To determine the incidence of pulmonary complications associated with mechanical ventilation in patients admitted to a second level hospital neonatal intensive care unit (NICU).
MethodsRetrospective analytical study records of newborns admitted to NICU who receiving mechanical ventilation in a secondary hospital health care. Demographic mechanical ventilation, intubation and complications data reported in the clinical record were collected and analyzed.
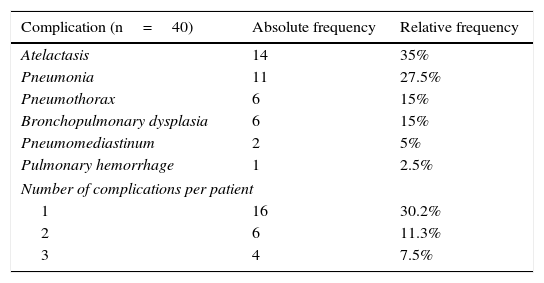
ResultsIn 53 patients selected, a total of 40 complications were found. The annual incidence of pulmonary complications associated with mechanical ventilation in the NICU, at a second level hospital at Sonora was 49.05% (95% CI 0.35 to 0.62). The most frequent pulmonary complications were atelectasis 35%, pneumonia 27.5%, pneumothorax 15%, bronchopulmonary dysplasia 15%, pneumomediastinum 15% and pulmonary hemorrhage 2.5%.
ConclusionsThe presentation of pulmonary complications secondary to mechanical ventilation in neonatal patients is similar to that reported in developing countries. Atelectasis is the most common pulmonary complication in neonatal patients undergoing mechanical ventilation.
Se buscó determinar la incidencia de complicaciones pulmonares asociadas a ventilación mecánica en pacientes ingresados a un servicio de cuidados intensivos neonatales (UCIN) en un hospital de 2° nivel.
MetodologíaEstudio analítico retrospectivo en expedientes de recién nacidos ingresados a una sala de UCIN y que recibieron ventilación mecánica en un hospital de segundo nivel de atención médica. Se recabaron datos demográficos, de la ventilación mecánica, la intubación y complicaciones reportadas en el expediente clínico y se analizaron en el programa estadístico SPSS 20.
ResultadosDe los 53 pacientes seleccionados se encontraron un total de 40 complicaciones. La incidencia anual de las complicaciones pulmonares asociadas a ventilación mecánica en el área de UCIN del servicio de Neonatología, en un hospital de segundo nivel en Sonora fue de 49.05% (IC 95% 0.35-0.62). Las complicaciones pulmonares más frecuentes fueron: atelectasia 35%, neumonía 27.5%, neumotórax 15%, displasia broncopulmonar 15%, neumomediastino 15% y hemorragia pulmonar 2.5%.
ConclusionesLa presentación de complicaciones pulmonares secundarias a ventilación mecánica en pacientes neonatales es similar a lo reportado en países en desarrollo. La atelectasia es la complicación pulmonar más frecuente en los pacientes neonatales sometidos a ventilación mecánica.
Ventilatory assistance allows for the recovery and maintenance of the patient with cardiorespiratory failure. Thanks to this intervention, many neonatal patients’ lives are saved in the neonatal intensive care units (NICUs). Nevertheless, the use of this supportive therapy induces lung injury, leads to irreversible structural damage and alters respiratory and hemodynamic function causing complications that impact the patients’ evolution and prognosis1–5.
Scientific advances have allowed relying on new and better devices for respiratory assistance, which have decreased neonatal mortality but not complications secondary to their use, given that many of them, especially premature neonates, depend on the level of pulmonary development of the patient6.
Risk factors of the premature patient that make him more vulnerable to complications secondary to mechanical ventilation have been widely described. Factors that stand out include central neurologic maturity and respiratory muscle weakness, poor alveolar development of the lungs, deficient surfactant synthesis and increase of alveolar-capillary membrane thickness7. Also, some patient-related factors such as gestational age less than 29 weeks, birth weight less than 1500g, neonatal sepsis, male gender and the presence of a persistent ductus arteriosus, as well as ventilator support, FiO2 concentration and the number of days on ventilator support8–12.
