1. Summary of the clinical history (A-13-08)
We present the case of a 13-year-old female patient with productive cough, weight loss and skin lesions.
1.1. Hereditary family history
The patient’s mother is 50 years of age and the father 51 years of age. There are seven siblings, six apparently healthy. One received treatment for tuberculosis (TB) for 1 year. The latest smear was negative.
1.2. Personal social history
The patient lived in a home with all services with a bedroom shared by four persons. The family cooks with wood. There are no pets living in the home.
IMMUNIZATIONS
Immunizations were as follows: BCG dose at 2 months of age, six doses of Sabin, three doses of pentavalent, two doses of DPT, one dose of triple viral.
1.3. Perinatal and disease history
The patient was the product of a seventh pregnancy without prenatal monitoring, folic acid or iron intake during pregnancy. Labor was assisted by a midwife. The infant cried and breathed at birth. No perinatal complications were reported.
1.4. Current illness
The patient’s illness began in December 2012 with a productive cough and yellowish-green non-bloody expectorate.
Dysphonia was added (1½ months before admission), dysphagia (first to solids and later to fluids), and weight loss of unspecified amount (of 1 month evolution). The patient also presented skin lesions with dry skin with evidence of scratching (1 week evolution.)
PHYSICAL EXAMINATION
Physical examination revealed weight 29.3 kg, height 147 cm, cardiac frequency 110/min, respiratory frequency 28/ min, blood pressure 81/48 mmHg, temperature 35.5°C, head circumference 54 cm, abdominal circumference 65 cm.
GENERAL EXAMINATION
The patient demonstrated adequate hydration. She was cachectic with pale, generalized dry skin with desquamation and signs of scratching.
HEAD AND NECK
There was adenomegaly of firm consistency in the superior chain and posterior neck (1-1.5 cm).
CHEST
With preserved respiratory excursions, pulmonary fields with bibasal hypoventilation and crepitant rales.
ABDOMEN
Soft, not painful to touch, without organomegaly.
EXTERNAL GENITALIA
Without alteration.
EXTREMITIES
Hypotrophic, adenomegaly of 0.5 to 1 cm in the axilla and groin.
February 15, 2013
Several hours after admission the patient presented abdominal pain in the right flank and mesogastrium. Plain chest x-ray showed pulmonary parenchyma with bilateral micronodular infiltrate predominantly in the left base with a rounded, thin-walled image at the apex (3.6 cm) with presence of air as well as subdiaphragmatic free fluid.
Exploratory laparotomy was carried out for the diagnosis of intestinal perforation. Abundant intraperitoneal fluid was found with scant biliary material and perforation of the ileocecal valve at 55 cm, which was closed. Ischemic lesions were noted, each of ~10 cm, in the entire small intestine, from 140 cm to the angle of Trietz. The intestine was resected from this point and an ileostomy of two openings was done. Antibiotic coverage was provided with amikacin and metronidazole. The patient presented hemodynamic instability and bleeding at the sites of the stoma and also as a result of the orogastric tube. Infusion with norepinephrine was started and platelets were transfused.
February 18, 2013
Dermatological diagnosis was nutritional dermatosis and probable pellagra.
February 19, 2013
Rifampin, isoniazid, pyrazinamide and ethambutol were begun.
February 21, 2013
The patient presented tachypnea and bibasal hypoventilation. X-ray showed right pleural effusion for which steroids were indicated and pleural tube was placed.
February 26, 2013
The patient had epistaxis and surgical wound dehiscence with purulent material from the wound. Septic shock was present and mechanical ventilation was started. Complication of pneumothorax was demonstrated and the patient was admitted to the ICU.
March 3, 2013
The patient was weaned from ventilatory support. Persistence of intraabdominal purulent fluid noted in the drains and on tomography. The patient was managed conservatively.
March 8, 2013
The patient had septic shock and pleural effusion. Mechanical ventilation was reinitiated. Diagnostic thoracentesis was done with output of 390 mL of rust-colored material. The patient suffered cardiorespiratory arrest and did not respond to resuscitation maneuvers.
LABORATORY RESULTS
Blood count was as follows: hemoglobin 11.6 g/dl, hematocrit 33.8%, leukocytes 4100, bands 8%, segments 58%, monocytes 11%, platelets 99,000. Coagulation time: PT 15.7”, PTT 31.4”. Blood chemistry: glucose 100 mg/dl, BUN 34 mg/dl, creatinine 1.1 mg/dl, uric acid 4.3 mg/dl, Na 133 mEq/l, K 3.7mEq/l, Cl 100 mEq/l, Ca 6.9 mg/dl, P 4.3 mg/dl. Bilirubins: direct 0.6 mg/dl, indirect 0.26 mg/dl, total 0.32 mg/dl, FA 501 U, ALT 38 U, AST 26 U, LDH 503 U, albumin 4.4 g/dl.
2. Case presentation
2.1. Pediatrician (Dra. Ana Victoria Villareal)
We discuss the case of a 13-year-old adolescent from a rural community in the State of Mexico. She lived in crowded conditions and had a brother with TB who was treated for 1 year. The patient was malnourished with inadequate nutritional intake and incomplete vaccination status. The following syndromatic diagnoses were made:
1. Respiratory infection syndrome: due to the presence of cough, dysphonia and tachypnea.
2. Constitutional syndrome: characterized by unquantified weight loss with 40% weight deficit for age, anemia, anorexia and cachexia with body mass index of 13.5, height for age 90%, and weight for height 76%.
3. Acute abdominal syndrome: due to the presence of abdominal pain and findings of bilateral subdiaphragmatic air on chest x-ray.
4. Systemic inflammatory response syndrome: due to the presence of hypothermia, tachycardia, tachypnea and leukopenia.
With the support of the syndromatic diagnoses and patient evolution, the following nosological diagnoses were made:
1. Miliary TB: based on the epidemiological background and the presence of respiratory infection syndrome, constitutional syndrome, nephritic syndrome, systemic inflammatory response syndrome, lymphadenopathy, pulmonary radiological findings, acute abdomen with intestinal perforation and granulomas positive for Ziehl-Neelsen stain.
2. Septic shock: based on the systemic inflammatory response syndrome, hypotension (with mean arterial pressure of 56 mmHg), and hematological dysfunction.
3. Severe acute chronic malnutrition: based on constitutional syndrome, with weight for age of 60%.
The patient had more than one risk factor for developing TB on admission. The one risk with the greatest relevance is the history of contact with her brother, apparently bacilliferous, who received unspecified treatment. The Guide for the Care of Tuberculosis in Children and Adolescents in Mexico, published in 2012 and part of the National Tuberculosis Program, recommended strict monitoring of contacts of patients diagnosed with TB as well as the application of the purified protein derivative (PPD) or tuberculin skin test (TST) for detection of latent TB in those who have had contact with the treated patient. This was not done in this case. The patient was immunocompromised and lived in crowded conditions, factors that are also indicators for strict follow-up.
TB is a public health problem at a global scale. WHO estimates that a third of the worlds’ population is infected by Mycobacterium tuberculosis. Between 5 and 10% of the persons infected will have symptoms throughout their lifetime. In Mexico, the reported prevalence of TB is 3.7 cases/100,000 inhabitants, of which 10% belong to the pediatric population.
Within the patient’s history, there is a report of a BCG vaccination 2 months later than that indicated by the National Immunization System. The effectiveness of this vaccine of live attenuated Mycobacterium bovis bacilli in severe forms (miliary and meningeal TB) varies in children between 60% and 80%. A meta-analysis of randomized and controlled cases published in 2006 demonstrated that the average effectiveness against tuberculous meningitis and disseminated TB was from 86%. The corresponding figure obtained in studies of cases and witnesses was 75%. In Saudi Arabia, a 20-year follow-up was carried out of individuals vaccinated with BCG during the neonatal period and the protective effectiveness against pulmonary, meningeal or disseminated TB was determined to be from 82% in children < 15 years of age, 67% in the age group from 15-24 years of age, and from 20% in persons 25-34 years of age.
