Introducción: Las quemaduras son un problema de salud pública ubicado dentro de las 20 principales causas de morbilidad en México. Uno de los grupos más vulnerables son los niños. Al realizar un análisis de los casos, se aporta para un mejor entendimiento del problema y pueden generarse medidas preventivas al respecto. El objetivo de este trabajo fue determinar el perfil epidemiológico de niños con quemaduras que ingresan a la Unidad de Niños con Quemaduras del Hospital Civil de Guadalajara Dr. Juan I. Menchaca.
Métodos: Se realizó un estudio transversal que incluyó características demográficas del lesionado, de sus padres y de las quemaduras de niños atendidos durante 2009 a 2011. El análisis estadístico se llevó a cabo mediante el cálculo de frecuencias absolutas, proporciones e intervalos de confianza de 95%.
Resultados: El perfil epidemiológico de los niños lesionados fue principalmente de varones (63.4%) menores de cinco años de edad (65.2%), con escolaridad de acuerdo con su edad (69.2%); hijos de padres menores de 35 años con escolaridad básica. Las lesiones fueron causadas por agua (56.2%) durante el lapso de las 12 p.m. a las 11:59 p.m. (73.0%) produciendo quemaduras de segundo grado superficial y profundo o menores (69.2%) que afectaron menos del 20% de la superficie corporal total (74.5%).
Conclusiones: Este perfil epidemiológico permite ampliar el panorama de las acciones preventivas, iniciando con investigaciones científicas que orienten el rumbo que se debe seguir, trabajando conjuntamente con instituciones públicas y privadas en la elaboración de programas y estrategias, así como el establecimiento de una política pública para lesiones no intencionales.
Background: Burns are a public health problem, ranking among the 20 principal causes of morbidity in Mexico. Children are a more vulnerable group to suffer from these injuries. For that reason, we analyzed cases in order to gain better comprehension and to propose preventive measures for this problem. The aim of the study was to determine the epidemiological profile of those injuries to allow us to plan and implement actions for burn prevention.
Methods: We conducted a cross-sectional study that included demographic characteristics of the child, the parents and the burn injuries from children treated at this Burn Unit. Statistical analysis was done to calculate amounts, proportions and 95% confidence intervals.
Results: The epidemiological profile of the injuries included males (63.4%) <5 years of age (65.2%) with educational level according to their age (56.2%). Parents of the included children were <35 years old with basic educational level. Burns were caused by hot water (56.2%) and occurred between noon and midnight (73.0%). The majority of the burns were shallow and deep second-degree or minor (69.2%) and affected <20% of body surface area (74.5%).
Conclusions: This epidemiological profile paved the way for preventive actions beginning with scientific research to guide the actions in a progressive direction along with the cooperative actions of public and private institutions in the development of programs and strategies. The end result would be the establishment of a public policy for accidental injuries.
1. Introduction
Burns are a public health problem due to the physical, psychological, economic and social impact they cause to the injured persons and their families. In Mexico, in accordance with the Department of General Epidemiology (DGE) of the Department of Health (SS), burns before the year 2010 were not included on an ongoing basis among the 20 principal causes of general morbidity in the country. In that year these injuries ranked 18th place (123,291 cases)1 and in 2011 in 17th place (129,779 cases)2. According to morbidity from non-contagious diseases in 2011, these injuries occupied the seventh position, in fact three positions above those caused by motor vehicle accidents2.
There are two published studies on the epidemiology of children with burns in Mexico: the first, a descriptive epidemiological study on children with burns who were seen at the University Hospital Dr. José Eleuterio González of Monterrey, Nuevo León, which describes the demographic and clinical characteristics of those patients with second- and third-degree injuries3; the second is an epidemiological study of burned children treated in the Burn Unit of the Trauma Hospital Magdalena de las Salinas in Mexico City from 2000 to 20064.
In view of the importance of burns due to their incidence in the population and short-, medium- and long-term complications in persons with burns, the objective of the present study was to describe the epidemiological profile of children with burns who present for medical care at the Children’s Burn Unit (UNQ) of the Hospital Civil de Guadalajara Dr. Juan I. Menchaca (HCGJIM) from 2009 to 2011.
2. Methods
A cross-sectional study was carried out using a sample of consecutive cases from January 2009 to December 2011 in the UNQ of the HCGJIM. This project was evaluated and approved by the Research and Ethics Committee of the Region of Investigation in Public Health Institute (IRISP) and the HCGJIM. The UNQ of this hospital receives patients from the entire Mexican Republic. The hospital is attached to this tertiary level health care institution, which provides health services to uninsured persons or those affiliated with Popular Insurance (Seguro Popular). Selected patients were <16 years of age who were admitted to the UNQ due to burns. Patients’ clinical records contained the necessary information for the study and all parents agreed to participate in the study. Exclusion criteria were that the family did not agree to be included in the study and that the information obtained for the case was <80%. Using these criteria there were no case exclusions due to lack of information or the family not agreeing to participate in the study.