Recent articles demonstrate the relationship between mechanical ventilation and lung injury in the preterm patient, which has been directly associated with surfactant deficiency and the inflammatory effect that results from secondary invasion by ventilator support. In the same way, the utility of prophylactic surfactant has been demonstrated, which reduces mortality compared to therapeutic administration, and decreases the risk of bronchopulmonary dysplasia, pneumothorax and pulmonary hemorrhage13–15.
The frequency of complications associated with mechanical ventilation in pediatric patients has been reported between 40-150%, depending on the population, since one patient can present more than one complication8,9,11. At the national level, there is scarce information about this topic in the neonate. Lopez-Candiani et al., in 2007, reported a study conducted in Mexico City in neonates that were treated with mechanical ventilation. They found a frequency of complications of 81%, being the most common atelectasis, accidental extubation, hypoxia during intubation, hospital-acquired pneumonia and bronchopulmonary dysplasia10. Similar studies in our region are not documented.
The objective of the present study was to describe the presentation of pulmonary complications associated with mechanical ventilation in patients of a NICU in a secondary care hospital in Sonora, Mexico.
2MethodsUsing a transversal, analytic and retrospective design, medical records of patients admitted to the NICU, who required assisted mechanical ventilation for more than eight hours during the period of September 2014 to September 2015 were included. All the patients should have a complete medical record to fill the data sheet.
During the aforementioned period, a total of 238 patients were admitted to the NICU. Patients referred from other hospitals, patients with a diagnosis of congenital heart disease, congenital lung disease and patients with a dysmorphic syndrome were excluded, as well as those whose medical records were incomplete, and those who died in the first eight hours of life of causes unrelated to mechanical ventilation.
The study was conducted in a secondary care hospital in northeastern Mexico, where healthcare to the newborn population of the state's different municipalities is provided. This hospital is a teaching center with a pediatric residency program. Thus, residents together with attending neonatal specialists and pediatricians provide healthcare in the NICU. The NICU has an annual admissions average of 250-300 patients; during the period of study, 238 admissions were reported. The most frequent diagnoses of admission are respiratory distress syndrome (hyaline membrane disease), neonatal sepsis, transitory tachypnea of the newborn, and respiratory depression.
Consecutive cases were obtained for the sample. From each patient, the following data were registered: gestational age, gender, age at onset of mechanical ventilation, birth weight, days of mechanical ventilation, intubation attempts, surfactant administration, and the number of doses administered. Additionally, the complications associated to the ventilator that were referred in the medical notes were registered: pneumothorax, atelectasis, pneumonia, bronchopulmonary dysplasia, and pulmonary hemorrhage. The CDC (Centers for Disease Control; Atlanta, GA, USA) criteria were considered for the diagnosis of ventilator-associated pneumonia16. The diagnosis of bronchopulmonary dysplasia was based on the modified Bancalari criteria17,18. Data was concentrated in a database in Excel Office® for Windows® that was analyzed using the statistical program SPSS v20 for Windows®. Data analysis was performed using frequencies and percentages for the qualitative variables, and measures of central tendency (median) for the quantitative variables. χ2 and Fisher's exact tests were used for categorical variables, and Student's t test for quantitative variables. Incidence rate was used as a measure of frequency, and with categorical variables a Spearman's correlation was performed.
