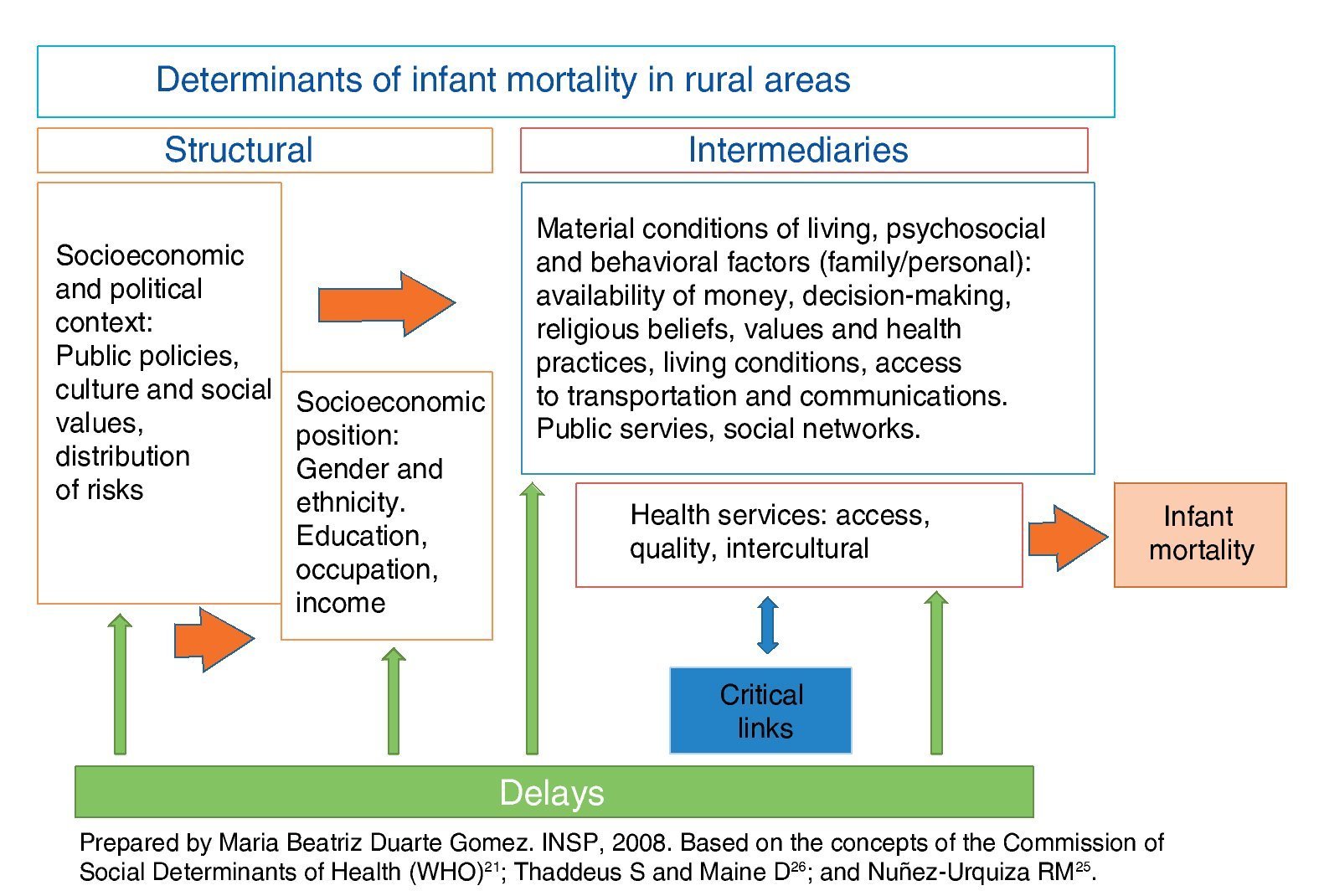
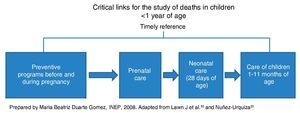
According to the Commission on Social Determinants of Health (CSDH) of the WHO, health is determined by the conditions in which people are born, grow, live and work,21 and groups the social determinants of health (SDH) into structural (related with the socioeconomic and political context, which in turn determine the socioeconomic position of the individual according to ethnicity, gender and social class), and intermediate (those that directly affect the health status, such as the material conditions of life, the family behaviors and beliefs and the health services).22,23 With respect to health services, for this study the concept of critical links in the process of care was used, which identify the omissions in care that are corrected, used in Mexico mainly for studying maternal death. For the case of infantile mortality a scheme was designed which begins with preventive programs before and during pregnancy (pre-pregnancy counseling, prenatal control in the first level of care, referral and second level of care), continues with intrapartum care and ends with care during the first year of age (Fig. 1).24,25
Figure 1 Critical links in care of babies <1 year of age. Critical links for studying deaths in children <1 year of age.
