Introducción: El síndrome de HELLP es un grave trastorno hipertensivo del embarazo con importantes problemas neonatales en los hijos de las madres afectadas. El objetivo de este trabajo fue conocer las características de estos neonatos y su evolución.
Métodos: Se llevó a cabo un estudio observacional descriptivo y retrospectivo de los neonatos hijos de madre con síndrome de HELLP, nacidos en un hospital universitario entre el 1 de enero de 2008 y el 31 de diciembre de 2013. Se estudiaron 33 neonatos procedentes de 28 gestaciones (cinco gemelares). Se realizó un análisis descriptivo y comparativo entre grupos, y posteriormente un análisis de multivarianza de factores asociados con la mortalidad dentro de la serie.
Resultados: De 33 recién nacidos estudiados (2.2/1,000 recién nacidos totales), dos fueron mortinatos (6.1% del total) y cuatro fallecieron tras el nacimiento (12.9% de los neonatos vivos), con una mortalidad perinatal total del 18.2%; 28 neonatos terminaron la gestación antes de la semana 37 (84.8%) y 11 antes de la semana 32 (33.3%); siete neonatos pesaron menos de 1,500 g (cuatro de ellos menos de 1,000 g). De los 31 recién nacidos vivos, 13 neonatos tenían peso menor al percentil 10 para su edad gestacional (41.9%), 20 precisaron reanimación neonatal (64.5%) y 14 presentaban leucopenia neonatal (45.2%). En la regresión logística final, la mortalidad neonatal se asoció con la gran prematuridad, independientemente del bajo peso, leucopenia o necesidad de reanimación neonatal.
Conclusiones: Los hijos de madre con síndrome de HELLP presentan elevada mortalidad asociada con la alta prematuridad, independientemente de la presencia de leucopenia, bajo peso para edad gestacional o necesidad de reanimación neonatal.
Background: HELLP syndrome is a serious hypertensive disorder of pregnancy with important neonatal problems in the newborn. The objective of this work was to determine the characteristics of these infants and its neonatal evolution.
Methods: A retrospective observational study of all newborns of mothers with HELLP syndrome born in a university hospital between January 1, 2008 and December 31, 2013 was carried out. Thirty-three infants from 28 pregnancies (five twin gestations) were studied. A descriptive and comparative analysis between groups and a multivariate analysis of factors associated with mortality in the series took place.
Results: Of 33 newborns studied (2.2 newborns/1,000 infants total), two were stillbirths (6.1% of the total) and four died after birth (12.9% of live neonates) with overall perinatal mortality of 18.2%. Pregnancies in 28 infants ended before 37 weeks (84.8%) and 11 pregnancies ended before week 32 (33.3%). Seven infants weighed <1500 g (four weighed <1000 g). Of the 31 live births, 13 infants were classified as <10th percentile weight for gestational age (41.9%), 20 needed neonatal resuscitation (64.5 %) and 14 had leukopenia at birth (45.2 %). In the final logistic regression, neonatal mortality was associated with extreme prematurity regardless of under-weight, leukopenia and/or need for neonatal resuscitation.
Conclusions: Children of mothers with HELLP syndrome have a high mortality associated with extreme prematurity, independent of the presence of leukopenia, low weight for gestational age and need for neonatal resuscitation.
1. Introduction
One of the most serious and frequent complications of pregnancy is the appearance of arterial hypertension in pregnant women. Preeclampsia (PE), eclampsia, and HELLP syndrome present as different stages of the same problem with important implications for the fetus and the newborn during various stages.1-3
HELLP syndrome is defined as a hypertensive disorder during pregnancy associated with microangiopathic hemolysis (Hemolysis), elevated liver enzymes (Elevated Liver) and thrombocytopenia (Low Platelets). Although not exclusive to severe forms of PE and eclampsia, it is often associated with these conditions. Its exact patho-physiological mechanism remains unknown, although it is known that in its presence there is an invasion of abnormal trophoblasts, a misadaptation of platelet function and a generalized alteration of the maternal vascular system.1,4
PE, eclampsia, and HELLP syndrome pose a major problem during gestational progression in which pregnancy termination is necessary in a high percentage of cases.5 The problem of prematurity, which is caused by the urgent need to terminate the pregnancy, can cause other neonatal problems such as low weight and the frequent presence of leukopenia at birth.