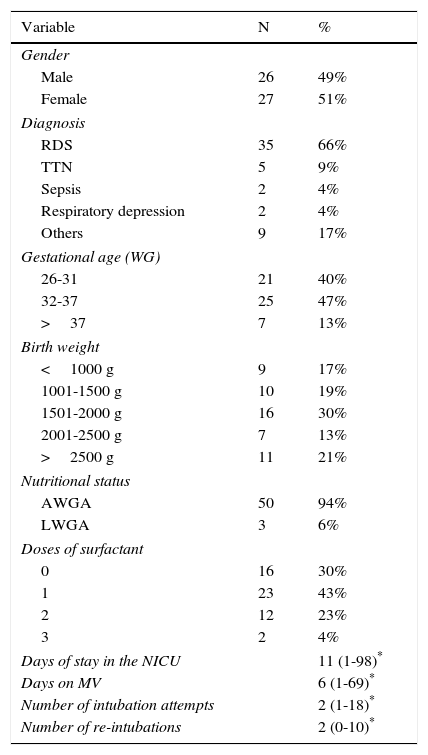
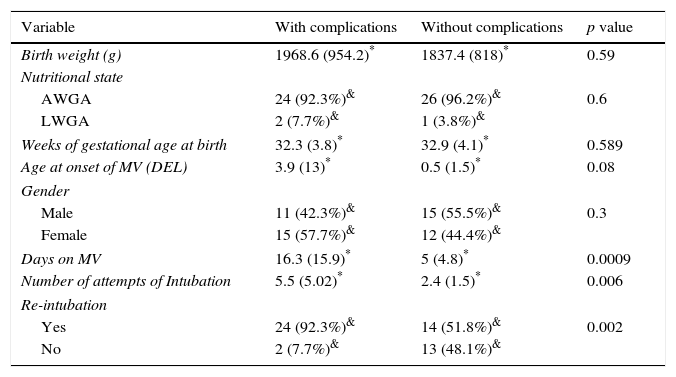
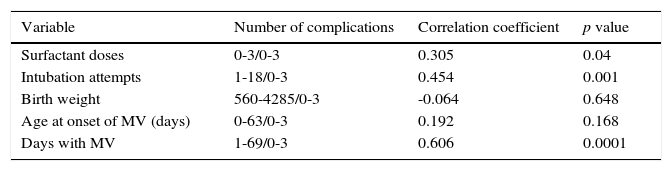
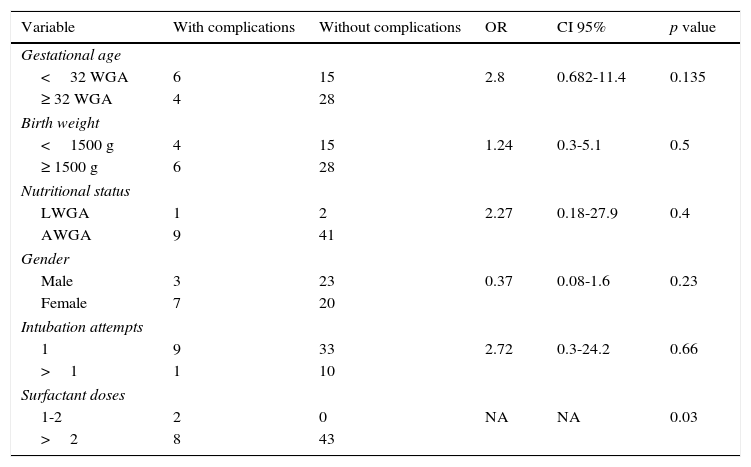
3ResultsFrom a total of 53 patients, 49% corresponded to male (n=26) and 51% to female (n=27) neonates. Preterm patients predominated (87% of the sample were<37 weeks of gestational age, an average of 32.66 weeks, and a standard deviation (SD) of 3.927), average birth weight was 1901g (SD=883g, minimum value of 560g and a maximum value of 4287g). The characteristics of the population are described in Table 1. A total of 40 complications arose. The incidence rate of complications associated with mechanical ventilation (MV) was 71.3 cases per 1000 days of ventilation and with pneumonia associated with MV, 19.3 cases per 1000 days of ventilation. The proportion of patients with a single complication was 30.2%; with two complications, 11.3%, and with three, 7.5% (Table 2). The most frequent pulmonary complications secondary to MV were atelectasis (35%), pneumonia (27.5%), pneumothorax (15%), bronchopulmonary dysplasia (15%), pneumomediastinum (15%) and pulmonary hemorrhage (2.5%) (Table 2). The main factors associated with complications in this series of patients were the age at onset of MV, the days of MV, the number of intubation attempts and the number of re-intubations (Table 3). A correlation of 0.731 between the number of pulmonary complications and the number of days on MV, and of 0.613 between the number of pulmonary complications and the number of intubation attempts (Table 4) were found. An estimation of the risk of developing multiple complications was assessed by calculating odds ratios (OR). A gestational age<32 weeks showed an OR of 2.8 (p=0.135), a birth weight<1500g had an OR of 1.24 (p=0.5), a low birth weight for gestational age compared to a normal birth weight for gestational age reflected an OR of 2.27 (p=0.4), male gender an OR of 0.37 (p=0.23), patients with more than one intubation attempt had an OR of 2.72 (p=0.66). Every patient who received three doses of surfactant presented with more than one pulmonary complication; hence, it was not possible to calculate and OR. However, a χ2 test revealed a p-value of 0.03 (Table 5).