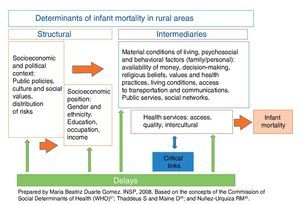
For the analysis of the SDH of infant mortality in the selected municipalities conceptual elements of the model of the three delays proposed by Thaddeus and Maine for maternal mortality were used. The first delay occurs in the family environment, and refers to the delay in recognizing the need for care and to look for it, be it due to lack of information or for cultural reasons. The second is to arrive to the health care department due to economic, geographic and transportation difficulties; and the third is the delay that occurs within the unit of care to provide a timely and adequate level of care.26 This model is not only related with health services (delay 3), but also with structural determinants that favor or hinder access to those services and that affect individual behaviors that are socially constructed based on both personal experience and the social and cultural context in which they live.27,28 Based on these elements a conceptual framework was designed that linked the critical links with health services and the model of three delays with the determinants proposed by the WHO (Fig. 2).
Figure 2 Social determinants, delays and critical links associated with infant mortality in those municipalities representing a low level of the Human Development Index (HDI) (Mexico, 2007).
In line with the national policy of prioritizing actions in the poorest communities29 of the 101 municipalities with the lowest HDI, the National Center for Health of Children and Adolescents (CENSIA) of the Health Ministry (SSA), directed this study in order to identify the most important social determinants of infant mortality in rural areas of social under-development in Mexico. For the operational work we had the support of the State Health Systems (SESA).
2. Methods
This exploratory study with a transversal design and sampling by convenience was conducted in 27 locations of 16 municipalities with low HDI from six states: Chiapas, Oaxaca, Veracruz, Guerrero, Chihuahua and Puebla. From each entity were selected two municipalities from the list of 101 with lower HDI, whose county seat was located two hours or more from the Sanitary District. In turn, from each municipality two locations were selected, one with infant mortality recorded in the last year and another without infant mortality recorded. The latter was to seek out deaths which had occurred, but had not been recorded. Interviews were conducted with 93 key informants, of whom 68 were health personnel. Informed consent was used for the interviews and confidentiality was guaranteed. The field work was conducted by the researchers themselves.
To identify the infant death occurred in the last year, the primary source was the local civil registry. We also inquired with key informants from the community, such as the local health director and health personnel on the following topics: deaths in children <1 year of age and sociodemographic characteristics, perception of the determinant factors of infant deaths, empowerment of women (making decisions about health in the family), suggestions for reducing child mortality; all of the above through a questionnaire. Frequencies and averages of the sociodemographic information were obtained. In addition, semi-structured group interviews were conducted with local health staff, with a guide that contained topics similar to those of the questionnaires, as well as with women beneficiaries of the program “Oportunidades” gathered for this purpose. The interviews were recorded, transcribed and organized thematically in Excel (Microsoft Office) program. Finally, infant mortality data from the towns were compared with those from the relevant jurisdictions to identify unreported cases in the towns because the deaths occurred in secondary hospitals.
To document the care processes, in addition to the interviews, observation visits were made to 57 health units from those of primary contact, such as houses and health centers to community hospitals and centers of reference of first and second level of care. A checklist used to record the availability of human, equipment and supplies resources. The health personnel information was categorized according to the deficiencies mentioned by respondents (adequacy and training of human resources, equipment and infrastructure, distances and means of communication), which was supplemented with observation.