In regard to the nutritional status of the patient, it is known that she was in a state of severe acute chronic malnutrition that led to an important immunocompromise and favored the bacillary multiplication by altering the cellular immune function, which is essential for protection against mycobacteria. In Mexico in 2005, 11.1% of the TB cases were associated with the presence of some degree of malnutrition, with 47% mortality in patients with both diseases. Patients who are immunocompromised have a greater predisposition for manifesting extrathoracic and disseminated forms, as in this case.
Treatment should be initiated once the diagnostic suspicion is made, even without confirmatory tests. In this patient there was a 5-day delay in treatment. Treatment delay is associated with greater mortality. The scheme recommended by the WHO and the Infectious Disease Committee for the treatment of disseminated TB is the same as for tuberculous meningitis due to the high probability of dissemination through blood. Treatment is recommended for 2 months with isoniazid, rifampin, pyrazinamide and streptomycin during the intensive phase and for a period of 4 to 10 months with isoniazid and rifampin in the consolidation phase. Streptomycin should be included because of its greater ability to penetrate the blood-brain barrier compared with ethambutol, even without the presence of meningeal involvement.
There are no studies that demonstrate the effectiveness of steroid treatment in cases of disseminated TB in children. WHO recommends its use only in cases of confirmed TB meningitis at a dose of 2 mg/kg/day for 4 weeks.
Miliary TB may present hematological dissemination to the CNS in 70% of cases. In the event that the diagnosis is suspected, CT scan of the brain is indicated in order to rule out the presence of characteristic lesions in a timely fashion, such as hydrocephalus due to basal obstruction of the ventricular system, leptomeningeal thickening and arachnoiditis.
The condition of the apical lobe of the left lung observed on the patient’s admission allows for the suspicion of lymphatic dissemination via the thoracic duct arising from the lymphatic transport of the intestinal trunk, suggesting the gastrointestinal tract as the primary focus of infection. The patient should have received fluids due to dehydration with hemodynamic alteration at the start, as well as early initiation of antibiotics because of the presence of severe sepsis. Timely administration of crystalloids and the early initiation of antibiotics achieve a decrease in absolute mortality of 15.9 and 17.7% at 28 days.