The variables included were classified into three groups:
Group 1. Information of the child: gender, age and education.
Group 2: Information of the parents: age, education and occupation of the mother and father.
Group 3. Information about the injury (burn): date when it was caused, if intentional, if the child was being cared for by another person at the time of the event, who was responsible for the child at that time, what caused the burn, place where the burn occurred, time when the burn occurred (00:0-05:59 h, 06:00-11:59 h, 12:00-17:59 h, 18:00-23:59 h), degree of the burn (first degree, second degree, superficial or deep burn, third degree); area of the body affected (head, neck, upper extremity, trunk, lower extremities and/or genitals), percent of body surface burned, place where the first medical care took place and time frame when the first instance of medical care was received.
For evaluation of the depth of the burns the classification proposed by Converse and Robb-Smith was used: 1st degree, 2nd degree superficial and deep and 3rd degree5. Data were captured and analyzed with the Epi Info for Windows program6 (v.3.5.4, Atlanta, GA) using absolute, relative frequencies and 95% confidence intervals, mean, median and standard deviation (SD). For the best analysis of the time frame (in months) of when the burns occurred, it was decided to group the months according to the seasons of the year; i.e., spring (March, April and May), summer (June, July, August) fall (September, October, November) and winter (December, January, February) and the analysis was done with the number of burn cases seen.
3. Results
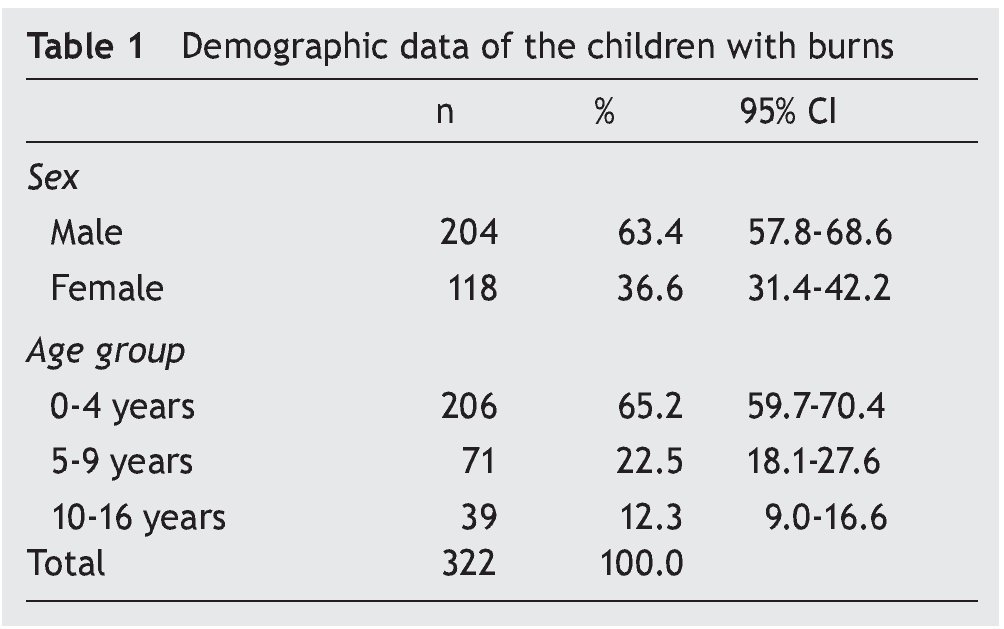
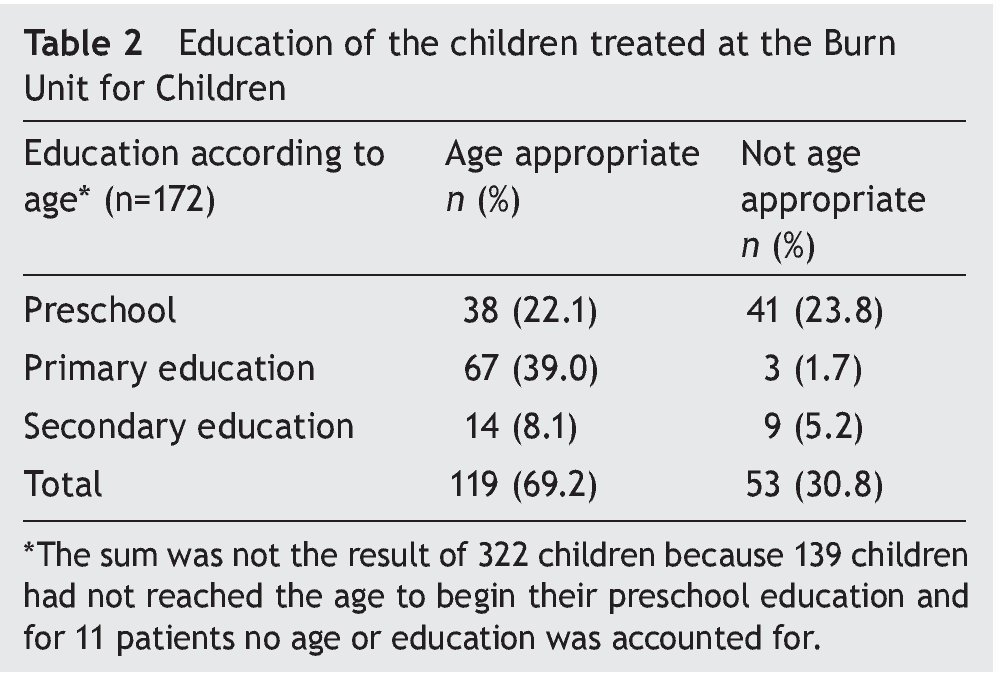
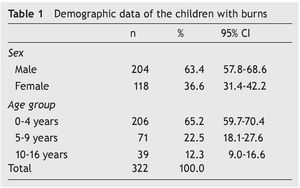
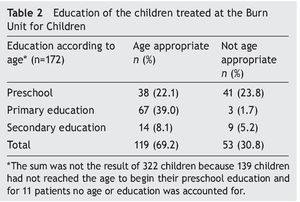
During the 3 years of study, data from 322 children with burns was obtained and who required medical care from the UNQ of the HCGJIM, of which 63.4% were