An interview called Verbal Autopsy (VA) was done with the relatives of the deceased infants and consisted of a semi-structured questionnaire about the events that took place prior to the death. The design was based on the verbal autopsy used regularly by the SSA and by other investigators.30,31 The interview was carried out in the homes of the families. In cases in which the mother did not speak Spanish, bilingual local staff was used for the translation. Data were also collected from the VA of children <1 year of age who died as a result of acute diarrheal diseases (ADD) and acute respiratory infections (ARI), done routinely by State Health Departments.
Information from staff interviews, as well as the VA, was captured in Excel (Microsoft Office) program in separate databases: one on the availability of resources with information from questionnaires of health personnel; one with the opinions of health personnel on the determinants of infant deaths and the proposed community and health system interventions; and another with the data of deaths found in every state (municipality, source of information, cause of death, age at death, place of death, presence of a death certificate). Finally, the information was summarized by state and municipality regarding the delays and critical links present in every death, obtained from all available sources of information for each case.
3. Results
Information was obtained on 119 deaths in children. In 50 of these children there was VA, 27 of which were done by the research team. The remaining cases were already done by the personnel from the SESA according to the VA rules in deaths by ADD or ARI in infants.
Regarding the sociodemographic characteristics of parents, 70% lived in a free union, 91% of mothers and 82% of parents were speakers of an indigenous language, and 16% were illiterate. The majority of fathers were farmers and the mothers were housewives. Average age of the mothers was 26 and fathers 33 years.
In terms of age of death, 50% of were post-neonatal infants (>4 weeks of age) and 50% were newborns. Of these deaths, 35% occurred in the early neonatal period (0-7 days old) and 15% in the late neonatal period (8-28 days of life).32
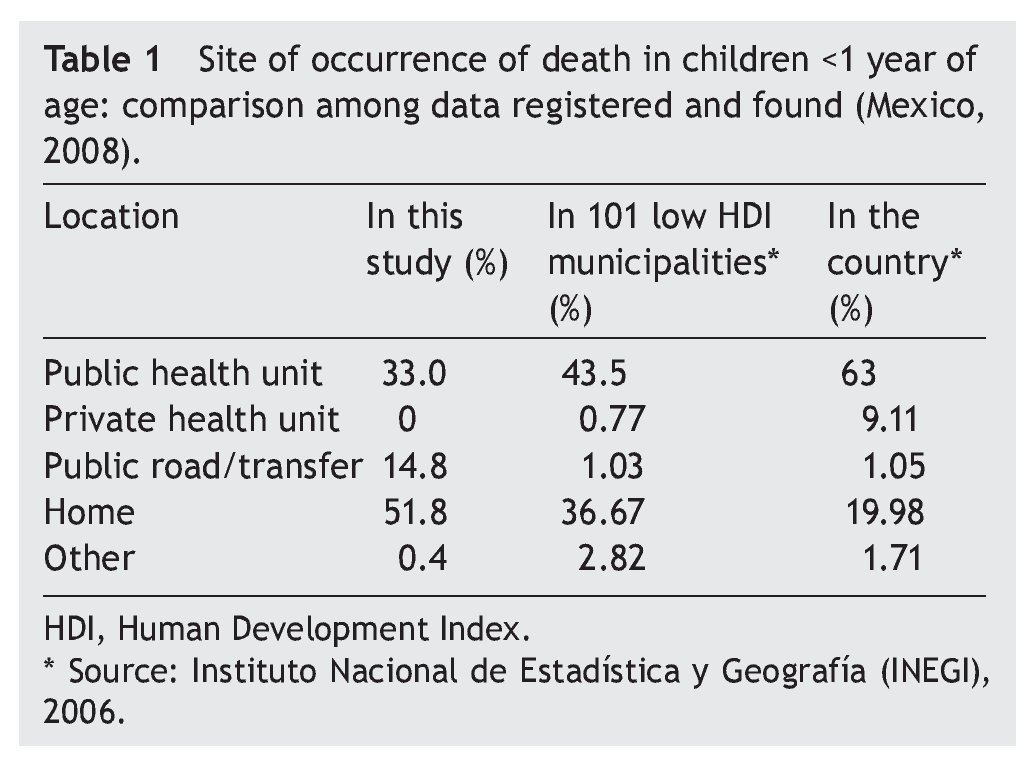
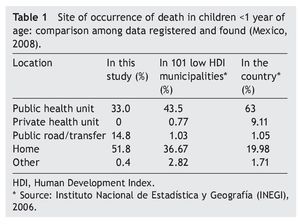
Half of the births of the infants who died were home births. In 76% of cases the family sought health care when the child became ill. However, 65.6% of deaths occurred outside a medical unit: 51.8% in the home and 14.8% in public places (Table 1).