After intestinal resection, an antibiotic scheme with gram-negative coverage, enterococcus, enterobacteria and anaerobes was initiated, suitable for the usual flora in an intestinal perforation. The guide for prophylaxis in surgical procedures in this institution reports an infection rate from 30-40% in contaminated surgeries due to visceral perforation.
Systemic inflammatory response persisted in the patient. An infection due to opportunistic germs was suspected as well as infection of the surgical wound. The patient showed no improvement despite receiving coverage with broad spectrum antibiotics. Regarding hemodynamic and ventilatory issues, prompt removal of non-invasive ventilation was achieved as well as removal of aminergic support and initiation of enteral route.
The patient had ventilatory and hemodynamic deterioration with a high probability of death due to the presence of factors such as leukopenia on admission of < 5000, severe malnutrition, superinfection by opportunistic germs, late initiation of antituberculous treatment, and the degree of systemic involvement by Mycobacterium. Septicemia caused development of acute respiratory distress syndrome. This finally led to multiple organ failure with mortality reported up to 100%.
The final clinical diagnoses are listed below:
1. Miliary TB with pulmonary, intestinal and renal involvement, with granulomatous lesion and necrosis that also affected the central nervous system, liver and heart
2. Severe chronic malnutrition
3. Postoperative status for intestinal resection due to perforation
4. Surgical wound infection
5. Septic shock
6. Acute respiratory distress syndrome
7. Multiorgan failure
2.2. Imaging (Dra. Pilar Dies)
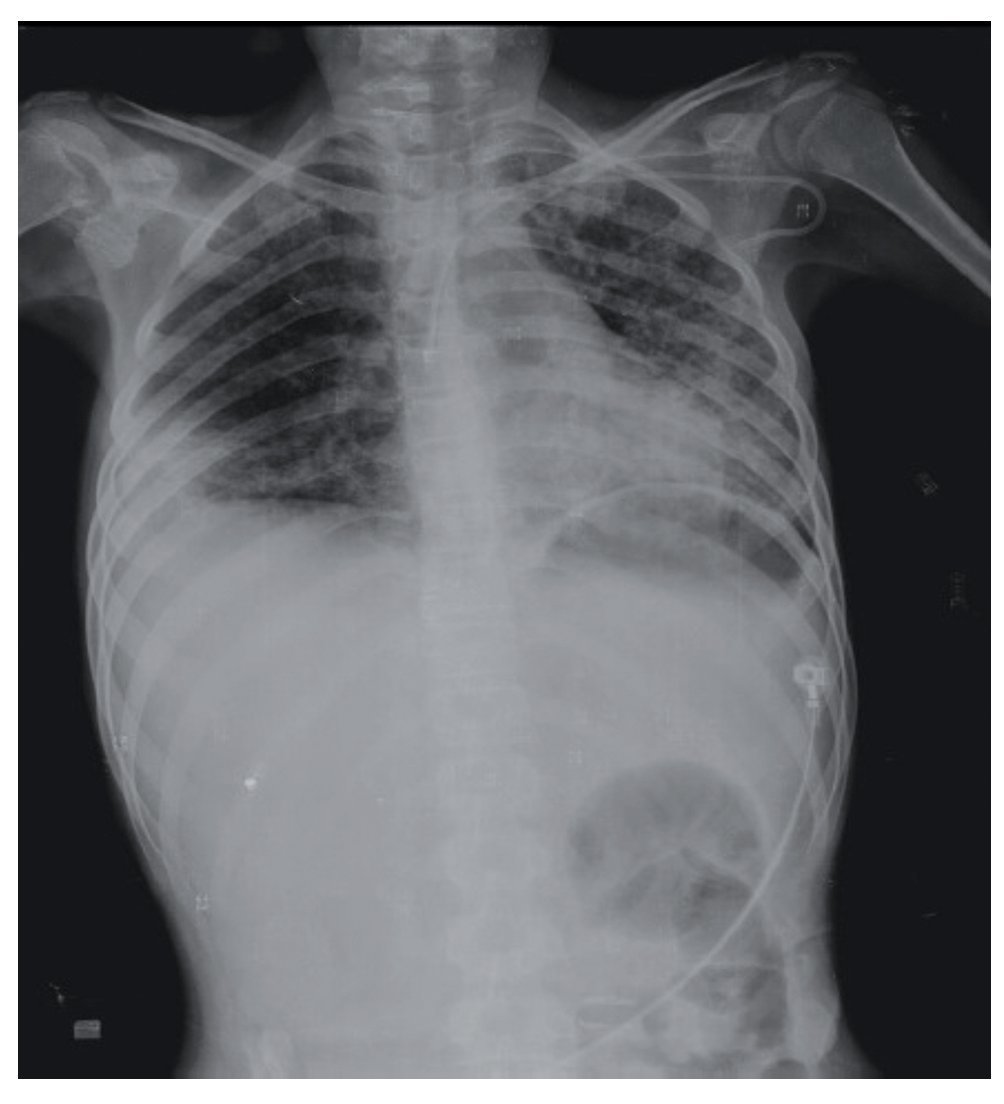
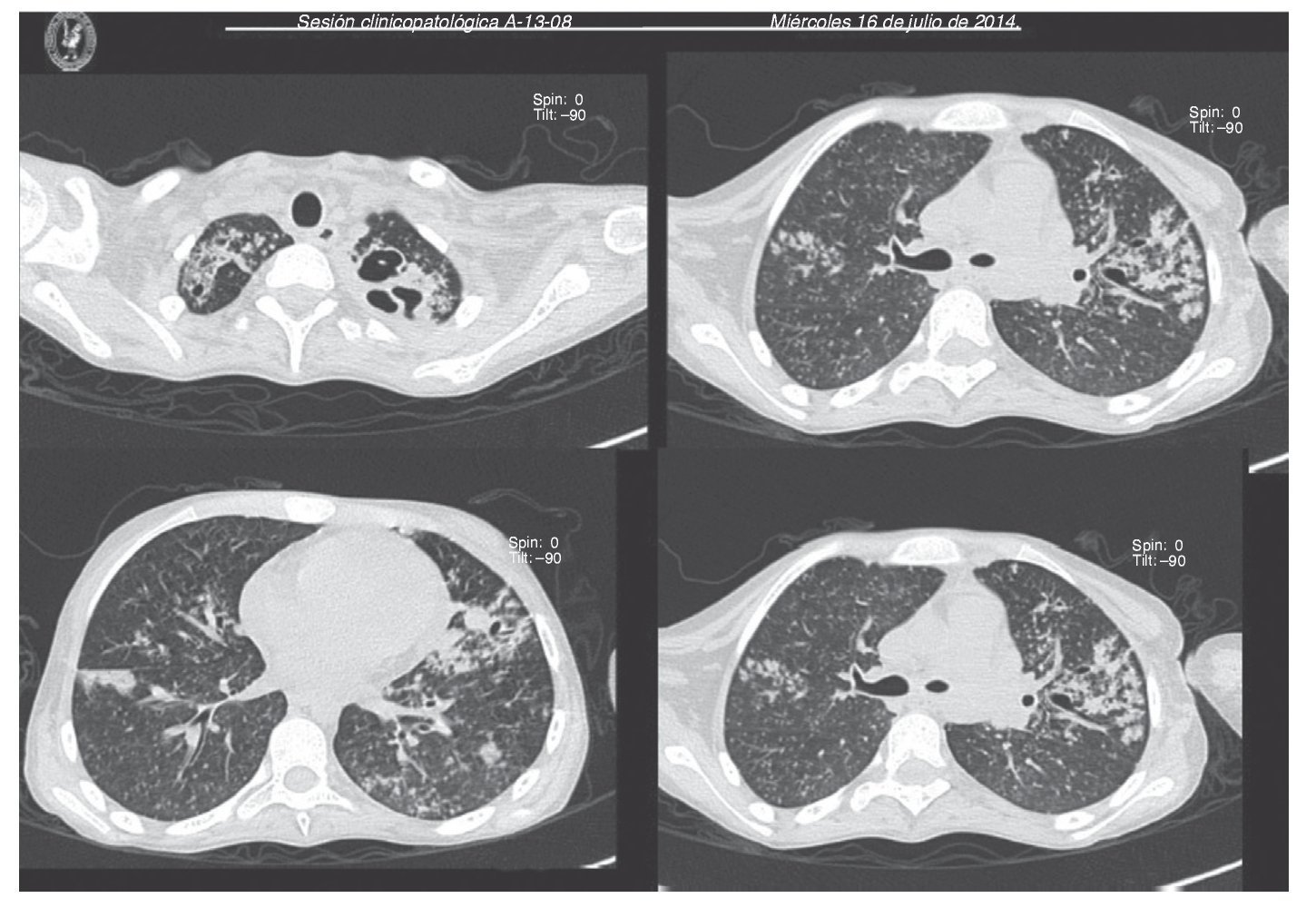
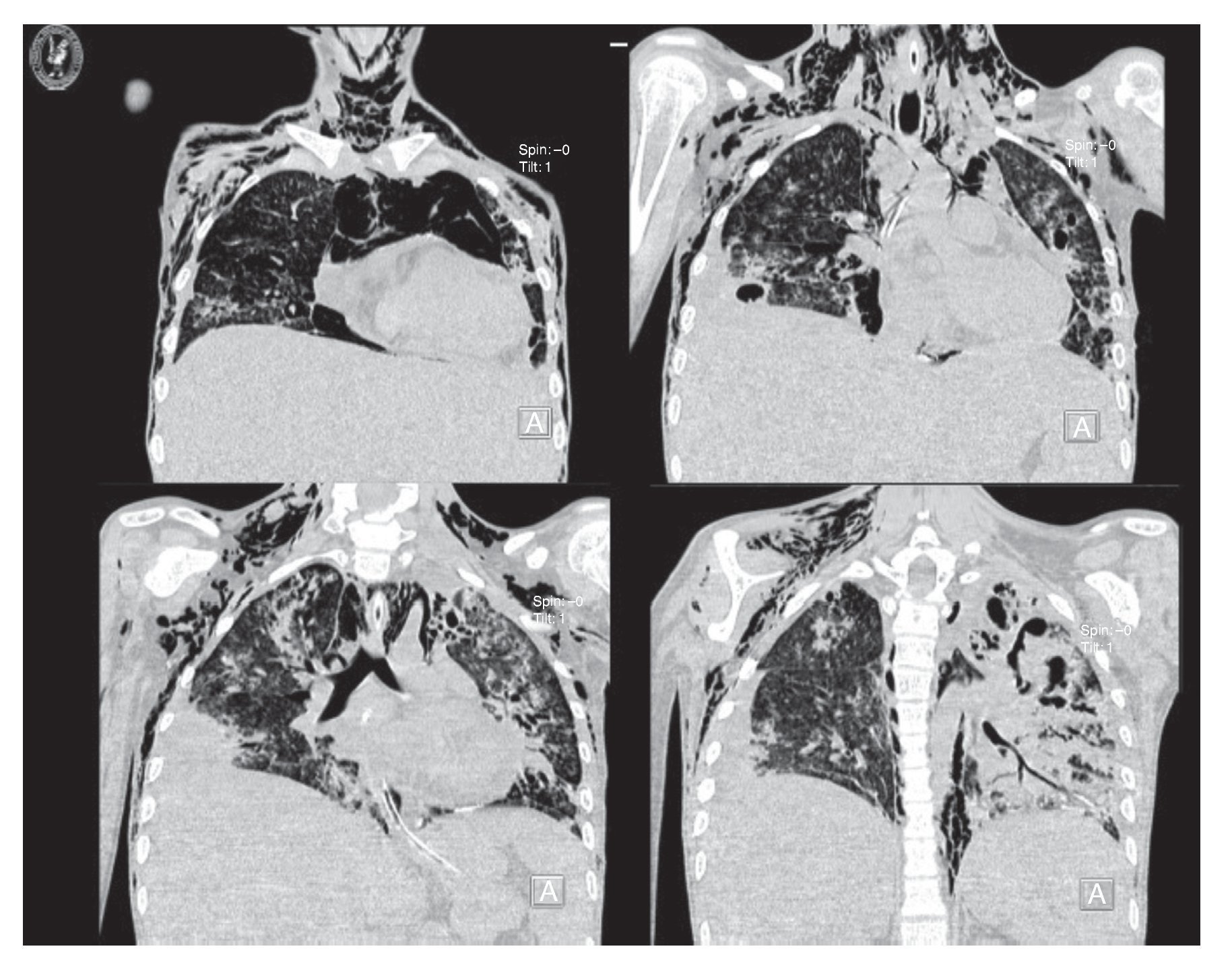
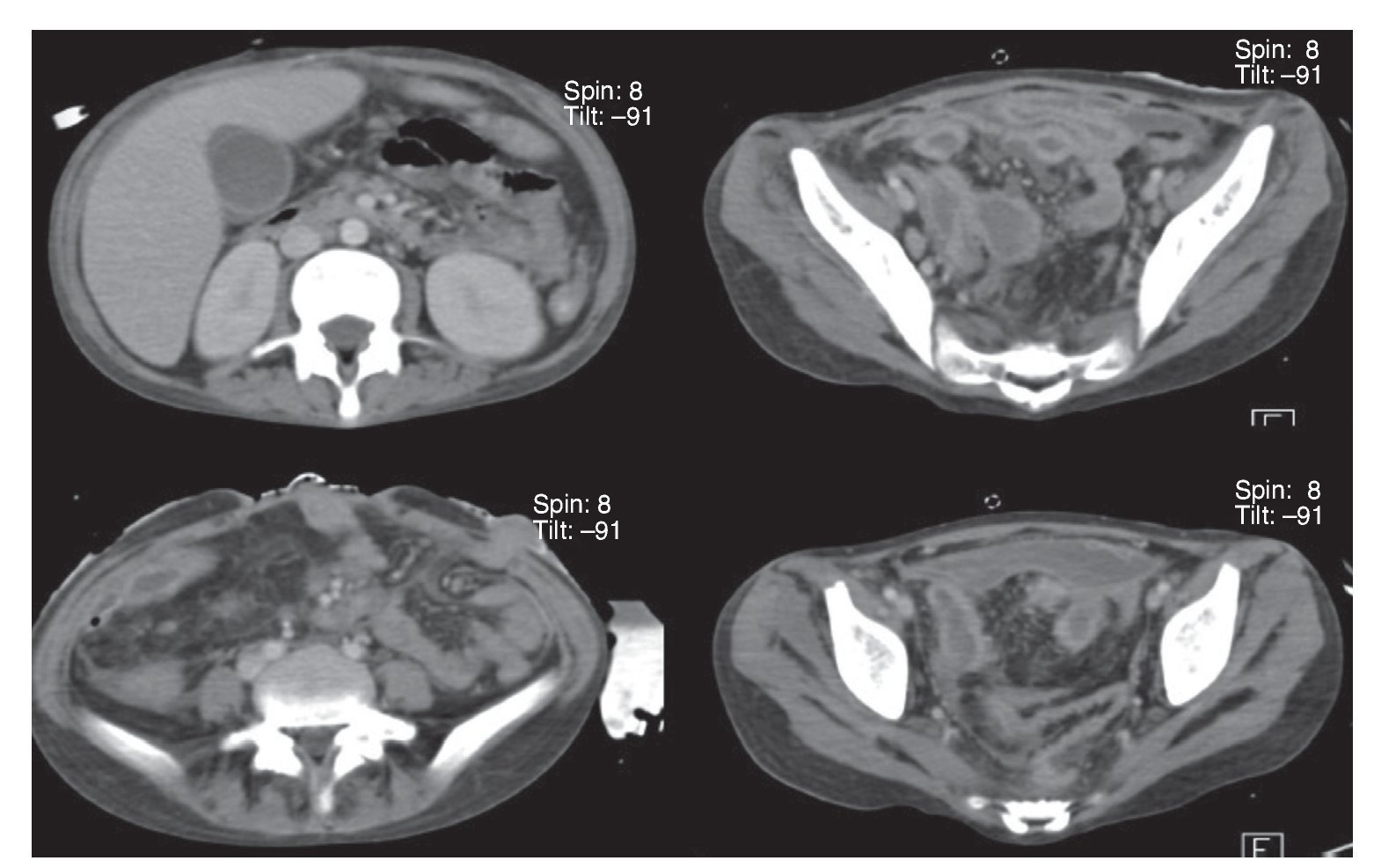
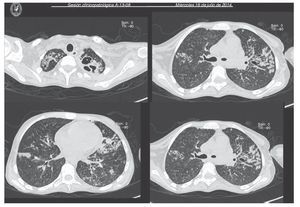
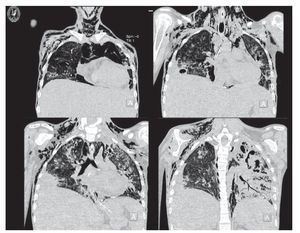
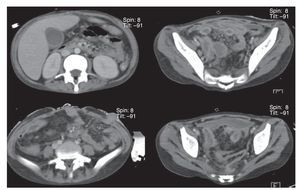