males and 65.2% <5 years of age (Table 1). Education was age appropriate in 69.2% of the cases. The remaining children were not at the level of education that corresponded to their age (Table 2).
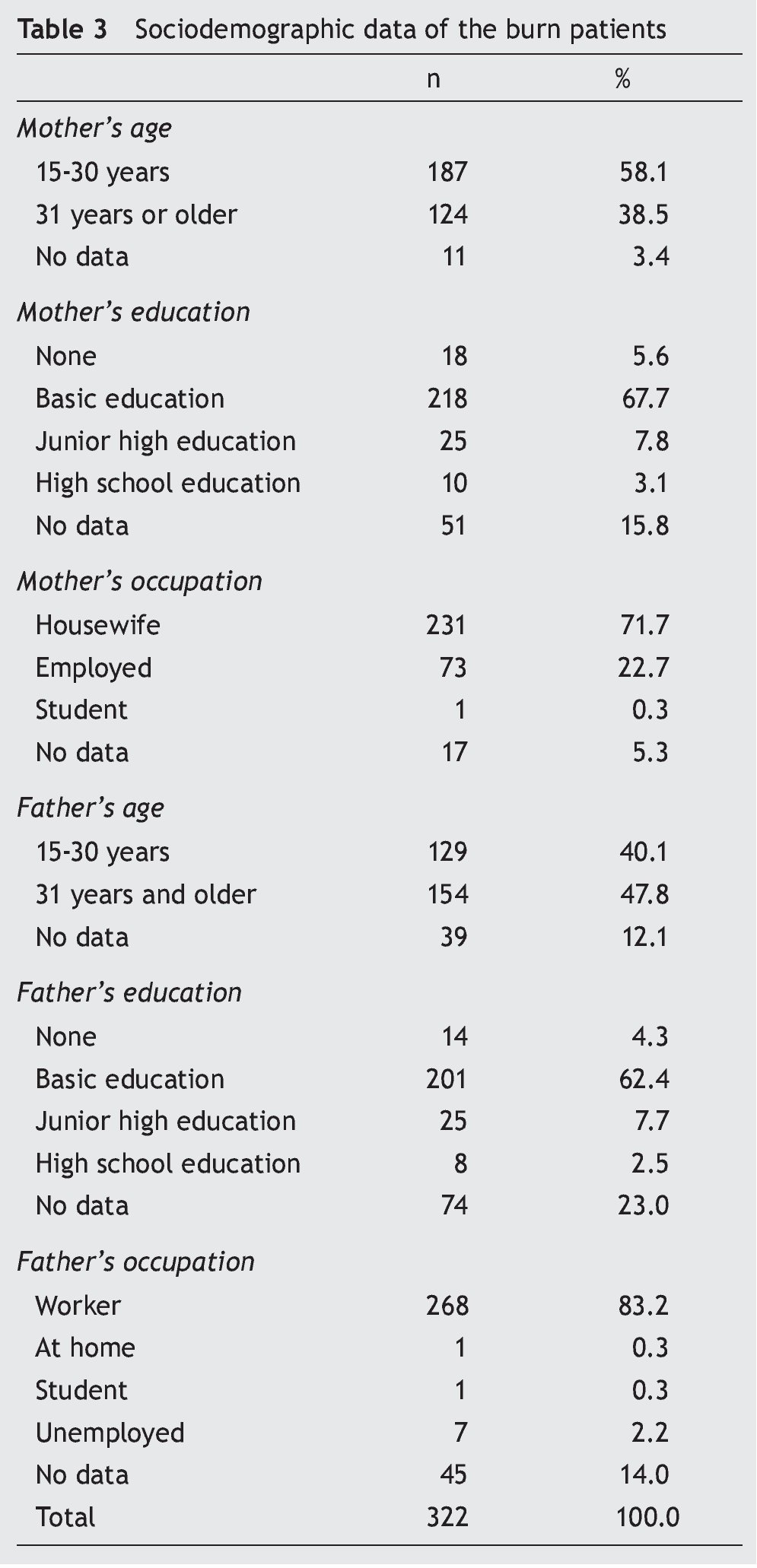
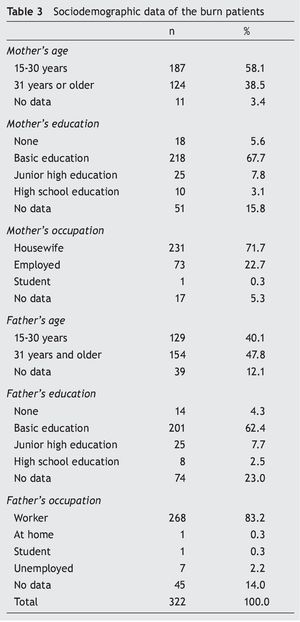
The profile of the parents of the burn patients was as follows: 58.1% of the mothers were between 15 and 30 years of age, 67.7% had basic education and 71.7% were homemakers. With respect to the parents, in almost half of the cases the age fluctuated from 31 years or older, 62.4% had basic education and 83.2% were employed (Table 3).
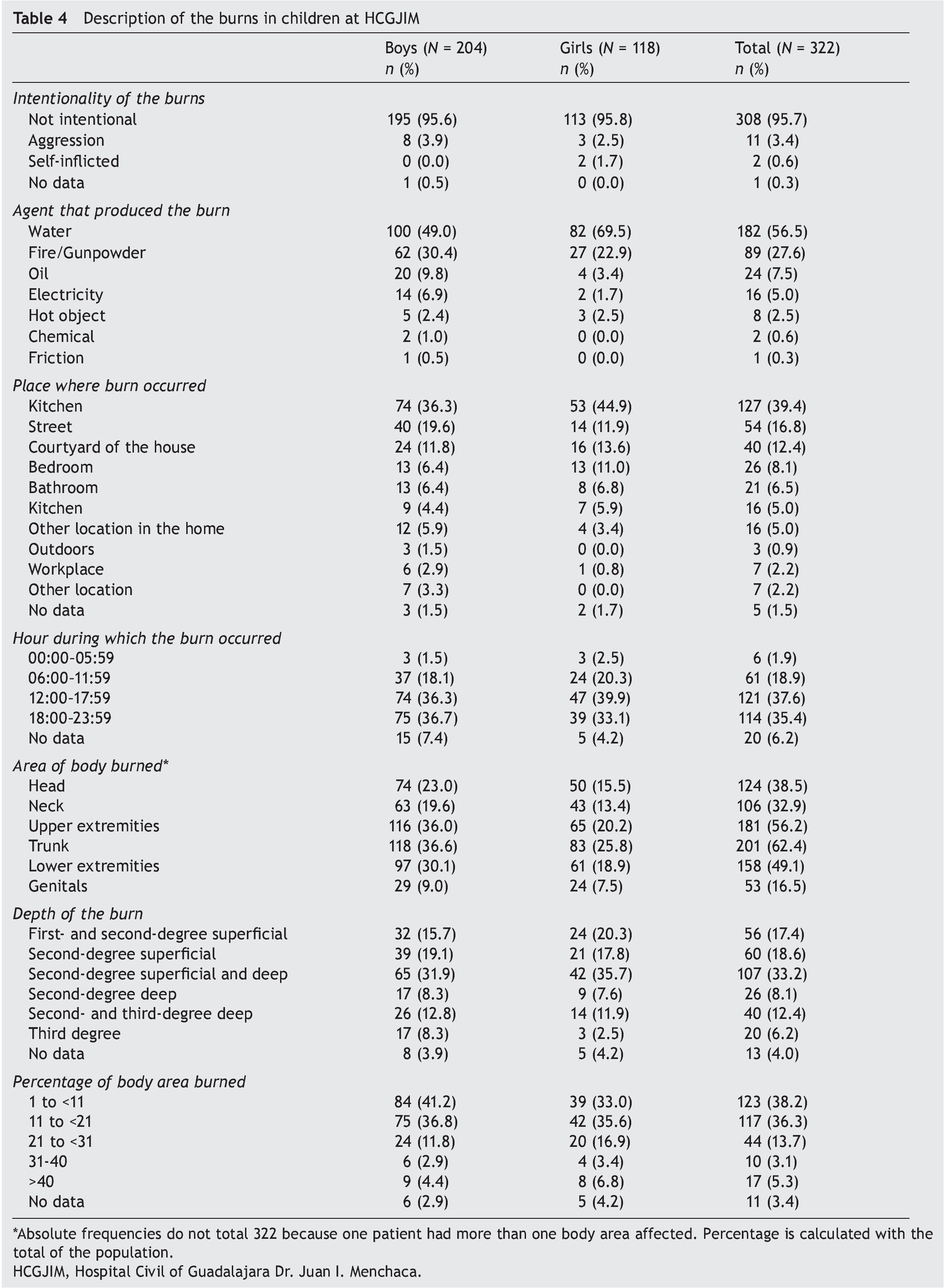
With regard to burns, the mechanism of the injury was not intentional in almost all their entirety (95.7%), the causal agent of the majority of the injuries (56.2%) was water; 39.4% of these events occurred in the kitchen and took place during the times from 12:00-17:59 h (37.6%) and from 18:00-23:59 h (35.4%). The depth of