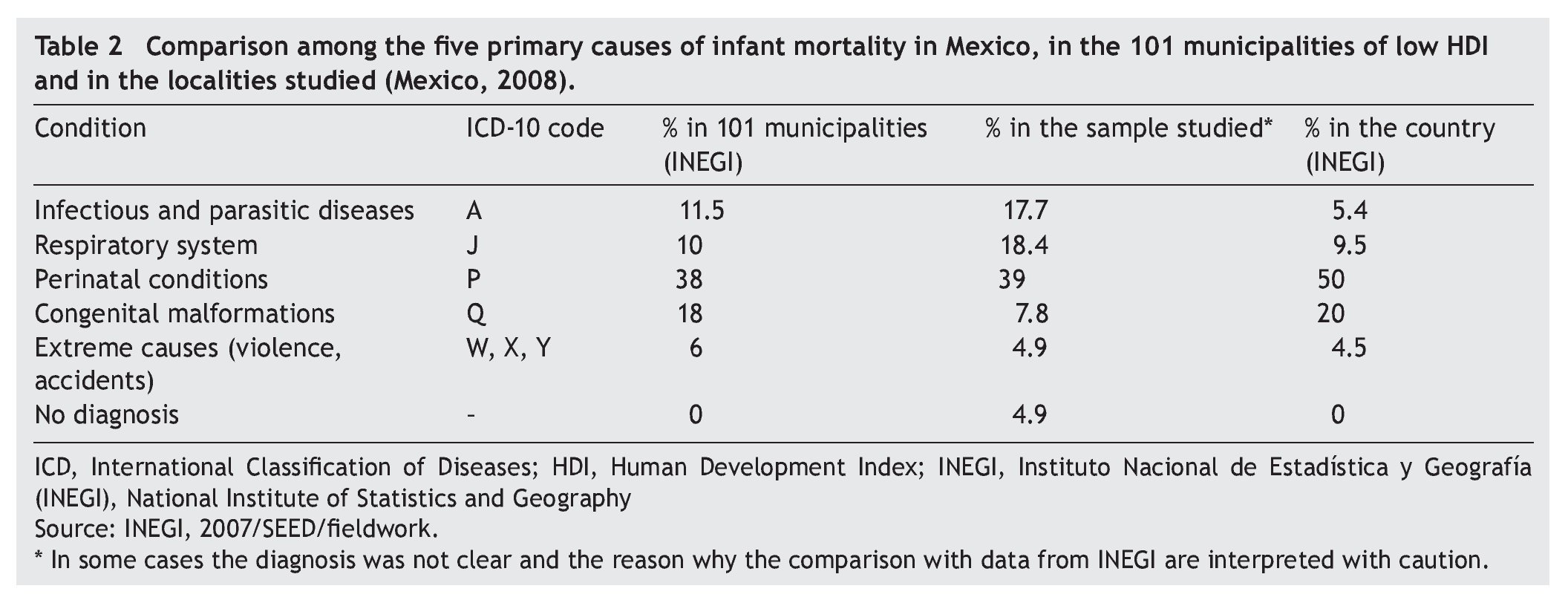
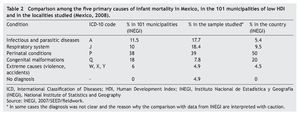
The main causes of death were perinatal conditions followed the ADD and ARI (Table 2). Most of the neonatal deaths were due to ADD and ARI, whereas neonatal causes were mainly prematurity. No death certificate was found for 14 deaths (11.7%).