General characteristics of the population on mechanical ventilation (N=53).
| Variable | N | % |
|---|---|---|
| Gender | ||
| Male | 26 | 49% |
| Female | 27 | 51% |
| Diagnosis | ||
| RDS | 35 | 66% |
| TTN | 5 | 9% |
| Sepsis | 2 | 4% |
| Respiratory depression | 2 | 4% |
| Others | 9 | 17% |
| Gestational age (WG) | ||
| 26-31 | 21 | 40% |
| 32-37 | 25 | 47% |
| >37 | 7 | 13% |
| Birth weight | ||
| <1000 g | 9 | 17% |
| 1001-1500 g | 10 | 19% |
| 1501-2000 g | 16 | 30% |
| 2001-2500 g | 7 | 13% |
| >2500 g | 11 | 21% |
| Nutritional status | ||
| AWGA | 50 | 94% |
| LWGA | 3 | 6% |
| Doses of surfactant | ||
| 0 | 16 | 30% |
| 1 | 23 | 43% |
| 2 | 12 | 23% |
| 3 | 2 | 4% |
| Days of stay in the NICU | 11 (1-98)* | |
| Days on MV | 6 (1-69)* | |
| Number of intubation attempts | 2 (1-18)* | |
| Number of re-intubations | 2 (0-10)* | |
RDS, respiratory distress syndrome; TTN, transitory tachypnea of the newborn; AWGA, appropriate weight for gestational age; LWGA, low birth weight for gestational age; NICU, neonatal intensive care unit; MV, mechanical ventilation; WG, weeks of gestation.
Pulmonary complications observed in the study population (N=53).
| Complication (n=40) | Absolute frequency | Relative frequency |
|---|---|---|
| Atelactasis | 14 | 35% |
| Pneumonia | 11 | 27.5% |
| Pneumothorax | 6 | 15% |
| Bronchopulmonary dysplasia | 6 | 15% |
| Pneumomediastinum | 2 | 5% |
| Pulmonary hemorrhage | 1 | 2.5% |
| Number of complications per patient | ||
| 1 | 16 | 30.2% |
| 2 | 6 | 11.3% |
| 3 | 4 | 7.5% |
Factors associated to complication in MV in neonate patients (N=53).
| Variable | With complications | Without complications | p value |
|---|---|---|---|
| Birth weight (g) | 1968.6 (954.2)* | 1837.4 (818)* | 0.59 |
| Nutritional state | |||
| AWGA | 24 (92.3%)& | 26 (96.2%)& | 0.6 |
| LWGA | 2 (7.7%)& | 1 (3.8%)& | |
| Weeks of gestational age at birth | 32.3 (3.8)* | 32.9 (4.1)* | 0.589 |
| Age at onset of MV (DEL) | 3.9 (13)* | 0.5 (1.5)* | 0.08 |
| Gender | |||
| Male | 11 (42.3%)& | 15 (55.5%)& | 0.3 |
| Female | 15 (57.7%)& | 12 (44.4%)& | |
| Days on MV | 16.3 (15.9)* | 5 (4.8)* | 0.0009 |
| Number of attempts of Intubation | 5.5 (5.02)* | 2.4 (1.5)* | 0.006 |
| Re-intubation | |||
| Yes | 24 (92.3%)& | 14 (51.8%)& | 0.002 |
| No | 2 (7.7%)& | 13 (48.1%)& | |
Student's t-test to compare hypothesis of quantitative. χ2 to compare hypothesis of qualitative variables, or Fisher's exact test in case one or more boxes had a value of<5. A p value of<0.05 was considered as statistically significant.