Chest x-ray demonstrated radiolucent images, predominantly towards the left apex (Figure 1). Lung CT scan with windows shows caverns in segments I and II and areas of consolidation and caverns predominantly in the posterior segments. There is an area of lung consolidation with areas of discrete thickening of the bronchi and acinar opacity (Figure 2). CT of the mediastinum shows dissection due to gas through the muscular mass and predominantly in the region of the neck, at the level of the chest, and with axillary predominance. In the lower segments it was observed how the air practically draws the entire tract of the aorta. There is pleural effusion, predominantly on the right side, and the liver is shown to be increased in size (Figure 3). In the mid-region there is diastasis of the rectus and changes due to the ileostomy (Figure 4).
Figure 1 Chest x-ray confirming the presence of a bilateral diffuse micronodular infiltrate with right basal pachypleuritis, bilateral axillary lymph nodes growths and hepatomegaly with abnormal distribution pattern of intestinal gas.
Figure 2 Computed tomography (CT) images (axial cuts) of the chest of the apical and parahilar regions showing bilateral diffuse nodular pattern in both pulmonary fields with peribronchial and alveolar thickening (image of budding tree), with left perihilar bronchiectasis and areas of apical cavitation of left predominance.
Figure 3 CT window images for pulmonary parenchyma that show evolution of the nodular lesions with increase in alveolar and peribronchial thickness with rupture of the alveolar structures that causes subcutaneous emphysema on the chest wall and cervical region bilaterally.
Figure 4 Axial cuts of abdominal CT showing perivesicular areas of fluid with diffuse, generalized thickening of the intestinal wall and postsurgical changes in the abdominal wall.
3. Discussion
3.1. Diagnostic ancillary services (Dra. Briceida López)
Real time RT-PCR was used to confirm the presence of Mycobacterium tuberculosis and the absence of genes resistant to rifampicin. The technology with which this test is done has a sensitivity and specificity of > 97%. It is a methodology recommended by the WHO since 2013 for countries such as Mexico as it does not require a level 3 laboratory to rapidly identify this type of microorganism. Among the advantages of this equipment is the speed with which the procedure is carried out and that the sample may be obtained from expectoration, lymphatic fluid or cerebrospinal fluid. RT-PCR substantially reduces the time for results (3-4 h) compared with the 6 weeks required for a culture.