3.1. Social determinants
The perception of health personnel is that infant death is related to social determinants such as malnutrition, poverty, and ignorance. They noted the absence of systems for distributing drinking water and proper sewage disposal as causes of disease, which favors the presence of diarrhea. The opinions about the reasons why children die at home are lack of money, transportation and routes of communication, ignorance and some cultural aspects (preference for traditional medicine agents, mother submissive to the decisions of the mother-in-law). In the case of respondents outside the health sector, in addition to the above reasons, they mentioned the inadequate care in health services “they do not serve them well.”
In most cases (78%) intermediate determinants converge related to living conditions, psychosocial and behavioral factors, and with the health system. For example, in the case of a 4-month-old child whose symptoms of ADD initiated at 8 pm, at 11 pm he was taken to the health center, but there was no physician available at night. There was also no public transport, no ambulance and they had no money to pay a private transport. He died at home, not even receiving oral fluids. The mother was 18-years old and illiterate (Case 8, Veracruz).
Low income and high parity also determine the health and nutrition of women before and during pregnancy.
“Almost all of our mortality is concentrated in that there is no generally optimal status of the mother, whether economic, nutritional, parity, or prenatal control. Everything hinges with the mother. The rest is the care at delivery and the rest is still representative of the third world” (Pediatrician, Tlapa, Guerrero).
Delays were related to both structural determinants as well as intermediate. In 32% of cases the first delay was documented due to lack of knowledge of warning signs in the family because of communication problems with the health personnel who do not speak the regional language, the limited empowerment of women, the low level of education of both parents, and the language of the residents, which hinders the understanding of the information provided by health personnel to identify warning signs. Additional obstacles are the beliefs related to health, nutrition or medical care and practices such as first going to a healer and reluctance to go to the health unit due to their beliefs or previous negative experiences. This conditions the first delay–the time lost until the need to go to a health service unit is realized.
The second delay was detected in 22% of cases. Some of the living conditions that generated delays in reaching the health unit were as follows:
a) Lack of roads, public transport and means of communication (radio, telephone). Most arrived on foot (58%); only 18% used public transportation to come to the health unit and 24% used private transport.
“…children of 1 year of age die because they live in remote areas where no physicians are available and they die on their way to the hospital…when there is an emergency there is no transportation to bring them to a health center.” (Health director; Puebla, File 41).
b) Lack of economic resources to pay for transportation to the primary care unit or to the referral hospital.
“They sent us to the IMSS hospital, but my husband had no money for transportation” (Case 1; San Agustín Loxicha, Oaxaca).
c) Lack of autonomy of the women to make decisions on seeking care. In this regard, it was mentioned that women do not go to health centers without the authorization of the husband or the mother-in-law; in 22% of the cases the interviewees manifested that grandparents decide whether or not medical assistance is sought and when:
“The grandmother did not allow the child (with diarrhea) to be brought to the clinic because if the child died in the clinic, his/her spirit would remain there.” (Physician, UMR; Oaxaca).
Finally, deficiencies were found in health services which comprise the type 3 delays in 40% of the cases: deficiencies in the assessment of the risk or severity of the health status of the child or lack of equipment or negligence or a combination of factors.
3.2. Human resources
1. Availability—Due to working conditions, some comprehensive community hospitals did not have the basic four specialties. In some hospitals there are specialists available one or two days a week because the specialized medical personnel do not wish to live in small towns.
2. Training—This was the deficiency found with greatest frequency (76% of the cases). Training of personnel at the first level of care, including assistants at the health units, is insufficient for caring for infants with neonatal problems, detecting signs of alarm in cases of ADD and ARI, and for making a timely referral. This is especially delicate in remote regions, from where the transfer to another level of care is difficult.