the burn produced was superficial second degree and deep in 33.2% of the children and 74.5% had <20% body surface burned. According to gender it was possible to observe that children with the greatest depth of burns were girls and with predominance in all the burn-causing agents. The average of the percentage of body surface burned was 15.9% (SD 11.8) and the median was 12.3%. With regard to gender, the average percent of body surface burned in males was 15.1% (SD 11.4) and in females was 17.3% (SD 12.3) (Table 4).
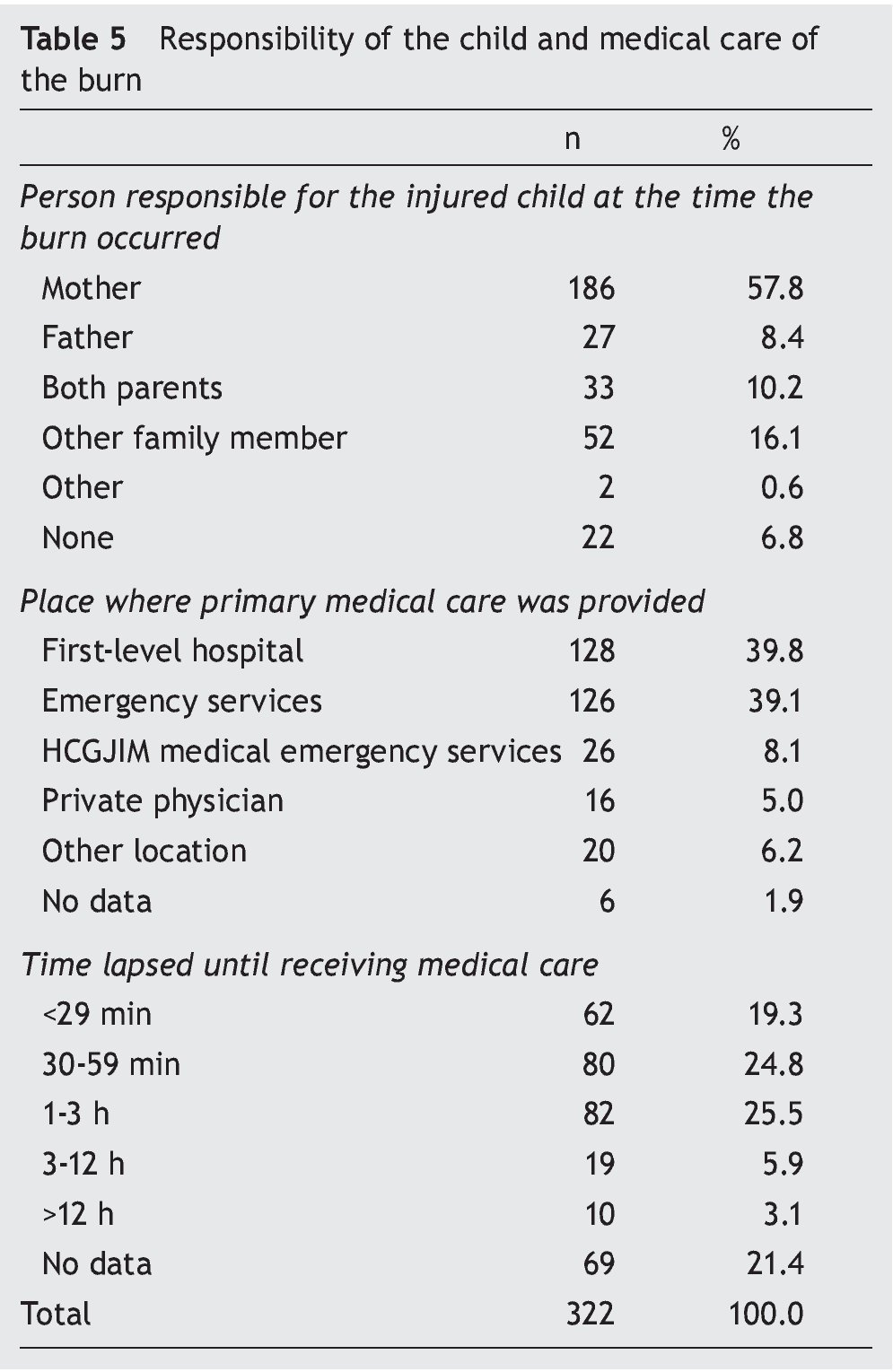
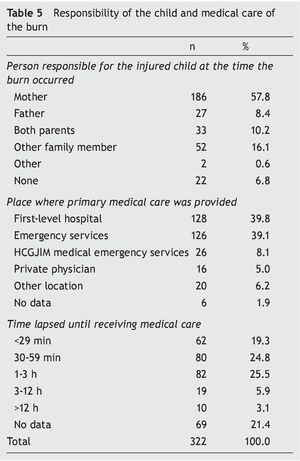
In these cases, during the time when the burn occurred there was someone responsible for the care of the children (93.2%); in the majority of the cases it was the mother (57.8%). Location where the injured child and the parents arrived as a first instance was to a first-level care facility (39.8%) or an institution that offers only emergency services (39.1%). Only 44.1% presented to a first-level care facility during the first hour or less from the time that the event took place (Table 5).