This article reports the retrospective review of the cases of children born to mothers with HELLP syndrome diagnosed in the Hospital Universitario Central de Asturias (HUCA) in the last 6 years. With the goal to determine the characteristics of these infants and their vital prognosis, assessing the role of prematurity, low birth weight for gestational age, and leukopenia.
2. Methods
A descriptive and retrospective study was conducted in infants born to mothers with HELLP syndrome. They were born in a university hospital, Hospital Universitario Central de Asturias (HUCA), with level III neonatal care, between January 1, 2008 and December 31, 2013.
Cases were actively sought between pregnancies/births associated with hypertension in the HUCA from discharges. From the initial list, clinical records of those mothers who met the diagnosis of HELLP syndrome were investigated (elevated mean maternal arterial pressure, hemolysis, abnormal liver tests and low platelets) to finally obtain the information from their children.
The newborn’s records were reviewed in order to complete the protocol to retrieve data of the pregnancy, childbirth, and subsequent evolution. Specifically, the presence of leukopenia (total blood leukocytes <10,000), neutropenia (total blood neutrophils <1,500), and thrombocytopenia (total blood platelets <150,000) were found in the first blood analysis (at birth). To calculate weight for gestational age, Fenton6 charts were used, defining underweight as <10th percentile for gestational age.
The study was conducted to meet the requirements of strict confidentiality in data handling, following at all times the guidelines of the Research Ethics Committee of HUCA. Data were captured using statistical software (SPSS
v.18.0 with license) in order to conduct the statistical analysis. First, a descriptive analysis was performed with frequencies for qualitative variables and means, 95% confidence intervals, medians and ranges for quantitative variables. Subsequently, comparisons were made by groups using the Student t test if the variables and the X2 test were quantitative; then qualitative variables were compared. Finally, logistic regression was performed to study the influence of the most important variables related to mortality. Statistical significance was established with p = 0.05.
3. Results
During the 6-year study period, 15,161 births were recorded at HUCA; 33 were children born to 28 mothers with HELLP syndrome (23 children from single pregnancies and 10 children from twin pregnancies), which is a frequency of 2.2 newborns/1,000 total newborns. The average age of the mothers at the time of delivery was 34.7 years (95% CI 32.6−36.8 years) with a median of 35 years and a range between 19 and 45 years. Five of the mothers were <30 years of age and four mothers were >40 years of age. Seventeen mothers (60.7%) had single pregnancies and five of the mothers (17.8%) had twins.
The average gestational age at birth was 32.6 weeks of gestation (WG) (95% CI 31.0−34.1 WG), with a median of 33 WG and a range of 24−39 WG. Twenty-eight infants were born before 37 WG (84.8%), one before 32 WG (33.3%), and four before 28 WG (12.1%). Of the 28 pregnancies, 23 ended with cesarean section (82.1%). Six pregnancies were induced by different fertilization techniques. Two infants were stillborn (6%), a male of 24 WG and a female of 26 WG.
The average birth weight of the 31 live births was 1,809 g (95% CI 1,559−2,059 g) with a median of 1,900 g and a range of 410−3,545 g. Seven infants weighed <1,500 g (four of them <1000 g), and four infants weighed >2,500 g. Thirteen infants had a weight <10th percentile for gestational age (41.9%). Of the 31 infants, 18 (58.1%) were males.