3. Attitude—Negligence or lack of sensitivity of the personnel was obvious in three cases. For example, in the case of a 5-month-old child with diarrhea and vomiting, oral fluids were begun at home. The child was brought to the Health Center where they prescribed oral fluids and syrup. They returned the next day because the child was doing very poorly. The parents state that they asked the physician to keep him at the Health Center or to refer him to the hospital, but he was once again sent home. The child died a 30 min later en route to the home (Case 4; Chiapas).
An administrator of a Chiapas health unit said: “We must pay more attention to patients because sometimes the staff are bored and treat them poorly.” (Chiapas, File 13). In every state, the staff of State Departments of Health agreed on the concern about the low quality of care by physicians in private practice, mainly for diarrhea. They comment that “they prescribe antibiotics, but do not hydrate.”
3.3. Budget, equipment and access to supplies
Only 22.7% of health centers visited were accredited by the Accreditation Program of the General Health Council. Community hospitals did not have a team to resolve complications such as transfer incubators or oxygen, which adds another factor to the delay in obtaining timely care. “We need supplies; sometimes we do not have the most basic” (Physician, Puebla, File 48).
The area supervisory teams of the health departments make few visits due to the lack of financial resources for travel expenses. There are problems of geographical access to the hospitals due to the poor state of the roads and lack of public transportation. Some localities have ambulances, health vans or community transport vehicles, but these may be inadequate for the unpaved roads.
Lack of communication equipment was another factor. With the exception of the rural health units of Veracruz, about half of the other localities had trouble communicating with a higher level of care, which leads to the referral of cases that could be treated or stabilized in the first level care unit, thus improving the chances of survival. Lack of intercultural approach to health services also generates distrust and communication problems.
Despite the extensive affiliation with the Seguro Popular Health Insurance and the strengthening of the distribution of supplies, shortage of medications was found; in one locality even childbirth is charged. Based on these observations, we can say that the financial protection of the health system has not yet fully reached these municipalities.
As an example of type 3 delay, there were three perinatal deaths reported of children of indigenous women who sought medical care during labor but were sent home by the physician. Death of the infants occurred at home.
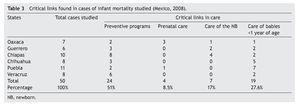
The problems of services as determinants of health outcomes are not limited to the time when accessing emergency care, but throughout the entire process of maternal/ infant care (Table 3). There were deficiencies found in half of the cases in the preventive programs such as family planning and health literacy. Among births taking place in health units, few problems were documented during labor and delivery and during care of the newborn. With respect to post-natal care, ~50% of cases demonstrate lack experience of the health personnel in the management of diarrheas and respiratory infections, e.g., lack of detection of alarm signs, omission of parenteral hydration and delay in referral to a health center of a higher level of care.
4. Discussion
The majority of deaths were avoidable with the knowledge and technology available, which constitutes an inequity between the most marginalized populations and the average of the country. The findings confirm that the health status is socially determined by the degree of social marginalization, which limits access to power and to the resources of the vulnerable groups: indigenous, female and economically disadvantaged.22 Biopsychosocial factors intervene simultaneously in the results of infant health; especially important is the intersectoral work to decrease the inequities in access to public services (education, transportation, potable water) and the health system as an intermediate determinant to catalyze the impact of social marginalization.33
The precarious quality of life characterized by isolation, limited economic resources, lack of sanitation and social marginalization along with poor access to services and opportunities for social and human development in these localities with an indigenous majority defined, largely, its material conditions of life in turn influence the determination and ability to access health services. These conditions create risks of malnutrition, which cause immunodeficiencies and health risks and may explain the higher proportion of postnatal deaths (50%) compared with other global statistics (34%). Although policies have been generated and programs of different sectors destined for the rural population,34 the desired coverage and effectiveness in the most marginalized rural areas have not been achieved.
Structural determinants underlie the deaths found and manifest the dissatisfaction of the needs of the population and the lack of public policies that guarantee decent living conditions. The delays detected are related both to the structural determinants (absence of policies to ensure the geographic and economic access to services) as well as the intermediate determinants.
Given the existence of structural determinants that place indigenous and rural communities in a vulnerable social position, health services, which should serve as a catalyst for social disadvantage, have not worked, and its failure has contributed to the occurrence of avoidable deaths. Problems in access, quality and timeliness of services are themselves one of the social determinants of child mortality.