4. Pathology (Dr. Guillermo Ramón García)
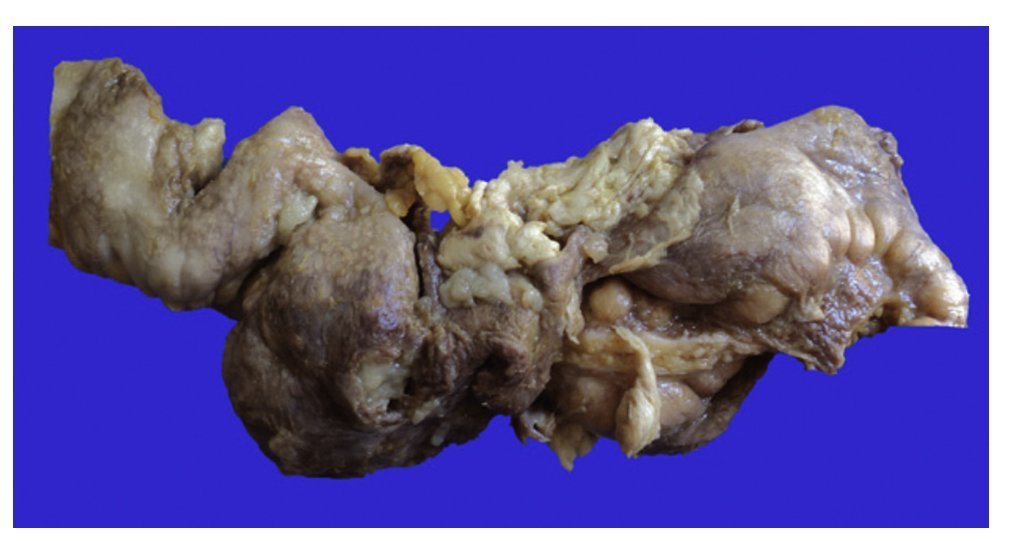
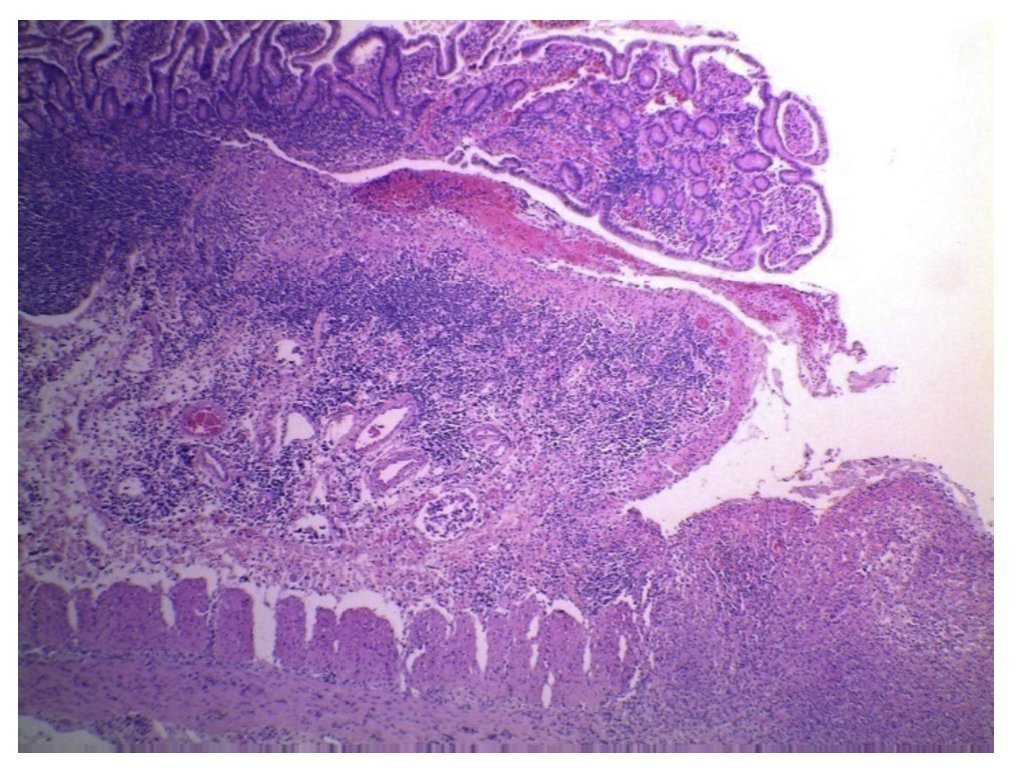
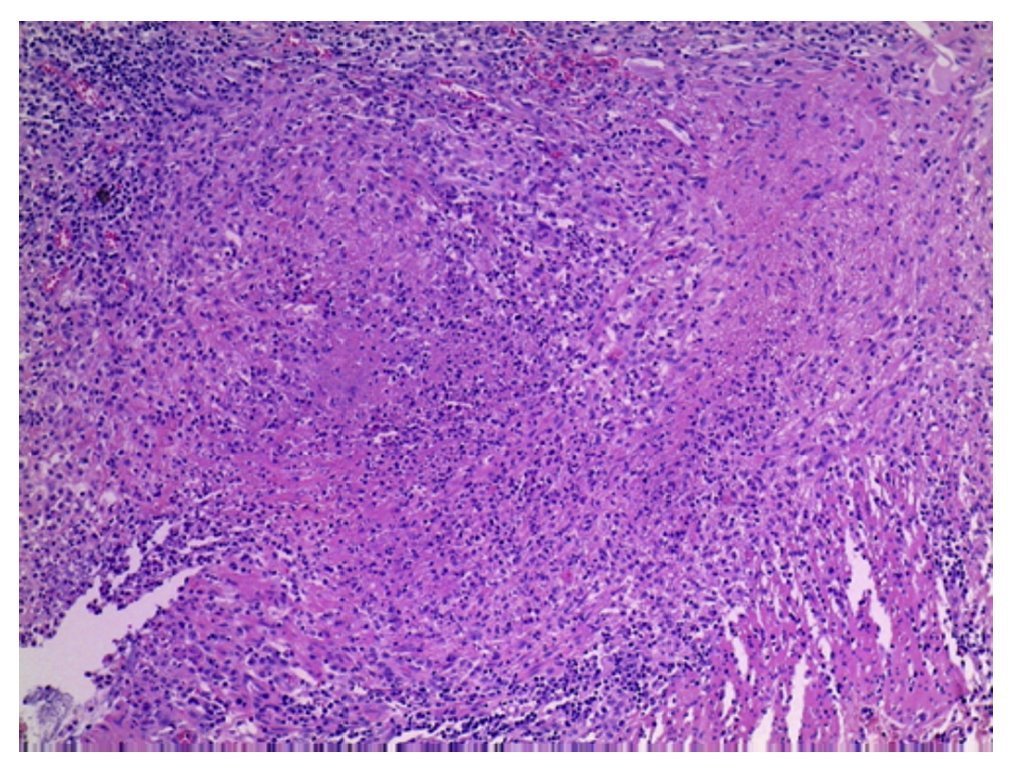
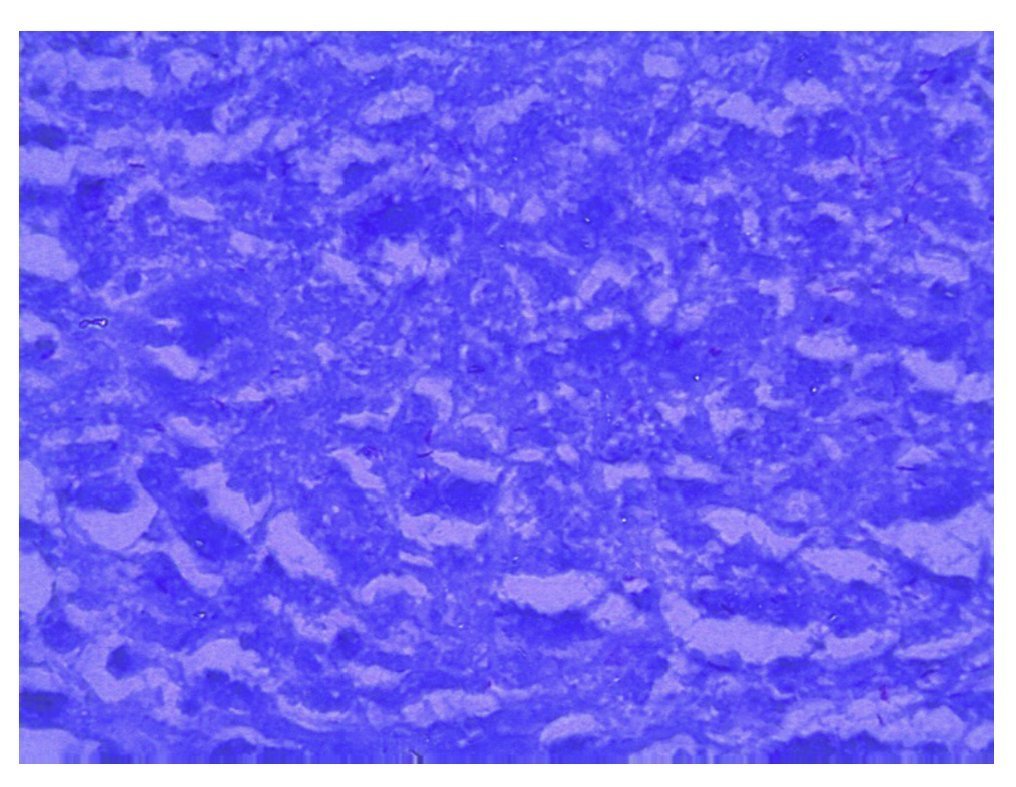
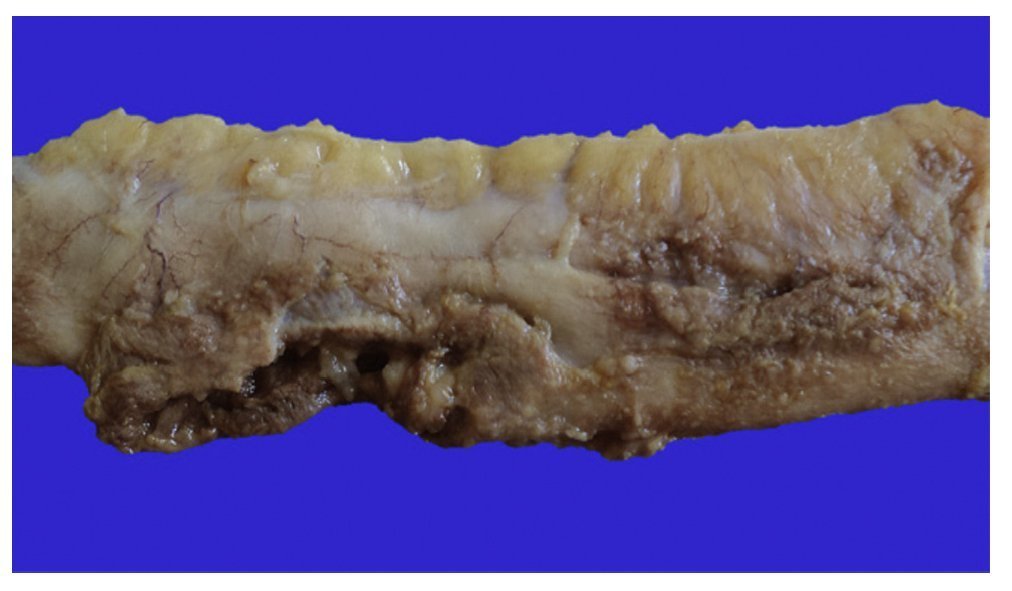
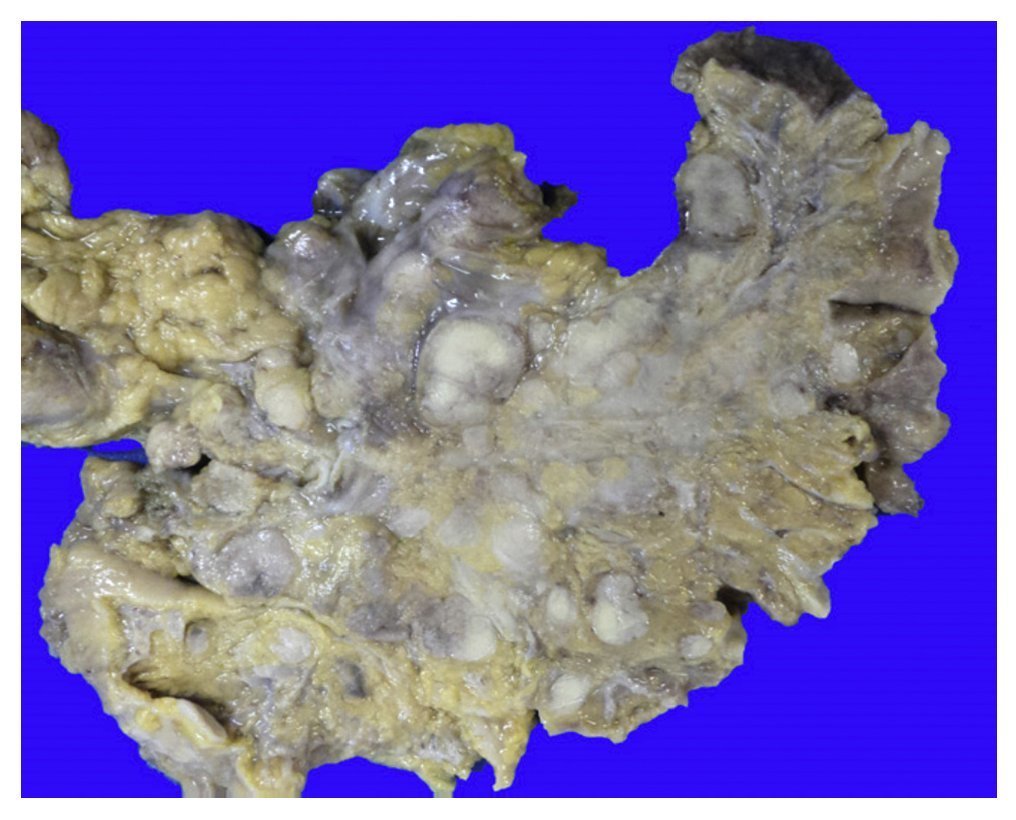
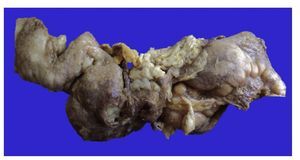
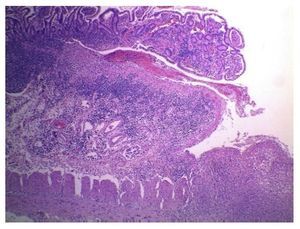
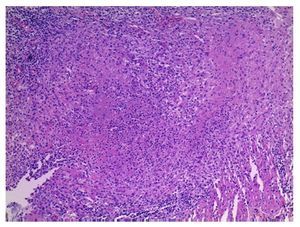
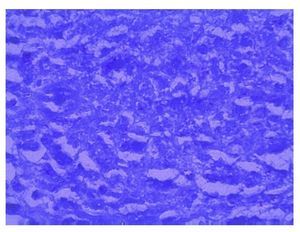
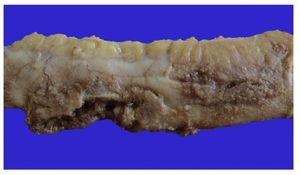
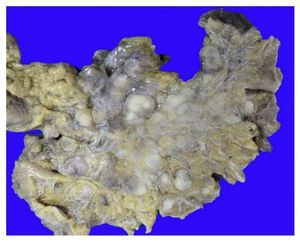
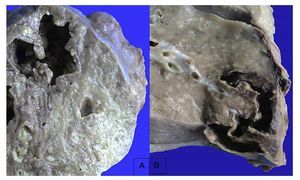
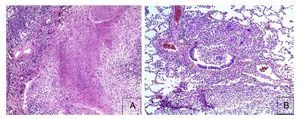
First we show the surgical specimen of a segment of ileum where we can see dull, opaque serosa with a 2-cm diameter perforation and with irregular margins that histologically corresponds to an ulcer covered by fibrin with dense inflammatory infiltrate (Figure 5). The ulcer is deep and extends towards the muscular wall and the serosa (Figure 6). In the wall thickness we can see necrosis, without the classic characteristics of TB, which is an area of caseous necrosis surrounded by a palisade of epithelioid histiocytes. An area of necrosis is seen and epithelioid histiocytes (Figure 7). With Ziehl-Neelsen stain, acid-alcohol resistant bacilli are identified (AARB) (Figure 8). The surgical specimen was diagnosed as chronic granulomatous inflammation due to mycobateria, compatible with intestinal TB. On autopsy, external appearance showed data of chronic malnutrition. The skin appeared dry and thin and with desquamation. Dental hygiene was poor. Surgical wounds were in the process of granulation. The most important findings were at the intestinal level. The small intestine remained with lesions of perforation and adhesions between the loops (Figure 9). There was 100 mL of purulent fluid and numerous small white nodules found throughout the peritoneum that corresponded to TB of miliary appearance, which involved the mesentery and serosa of both intestines. Histologically, ulcers presented granulation tissue and granulomatous inflammation, with central necrosis and involvement of vessels in the form of a vasculitis with necrosis and multinucleated giant cells, characteristic of tuberculous granulomas. There were TB lesions in other organs such as in salivary glands, cervical lymph nodes, mediastinal nodes, mesenteric nodes (Figure 10) and retroperitoneal nodes. No granulomas were found in the esophagus and stomach, but esophagitis and acute ulcerated gastritis were found. There were numerous peritracheal and peribronchial adenomegalies present.