Among the live births, 20 infants (64.5%) received some type of resuscitation (six required intubation at birth), 27 were admitted to the neonatal unit (87.1%) and 14 were in intensive care (45.2%). At birth, 14 infants (45.2%) had blood leukocytes <10,000, four had neutrophils <1,500, and six had platelet counts <150,000 (three had platelets <100,000). No statistically significant association was found between leukopenia and low weight for gestational age (LWGA).
After birth, 11 infants had respiratory distress, one had vertical clinical sepsis with negative blood cultures, five had nosocomial sepsis (two with S. epidermidis, two with Klebsiella pneumonia, and one with S. capitis), two had periventricular hemorrhage (both were grade II), and two had necrotizing enterocolitis (grade III or higher).
Of the 33 infants with HELLP syndrome, two were stillborn (6.1% of the total) and four died after birth (12.9% of the live births), representing an overall perinatal mortality of 18.2%.
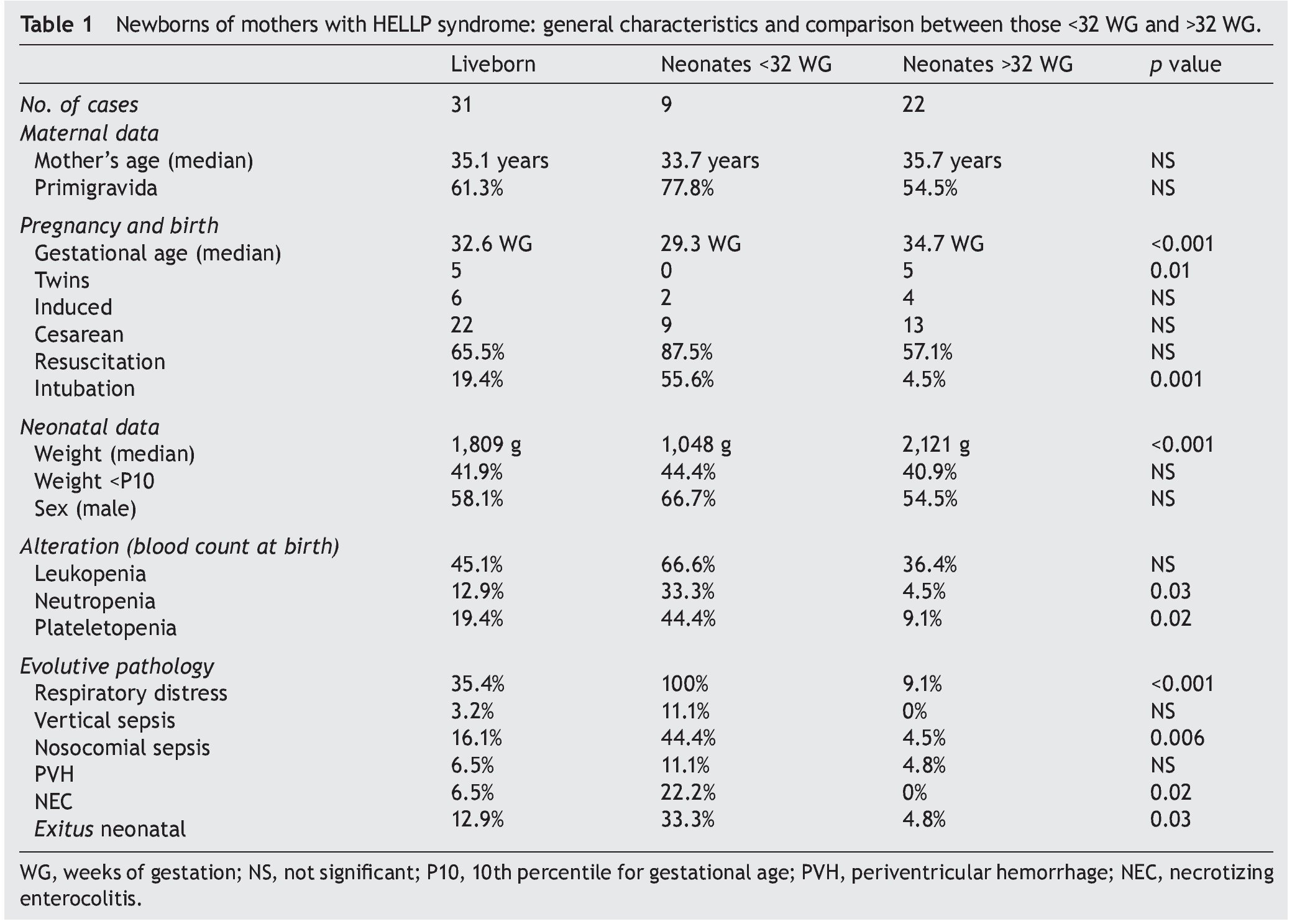
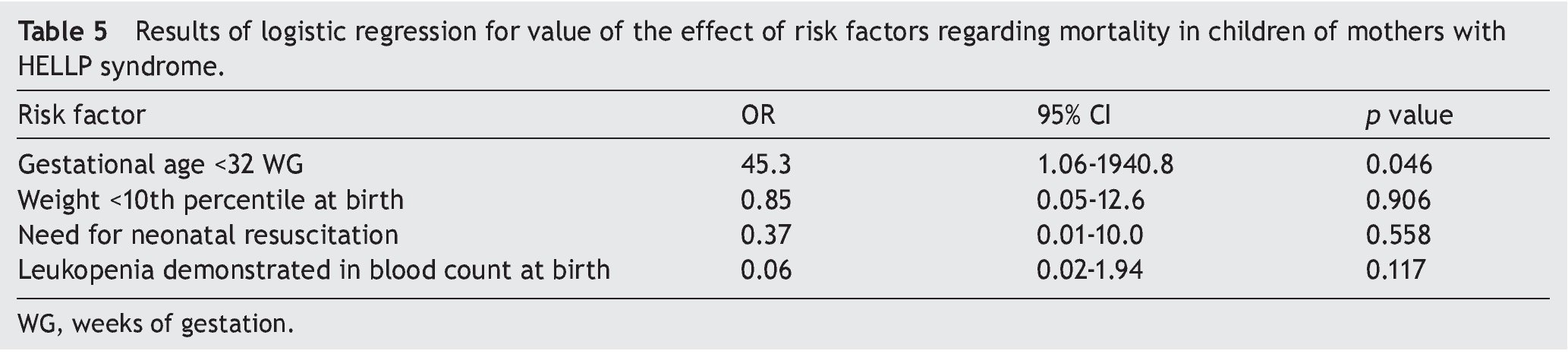
Table 1 shows the main characteristics of the study and the comparison for gestational age (less than or greater than 32 WG). All evolutionary complications were more common in those born before 32 weeks, making respiratory distress, nosocomial sepsis, necrotizing enterocolitis, and mortality statistically significant.