If health services are to be used to reduce social inequalities, the health sector needs to invest additional resources and improve the organization to efficiently and effectively fulfill its task of providing affordable, good quality health-care and intercultural approach to rural and indigenous communities. This weight of the determinants derived from health services is an opportunity, because it is an issue on which the health system can have a direct influence and in a short time if the political will is positive.
Achieving greater efficiency of health systems internationally has been identified as a priority factor to reduce infant mortality, mainly perinatal. Various factors are required:
a) Improve the capabilities of community personnel and of the first level of care, which includes effective intercultural communication skills.
b) Eliminate barriers for timely and good quality care (including transportation for emergencies).
c) Promote healthy community practices.
d) Facilitate active community participation in the decisions related with their living conditions.35,36
Although making visible the differences and inequities among the population of these municipalities was not part of the objective, information was included about deaths outside the institution and mortality due to preventable causes socially determined as indicators of inequities in health. Except for the limitations in the postpartum follow-up, the determinants found related with the health system coincide with other studies: home births without qualified care during labor and lack of capabilities of the health personnel to care for newborns and infants with acute problems.37 The latter was detected both in health assistants as well as primary care medical personnel. Deficiencies in the first level of care make it necessary to plan the health system with a focus on complete primary care, which includes community participation. One strategy is training of native personnel from the region. Health assistants especially, who are the first contact in the remote communities, are the personnel who should fortify their skills with further training, equipment, means of communication and adequate transfers. For this reason it is fundamental to include these health assistants in programs of improvement of competencies. In addition, to reinforce medical oversight and supervision in the remote health units, guarantee placement of equipment in the first level of care for the newborn and the infant with complications. Also, offer optimal conditions for referrals and guarantee availability of pediatricians in the comprehensive hospitals with strategies for intersectoral coordination.
Despite the geographic, economic and cultural obstacles, most mothers arrived at the health clinics when their child became ill, demonstrating confidence in the services. However, when complications arise, the problems of resolution at the first level of care and of accessibility to the second level were documented in other studies,38 confirming the need to strengthen primary care and rural secondary hospitals as well as improving routes of communication and transportation according to the geographical characteristics of each region.
Because family behaviors and personal decisions are socially determined, it is necessary to know the social context of each locality and implement health promotion strategies to address the social determinants of maternal and child health with participative methodologies and with an intercultural approach.
Faced with evidence of the importance of pre-pregnancy health,38-44 further research and care directed at the health of women and men of reproductive age is required, as promoted by the National Program for Maternal and Perinatal Health. This should be done in order to reduce the chances of health problems during pregnancy and the first year of life,45 mainly those derived from chronic conditions in poor women such as malnutrition, anemia and urogenital infections.
This study had some limitations including a lack of precision in some diagnoses when they came from VA and deaths that occurred at home, and lack of access to some mothers to complete the VA due to migration of the families or the road conditions. Given the exploratory nature of the study, studies with mixed methodologies are needed that delve deeply into the relationship with other determinants such as ethnicity, migration, education, culture and social exclusion in a manner suggested by other authors.46 Other studies should be designed that measure the relative weight of the different social determinants of infant mortality in different regions of the country.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Funding
Centro Nacional de Atención de la Infancia y la Adolescencia de la Secretaría de Salud.
Conflict of interest
The authors declare no conflict of interest of any nature.
Acknowledgments
The authors extend their appreciation to the health personnel of the states and to those respondents of the visited communities.
Received 19 February 2015;
accepted 15 June 2015
☆ Please cite this article as: Duarte-Gómez MB, Núñez-Urquiza RM, Restrepo-Restrepo JA, Richardson-López-Collada VL. Determinantes sociales de la mortalidad infantil en municipios de bajo índice de desarrollo humano en México. Bol Med Hosp Infant Med. 2015. http://dx.doi.org/10.1016/j.bmhimx.2015.06.004
* Corresponding author.
E-mail:beatriz.duarte@insp.mx, mbduarte52@yahoo.com (M.B. Duarte-Gómez).