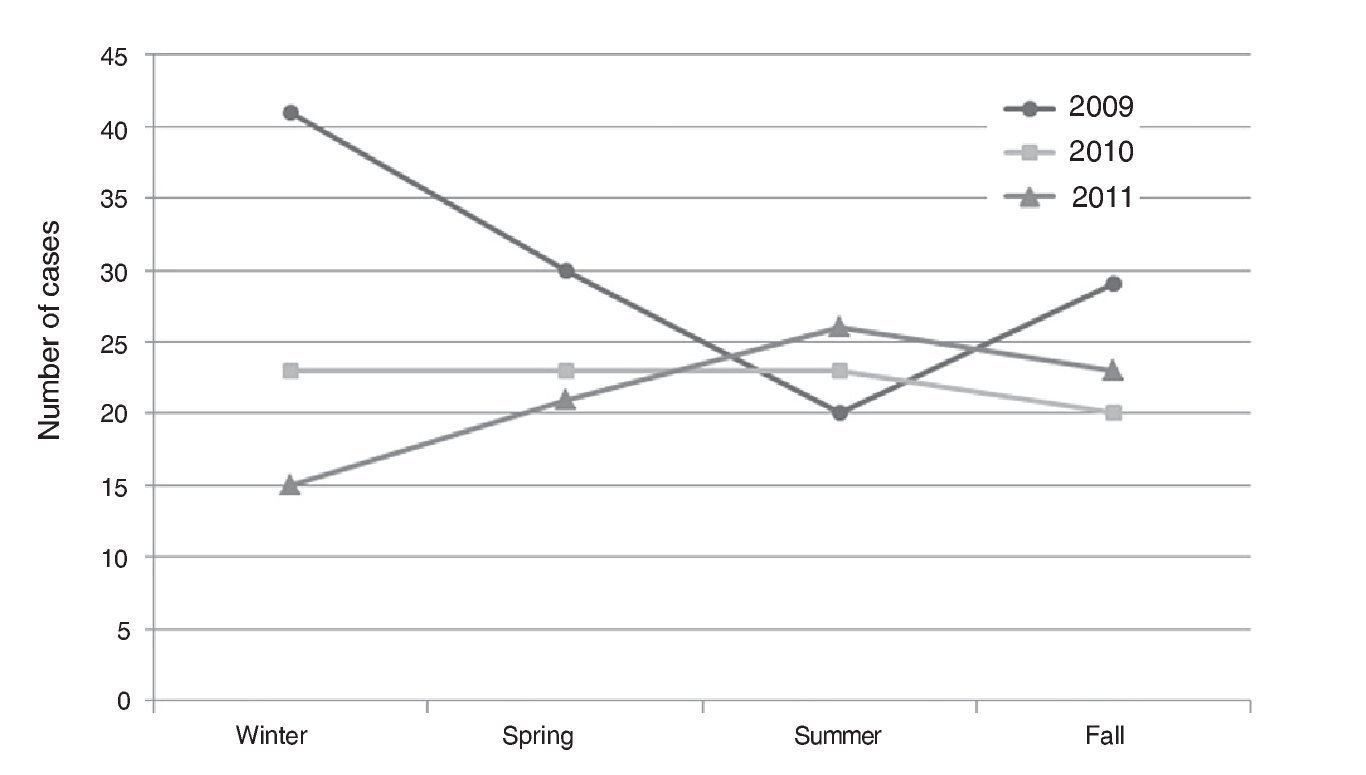
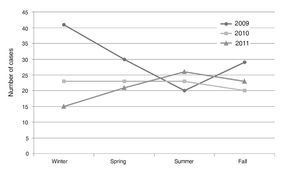
According to the incidence of burn cases from 2009-2011, there are differences seen in the 3 years: in 2009 the admission of patients was higher during winter, spring and summer seasons compared with the two following years, in 2010 the incidence of burn patients remained at the same level in the number of cases during the winter to summer seasons and in the fall a slight decrease was seen. Finally, in 2011 the most important increase occurred in the summer; being higher than in the 2 years prior. Together the number of cases by seasons of the year places in the first places the winter (79 cases) and in the spring (74 cases). The months of the year in which burns occurred with the greatest frequency were December (13.4%), November (10.6%) and in May (8.8%) (Figure 1).