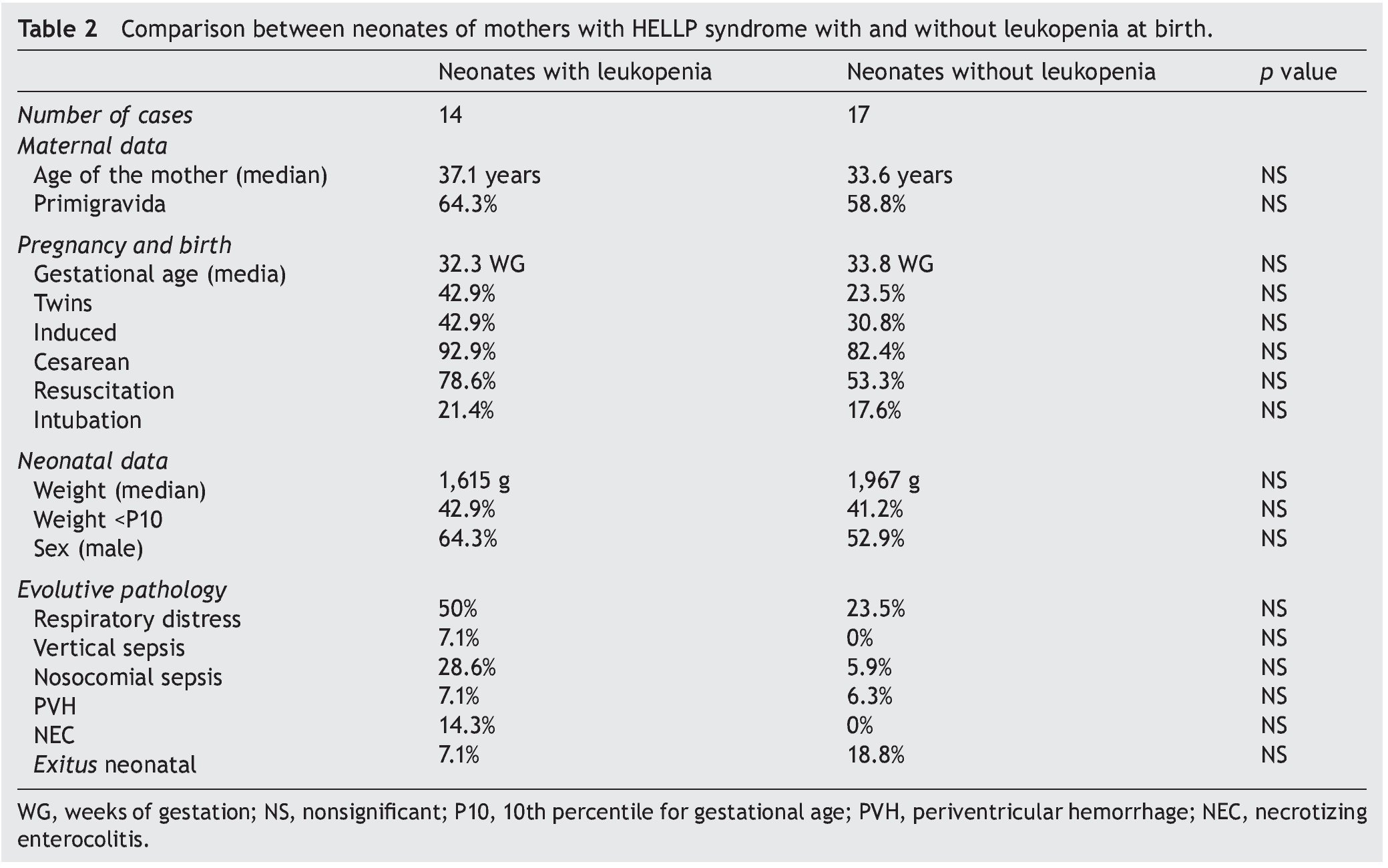
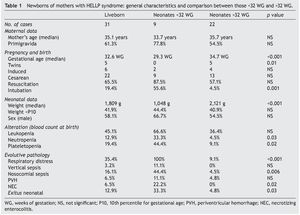
Table 2 shows the comparison between infants with and without leukopenia regarding risk factors and consequences. No statistically significant differences were found between groups.