Figure 5 Segment of small bowel that shows dull, opaque serosa and an area of 2-cm perforation with necrosis and sludge.
Figure 6 Panoramic view of the microscopic appearance of an ulcerated area in the mucosa that extends to the entire wall (HE x25).
Figure 7 Close-up of the borders of the area of perforation where coagulative necrosis and inflammation with poorly formed granulomas is seen (HE x25).
Figure 8 Ziehl-Neelsen stain showing various acid-alcohol resistant bacilli.
Figure 9 Macroscopic appearance of a segment of small intestine with an area of perforation 3 cm in length and other pinpoint areas.
Figure 10 Mesentery with numerous lymph nodes with caseous necrosis.
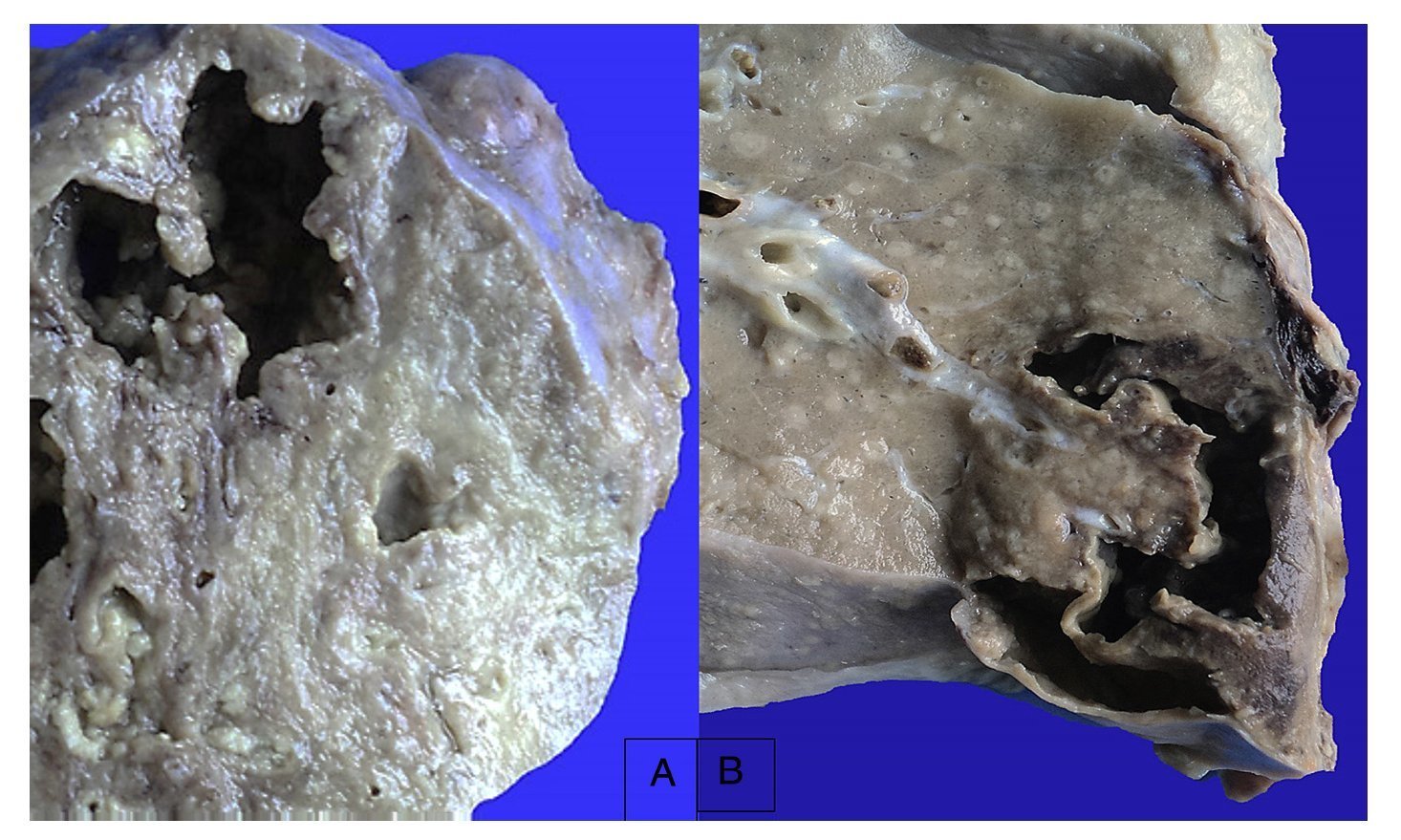
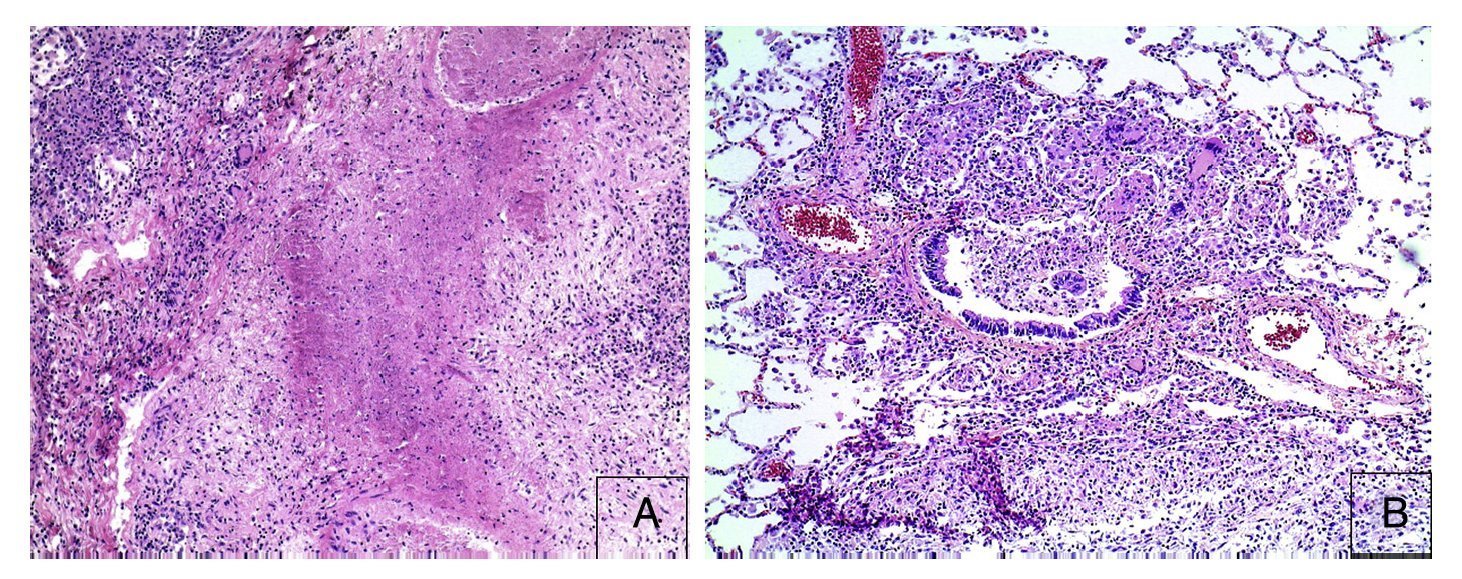
In the lungs, the pleura were dull with numerous whitish nodules that also corresponded to granulomas and pleural adhesions (Figure 11). Histologically, granulomas with necrosis were seen. On section there were cavitary lesions seen in the left upper lobe as reported on the CT scan. There were other larger lesions in the right lung and the lower lobe (Figure 12). In addition, there were multiple whitish nodules seen throughout the parenchyma, which corresponded to miliary TB and caseous nodules with cavitation. Histologically, the whitish nodules corresponded to granulomas with multinucleated giant cells. There was involvement around the bronchioles and there was necrosis in the vessels. There were two large vessels with vasculitis and areas of infarction around them, which evolve to cavernous formation (Figure 13). There were some calcifications. Ziehl-Neelsen stain was positive for AARB.