Figure 1. Number of cases with respect to seasons of the year.
With regard to the depth of the burn, fire caused the greater part of third-degree burns and those of deep second degree and third degree; in the other categories, water was responsible for the depth of the burn (Table 5).
4. Discussion
The epidemiological profile of the child injured as a result of burns is represented by males <5 years of age1,4,5,7-19 who are injured more frequently than females7-17,20-22 except in the case of the Burn Unit of the Maternal Child Hospital of Tegucigalpa in Honduras18 where females are injured with greater frequency. They are the children of mothers who are housewives and with basic elementary education. With regard to the population cared for in the HCGJIM, it coincides with what is reported in other studies carried out in burn units or hospitals in countries such as Israel7,10, Brazil11, South Africa14, Chile15 and, in the Mexican context, states such as Nuevo Leon3 and DF4. Thus, the profile of the mother of the injured children agrees with that of mothers injured from the county of Fortaleza in Colombia23.
In terms of morbidity, the most common burns in children are as a result of contact with hot liquids, which cause scalding. This occurs in patients in hospitals from other countries7,8,11,12,14-17,19-22,24, but not so in Ikeja-Lagos, Nigeria9 or in Beer-Sheva, Israel10 where the principal agent was fire. The location where childhood burns most commonly take place is the home, in the kitchen, as in other studies7,11-13,16,18-20,24. However, it is different from what has been reported in southern China where the principal location for these injuries to occur is in the living room20.
With regard to clinical information of the burn, previously published studies agree in that the most common depth of the burn is second degree4,11,16,17. The results of the present study coincide with other studies11,21 where the most affected body part as a result of burns is the trunk. However, there are studies that report that the upper extremities are most commonly affected 9,13,15,17,20. According to the region of the body, it was shown that 16.5% of children suffered burns to their genitals and boys suffer burns with greater frequency than girls. A subanalysis of the burn agent and age of the child with genital burns was done; of the 9.0% reported in males, 3.7% occurred in those <5 years of age and 7.5% in females, 4.7% occurred in those <5 years of age. With the information obtained in the present study it is not possible to explain why these differences exist, but the mechanism of the event showed that children were playing near the work area of the parents. When leaving objects containing hot liquids on the floor, children may fall into the containers. When water is heated in containers for bathing in areas other than the boiler, they may be left on the floor and with only a moment of carelessness, a child can be burned.
The upper average percentage of the body surface burned in this study coincides with the averages from the University Hospital of the State of Lagos in Ikeja-Lagos, Nigeria9; Burn Hospital of Motahari of Tehran, Iran12; and in the Brno Hospital, Czech Republic21. Cases from the Burn Unit in Istanbul, Turkey8, Sheba Medical Center, Israel7; Soroka University Medical Center, Beer-Sheva, Israel9; Michigan Pediatric Hospital in the U.S.24 and the Burn Unit of the Xiangya Hospital of Changsha, China all have lower percentages20.
It coincided that the month of December was the month of the year with the highest incidence of cases in studies performed in Israel7 and Honduras18 in contrast with that reported in studies in Brazil11, China20 and the U.S.24.
The first instance of medical care sought by this population of patients are the services of the first level of care, which requires that personnel from this sector have the preparation and necessary training to provide first aid in order to limit the extent and depth of the burns as well as the possible short-term complications as a consequence of these injuries. In this regard, the National Center for the Prevention of Accidents (CENAPRA) has guidelines for the general population25 and for health professionals26 where sections for prevention of the events, performing first aid once burns occur and a general outline for the medical management of burns.
This study has the strength of demonstrating the epidemiological profile and behavior of burns in children without a social safety net from the western region of the country who present to the HCGJIM. This offers a panorama for suggesting preventive measures for decreasing the incidence and severity of the injuries due to this public health problem. The study limitations are that because it is a descriptive study, it provides the hypothesis for subsequent studies and does not allow making causal inferences.