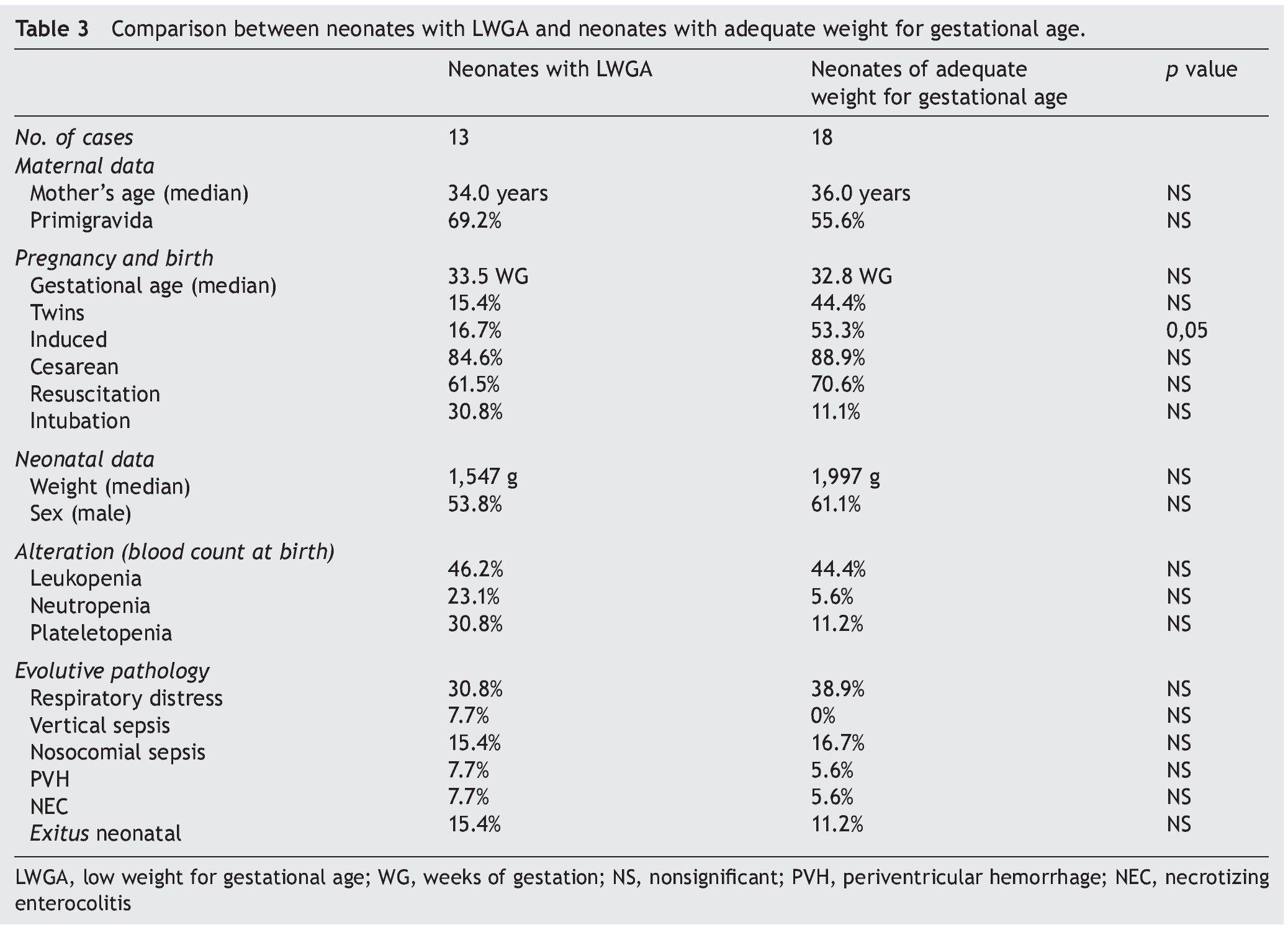
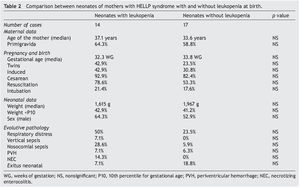
Table 3 compares infants with low birth weight for gestational age and those of appropriate weight. We found a higher percentage of cases from induced birth in the group of newborns with appropriate weight for gestational age.