Correlation of risk factor with multiple complications (N=53).
| Variable | Number of complications | Correlation coefficient | p value |
|---|---|---|---|
| Surfactant doses | 0-3/0-3 | 0.305 | 0.04 |
| Intubation attempts | 1-18/0-3 | 0.454 | 0.001 |
| Birth weight | 560-4285/0-3 | -0.064 | 0.648 |
| Age at onset of MV (days) | 0-63/0-3 | 0.192 | 0.168 |
| Days with MV | 1-69/0-3 | 0.606 | 0.0001 |
MV, mechanical ventilation.
Spearman's correlation coefficient to define the association between two numerical valuables. Values between 0-1, positive correlation. Between -1 and 0, negative correlation; 0, no correlation. A p value<0.05 was considered statistically significant.
Risk associated with multiple complications in neonates with mechanical ventilation (N=53).
| Variable | With complications | Without complications | OR | CI 95% | p value |
|---|---|---|---|---|---|
| Gestational age | |||||
| <32 WGA | 6 | 15 | 2.8 | 0.682-11.4 | 0.135 |
| ≥ 32 WGA | 4 | 28 | |||
| Birth weight | |||||
| <1500 g | 4 | 15 | 1.24 | 0.3-5.1 | 0.5 |
| ≥ 1500 g | 6 | 28 | |||
| Nutritional status | |||||
| LWGA | 1 | 2 | 2.27 | 0.18-27.9 | 0.4 |
| AWGA | 9 | 41 | |||
| Gender | |||||
| Male | 3 | 23 | 0.37 | 0.08-1.6 | 0.23 |
| Female | 7 | 20 | |||
| Intubation attempts | |||||
| 1 | 9 | 33 | 2.72 | 0.3-24.2 | 0.66 |
| >1 | 1 | 10 | |||
| Surfactant doses | |||||
| 1-2 | 2 | 0 | NA | NA | 0.03 |
| >2 | 8 | 43 | |||
OR, odds ratio; CI 95%, 95% confidence interval. p value: <0.05 was considered statistically significant. NA, not applicable. OR requires a value greater than 0 to be calculated but the differences between groups was calculated using χ2. WGA, weeks of gestational age; LWGA, low weight for gestational age; AWGA, appropriate weight for gestational age.
The present study showed that 49.05% of the studied population developed pulmonary complications associated to MV, atelectasis being the most common. This corresponds to a less than expected rate, given that previous reports in similar populations have described greater frequencies of up to 150%8,9. An incidence rate of pulmonary complications associated with MV of 71.3 cases per 1000 days on ventilation are reported. In the bivariate analysis, it was observed that patients who developed complications had more days on mechanical ventilation (16.3 vs 5 days; p=0.0009). Also, the mean of intubation attempts was higher in this group (5.5 vs 2.4; p=0.006) and the proportion of patients with an intubation reattempt was greater in the group who presented complications (92.3% vs 51.8%; p=0.002). It is worth mentioning that residents are a considerable part of the medical staff and this decreases the probability of success of endotracheal intubation maneuvers.