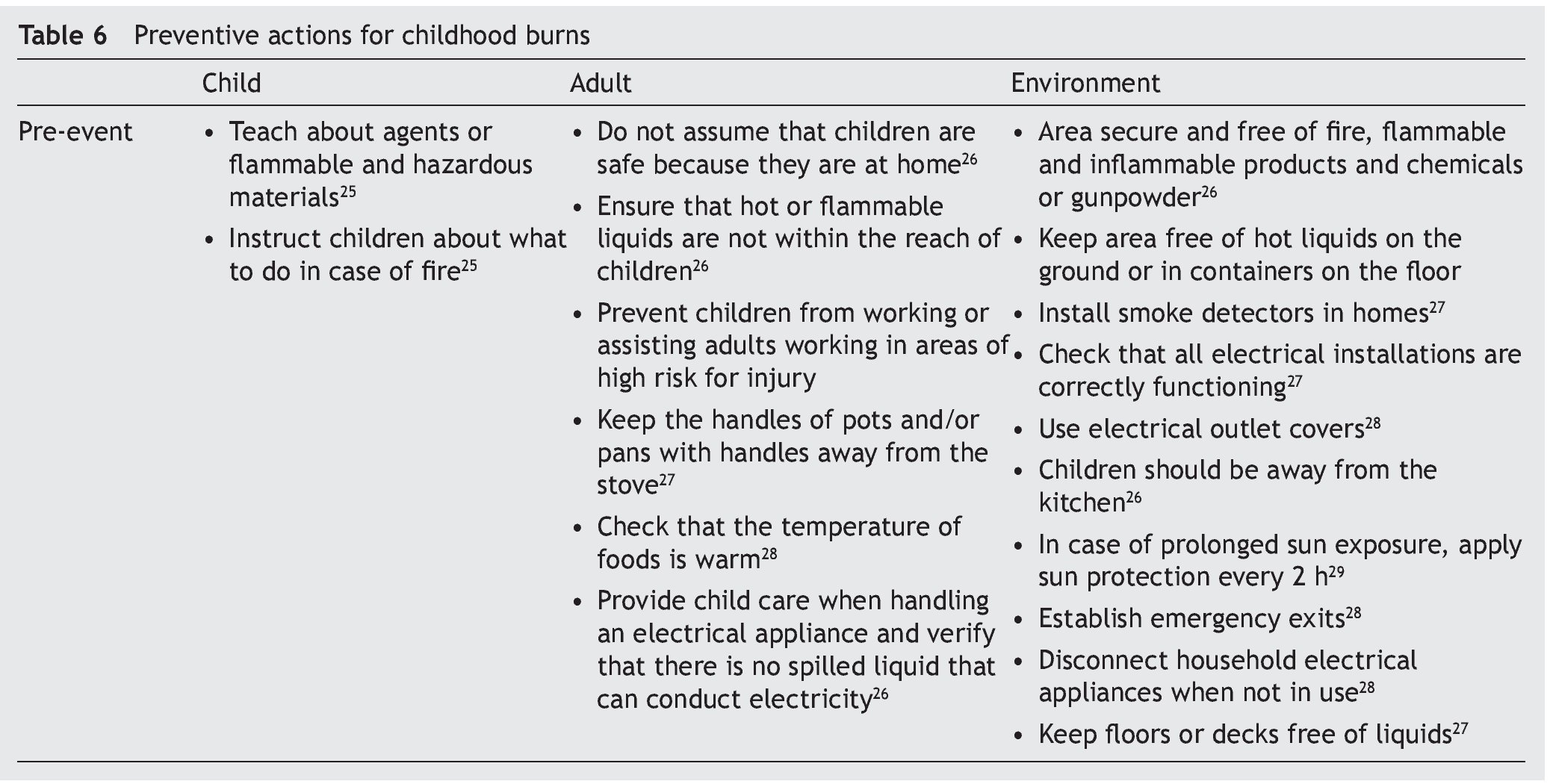
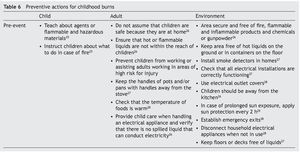
In conclusion, having determined an epidemiological profile of children with burns cared for in the Hospital Civil de Guadalajara Dr. Juan I. Menchaca, we are aware of the general and clinical characteristics of these events, which could allow for the planning and design for programs for promotion and prevention of burns during childhood and to also review the known measures in this regard, directed at children, adults and the environment (Table 6). An aspect that should be promoted is the incorporation of the pre-school and school-age curriculum for preventive burn measures such as previously stipulated with driver education.
Ethical disclosure
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflict of interest
The authors declare that there are no conflicts of interest.
Received 3 June 2015;
accepted 28 July 2015
* Corresponding author.
E-mail:maria.orozco.valerio@gmail.com, dracmm@yahoo.com.mx (M.J. Orozco-Valerio).