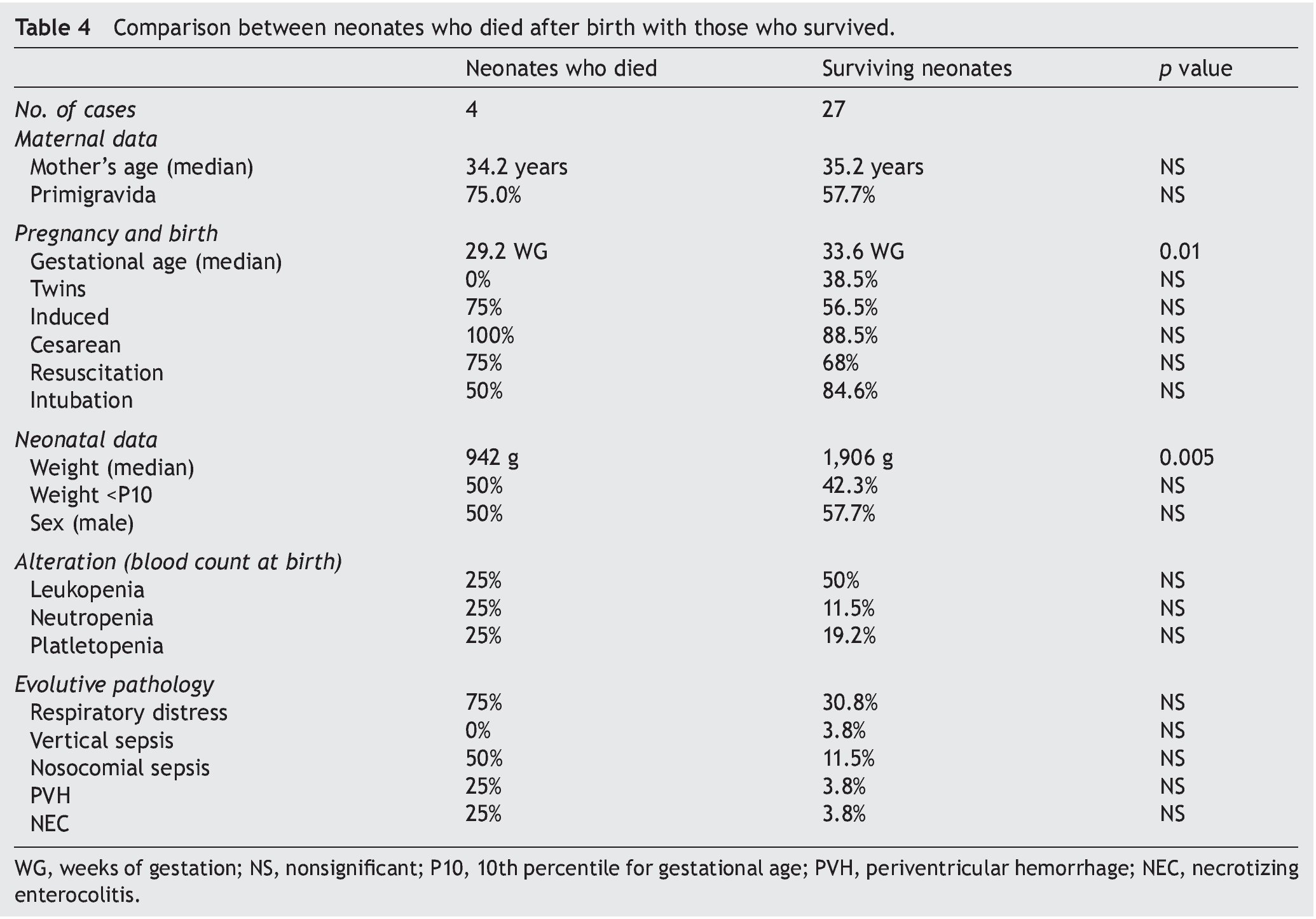
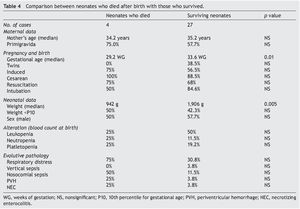
Table 4 compares liveborn infants who died and those who survived. Statistically significant differences were found between groups according to gestational age and birth weight.