Regarding surfactant dosing, it was shown that greater doses of surfactant were associated with a greater number of complications (Pearson 0.295; p=0.032), although there are articles reporting the utility of surfactant administration and a risk reduction in patients who receive it. In this case, the results were associated with the patient's conditions at delivery, given that the population consisted of patients of 26-28 gestational weeks, with significant lung immaturity. Other correlations that were established using the same method included a greater number of intubation attempts and a greater number of complications (0.616; p=0.0001). Similarly, it was observed that starting MV at a lower age increased complication episodes (-0.303; p=0.022). The days of MV correlated with the number of complications. Moreover, the administration of three doses of surfactant was identified as a risk factor to develop multiple complications, given that 100% of the patients that received three doses of surfactant presented more than one complication (p=0.03).
Previous publications over the past years in different countries have shown similar results. In 2014, Cernada et al. published a study conducted in Europe in neonatal population, which identified prematurity and the presence of reintubations as the main risk factors for ventilator-associated pneumonia. These data agree with the present results, in which the rate of ventilator-associated pneumonia was 19.6 per 1000 days of MV, which corresponds to that reported in developing countries8.
In a study published in 2007 by Lopez-Candiani et al., pulmonary complications presented with a frequency of 81%. Atelectasis was also found to be the most frequent complication. Their results showed more diversity since their population was studied prospectively. Nevertheless, regarding the most frequent complications, our results were similar.
In 2009, Tapia-Rombo et al.12 conducted a case-control study including 100 preterm newborns. When evaluating risk factors, they identified that a birth weight<1500g increased the risk of having a complication by three-fold (OR 3.2; p=0.01). We observed that the same risk factor had an OR of 1.24, although this finding was not statistically significant (p>0.05). Similarly, as for gestational age at birth, the study previously mentioned determined an OR of 7.25 for those<32 weeks. In this study, this estimator had a value consistent with increased risk (OR 2.8), but like the previous factor, it had a poor statistical significance (p=0.135). We recognize that this fact may be conditioned by a small study sample. We also found coincidences in prolonged duration of MV (mean 16.3 vs 5 days of MV; p=0.0009) and the increase in the frequency of reintubations (p=0.002)12 with the data reported by Tapia-Rombo et al.
Articles published in developed countries show no significant differences. Principi et al.13 reported a rate of 114 complications per 1000 days of ventilation in a population of pediatric patients in Canada, including newborns aged 1 day up to 18-year-old adolescents. Despite being a population with a wide range of ages, a prevalence of complications associated with ventilation of 40% was described and atelectasis was reported as the most frequent in 17% of the patients, which is very similar to the results reported for the population in our study.
It is important to highlight the limitations of our study since the main inconvenient present during the recollection of information from the clinical records was that it was absent or incomplete; moreover, given that this is a retrospective study, it is not possible to measure variables in real time; thus, a better analysis of these variables cannot be performed. It is recommendable that future studies evaluate the population in a prospective manner and give a real-time follow-up of their evolution during their hospital stay. This way, a better control of the variables of study could be achieved, and ventilation parameters and factors that cannot be evaluated in historical studies could be included.
To conclude, this study determined that the occurrence of pulmonary complications secondary to MV in neonate patients is similar to that reported in developing countries and that it has not varied significantly with time despite technological improvements in MV devices. These results highlight a great area of opportunity to establish strategies for continuous improvement and to be able to decrease, as far as possible, the number of complications associated with the use of MV in neonates.
The most statistically significant risk factor for the presentation of complications secondary to MV were the number of days on ventilation, number of intubation attempts and the number of doses of surfactant.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingResources from the Hospital General Regional No. 1, Instituto Mexicano del Seguro Social in Ciudad Obregón, Sonora, and from the authors.
Conflict of interestThe authors declare no conflict of interests of any nature.
To the directive personnel of the Neonatology Department, Clinical Archive and Health Documentation Center of Hospital General Regional No. 1, Instituto Mexicano del Seguro Social in Ciudad Obregón, Sonora, for the facilities provided for the elaboration of this manuscript.
Please cite this article as: Torres-Castro C, Valle-Leal J, Martínez-Limón AJ, Lastra-Jiménez Z, Delgado-Bojórquez LC. Complicaciones pulmonares asociadas a ventilación mecánica en el paciente neonatal. Bol Med Hosp Infant Mex. 2016;73:318–324.