Figure 11 Outer view of the lungs that show dull thickened pleura with adhesions on the left basal portion and numerous small nodules on the surface.
Figure 12 Appearance of the lungs on section. Areas of necrosis with cavitation that correspond to the left upper lobe (A) and lower right lobe (B).
Figure 13 Histological appearance of the lung. Areas of caseous necrosis with chronic inflammation and some giant multinucleated Langhans type cells (A) are seen. Granuloma without necrosis with giant Langhans cells with destruction of the bronchiole are noted (B).
An inflammatory exudate with fibrin and some small granulomas were found in the thickness of the pericardium. The liver was large, nodular, with accentuation of the lobular pattern. On section it presented a micronodular appearance with numerous whitish brown nodules, which corresponded to granulomas. These were seen in the parenchyma as well as portal spaces. In addition, there was diffuse steatosis, cholestasis and iron deposits. The gallbladder, which on imaging was described as thick-walled, showed thickened serosa as part of the dissemination of the TB in the mesentery and peritoneum. The interior the mucosa was noted to be dull, opaque and with small calculi. The kidneys were mildly increased in size, with medullary congestion and also showed white nodules that corresponded to TB dissemination with caseous granulomas. There were also data of acute tubular necrosis with detachment of the epithelium and granular cylinders. The adrenal glands showed granulomas on the surface and in the interior and hemorrhage in the deep portion of the cortex. In the uterus, abundant deposits of caseous material were seen on the surface and in its interior. The urinary bladder also had thickened walls with presence of granulomas. There was miliary TB dissemination in the diaphragm, thyroid gland and pancreas. The thymus was small, atrophic and with adipose infiltration. In the central nervous system there were data of atrophy with dull, opaque meninges and with miliary dissemination seen. Interestingly, although TB tends to affect more the basal portion, here it presented most over the hemispheres. On section, dilation of the ventricles was seen. The circumvolutions were small and there was very intense congestion of the meninges and vessels. The fourth ventricle was also noted to be dilated and there was necrosis of the folia of the cerebellum. Miliary TB was found in the spinal cord around the cavity.
Final pathological diagnoses were the following:
Principal disease
• Disseminated TB in lungs, lymph nodes (cervical, thoracic, mediastinal and mesenteric), larynx, bronchi, pericardium, salivary glands, small and large intestines, mesentery, liver, spleen, pancreas, kidneys, bladder, uterus, bone marrow, meninges and vertebral canal.
Concomittant disorders
• Intestinal perforation
• Exploratory laparotomy with intestinal resection (10 cm)
• Acute and chronic granulomatous peritonitis
• Acute and chronic granulomatous pericarditis
• Pericardial effusion (150 ml)
• Pleural effusion (200 ml, hemopurulent)
• Purulent ascitis (100 ml)
• Anatomic data of shock
• Hypoxic-ischemic visceral myopathy
• Acute tubular necrosis
• Necrosis of cerebellar cortex
• Chronic malnutrition, weight 29.5 kg, height 1.47 m
• Chronic dermatitis with atrophy
• Hepatic steatosis
• Cerebral atrophy
Independent alterations
• Chronic lithiasic cholecystitis
Cause of death
• Septic shock
The diagnosis of TB continues to be a problem, especially in children because the manifestations are nonspecific. Children are not frequently bacillipherous and there is a high frequency of extrapulmonary presentation with even less precise symptoms. There are important risk factors such as socioeconomic, malnutrition and immunological disorders. Extrapulmonary presentation ranges from 4-6% of all cases of TB up to 60% in areas of high prevalence.1-3 At the National Institute of Pediatrics in Mexico, in a study of 153 autopsies with a diagnosis of TB, 17 cases (15%) were found with peritoneal or intestinal involvement such as presented in this case. Of these, 14 were cases with disseminated miliary forms. The cause of death was also attributed to the activity and dissemination of the disease.4,5
5. Final comments
5.1. Infectious disease (Dr. Sarbelio Moreno)
Normally, TB is known as the great imitator that can cause any syndrome. In this case, the diagnosis should have been strongly suspected because the patient was Coombs’ positive as evidenced by the brother with TB. The conditions for TB being highly prevalent in Mexico are deprivation and mis-treatment although this does not mean family abuse; malnutrition is the maximum manifestation of abuse. The AIDS epidemic has also had an influence, but much of it is due to the lack of information (of the population and by the health sector) on how the contacts should be treated.6 This case could also be explained by the low socioeconomic status. It is very important to provide adequate treatment and to know prior sensitivity to antimicrobacterial drugs.
With the history, clinical picture, manifestations and severity, it was undisputed that the patient would be studied for TB. An intestinal origin was mentioned. This is important because if the bacterium was Mycobacterium bovis, treatment with pyrazinamide would be of no use. The patient should have been treated with an antimycobacterial scheme and would have included rifampin, ethambutol and pyrazinamide. One advantage of the GeneXpert MTB/RIF® is that it identifies the primary sensitivity to rifampin. However, there was a high probability that the patient, due to having had contact with someone who had already been treated for TB, could have presented multiresistance. Management of the intensive care treatment to provide ventilatory support is very important as well as control of fluids and electrolytes.
5.2. Surgery (Dr. Eduardo Bracho)
Several patients have been seen with TB in this institution over the past 25 years. Currently, this number is lower as previously there were five to seven patients per year. This patient is the first with a diagnosis of TB who had surgery performed in the last 2-3 years. There are some findings that the surgeon should keep in mind for suspicion of TB, although they are not pathognomonic. As previously mentioned, TB was categorized as the great imitator and this can also be mentioned from the abdominal point of view. Abdominal TB has been confused with ovarian tumors, inflammatory problems, flank problems, infectious problems or parasitosis. It has been categorized as other diseases and finally, after much time, has been confirmed to be TB. However, the fact of finding granulomas, the “millet grains”, both in the peritoneum as well as the intestine, added to the fact of the finding of enlarged lymph nodes in a patient with a history, usually chronic, of some type of intestinal problem plus malnutrition, should guide the thinking towards the possibility of TB.
5.3. Final comment
The present case is a vehicle to strongly draw attention to and be alert to reemerging infections, particularly TB, which occur much more frequently than is believed and is associated with immunosuppressed patients and with more severe conditions.
Received for publication: 2-3-15;
Accepted for publication: 2-4-15
http://dx.doi.org/10.1016/j.bmhimx.2015.03.003
Correspondence:
Dr. Mario Perezpeña-Diazconti
E-mail: mpdiazconti@gmail.com