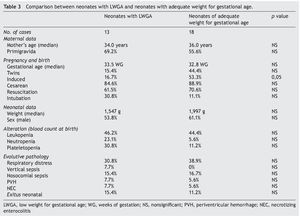
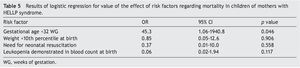
Table 5 shows the results of logistic regression performed with the predictors of “significant prematurity”, “leukopenia”, “low weight for gestational age”, and “need for resuscitation” for the dependent variable “exitus”. The only variable that has a statistically significant influence on mortality, independently of the others, is the high percentage of prematurity.
4. Discussion
Children of mothers with HELLP syndrome who were born at HUCA during a 6-year period had a high rate of mortality associated with extreme prematurity and, independent of the presence of leukopenia, LWGA or necessity for resuscitation at birth.
Induced prematurity is a consequence of definitive treatment of severe cases of pregnancy-induced hypertension. Pregnancy termination is the ultimate solution to maternal problems in most cases, but the effects on the neonate as a result of this decision may present a high cost.
Although the prognosis of preterm births has much improved in the last 20 years, especially in developing countries, birth before 32 WG still has important consequences. NICUs are a very imperfect substitute for the womb, and the problem is greater with a younger gestational age at the time of birth, reaching important ethical problems when approaching the “gray area” of periviable births (between 22 and 26 WG).7-9 However, as already published in numerous papers, late preterm infants have not been spared from associated morbidity and mortality.10,11
One of the most discussed points in this issue is whether premature infants of mothers with PE, eclampsia, or HELLP syndrome present a poorer prognosis than preterm infants of mothers without these conditions. The study presents widely varying and sometimes contradictory data. Perhaps premature offspring of affected mothers could have a better discreet prognosis than their peers whose mothers were not affected. The opposite occurs in late preterm births.2,12
In this study, a neonatal mortality rate of 12.9% was obtained, a figure well above the expected estimate. For this reason, the possible role of other factors in this poor prognosis was raised—prematurity, low birth weight for gestational age and leukopenia.
In addition to this induced prematurity, children of mothers with PE, especially in its most serious forms such as HELLP syndrome, are predisposed to present LWGA as a result of intrauterine growth retardation. LWGA has been linked to metabolic disease in the medium and long term, partly explained by the classic Barker hypothesis,2,13,14 but other short-term problems may ensue. For example, it may be directly related to the emergence of alterations in blood count of the newborn at birth and, in particular, with the development of leukopenia.
The results of this univariate analysis ruled out that leukopenia or LWGA influenced mortality, but the authors decided to confirm using linear regression through a multivariate analysis to rule out possible confounding effects. In the initial model they introduced data of infants <32 WG with LWGA, leukopenia and the need for neonatal resuscitation because the vitality at birth could confuse or interact with the other three introduced variables. However, as noted in the results, only the high degree of prematurity (being born before 32 weeks WG) was a statistically significant factor associated with mortality.
In conclusion, in this study of children of mothers with HELLP syndrome, a poor short-term prognosis with high mortality (12.9%) is demonstrated, which is related to the high incidence of prematurity but not with LWGA, leukopenia, or need for neonatal resuscitation at birth.
Ethical disclosure
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Funding
None.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 3 September 2015;
accepted 18 September 2015
☆ Please cite this article as: González Álvarez CE, González García LG, Carrera García L, Díaz Zabala M, Suárez Rodríguez M, Arias Llorente RP, et al. Hijo de madre con síndrome de HELLP: características y papel de la prematuridad, bajo peso y leucopenia en su evolución. Bol Med Hosp Infant Mex. 2015. http://dx.doi.org/10.1016/j.bmhimx.2015.09.006
* Corresponding author.
E-mail:gsolis@telefonica.net (G. Solís Sánchez).