Introducción: El objetivo de este estudio fue demostrar si la decisión de realizar una tomografía axial computarizada de cráneo (TACC) en un paciente con traumatismo craneoencefálico (TCE) no severo se encontraba determinada por la presencia o ausencia del médico tratante durante la valoración en el servicio de urgencias.
Métodos: Se seleccionaron los expedientes de 92 pacientes de 8 meses a 4 años de edad. Los pacientes acudieron al servicio de urgencias del Hospital Español de México por TCE. Para la valoración inicial se utilizó la escala de coma de Glasgow (ECG). Se consideraron los siguientes criterios: pacientes con o sin realización de TACC, pacientes con médico tratante que acudió a la valoración inicial, pacientes con médico tratante que no acudió a valorar al paciente y pacientes valorados por el médico de guardia.
Resultados: Se determinó que al 38% de los pacientes con TCE no severo se les realizó TACC; el 8.6% tuvo alguna alteración; la intensidad de impacto moderada fue mayor en el grupo con TACC. De acuerdo con la ECG se encontró que la mayoría de los niños se localizaron en el puntaje 15 (p = 0.03). En aquellos pacientes sin médico tratante se observó una tendencia mayor a la realización de TACC.
Conclusiones: En pacientes pediátricos con TCE no severo sin datos de deterioro neurológico se sugiere una valoración clínica detallada y que genere confianza en los familiares, con la finalidad de evitar la toma de TACC cuando su uso no se encuentra justificado.
Background: The main goal of this article was to evaluate if the decision to perform cranial computed tomography (CT) in children with minor head injury is determined by the presence or absence of the physician during assessment in the emergency room.
Methods: Clinical files of 92 patients from 8 months to 4 years of age were selected. Those children were evaluated at the emergency department of the Spanish Hospital of Mexico due to non-severe traumatic brain injury. Glasgow Coma Scale (GCS) score was determined in all patients. Groups of patients were compared: 1) patients having CT, 2) patients with a physician who attended the initial assessment, 3) patients whose attending physician did not arrive to assess the patient and 4) patients assessed by the emergency room staff.
Results: 38% of patients with non-severe brain injury underwent CT, 8.6% had a brain injury visible on the CT. Moderate intensity impacts were greater in patients with CT. Regarding the ECG, it was found that most children scored 15 points (p = 0.03). In patients without a physician, a greater trend was demonstrated for performing CT.
Conclusions: Patients with minor head injury but without neurological signs should undergo a detailed clinical evaluation in order to avoid unwarranted CT.
Pagina nueva 1
1. Introduction
Traumatic brain injury (TBI) is the direct injury of the cranial, brain and meningeal structures caused by a mechanical force.1 There are various TBI classifications. However, in our environment, the one most utilized is the classification according to severity.2 The Glasgow coma scale (GCS) is universal and numerically establishes using clinical examination the degree of TBI, which could be mild, moderate or severe. In infants and pre-school children the modified GCS is used because the values to be evaluated depend on the child’s neurological maturity.3,4
In mild TBI there is no alteration in the awakening state and there are no data of focal neurological changes. If there are symptoms, these tend to be demonstrated immediately after the trauma. Children who have TBI should be evaluated initially at the primary care site. In mild TBI, the risk of complication is minimal.5,6 Because of this, if during the first 24 h after a TBI no data of neurological deterioration are detected, the child can continue with usual routine activities and be monitored on an outpatient basis.
The patient with moderate TBI has a higher risk of complications. Therefore, inpatient neurological monitoring is recommended for 12 to 24 h after the impact. Finally, in severe TBI it is essential to maintain the cervical spine immobilized. The priority is to stabilize the airway and keep the patient hemodynamically stable. In addition, it is essential that a cranial CAT (CCAT) assess surgical treatment and closely monitor the patient in a pediatric intensive care unit.7
The importance of diagnostic imaging in the evaluation of TBI lies in the early detection of potential injuries requiring prompt treatment, thereby reducing the number of sequelae. CCAT is the gold standard in TBI because it provides great diagnostic certainty and is characterized by providing a precise view of the brain structures. Indications for a CCAT are established worldwide and are as follows: deterioration in the neurological state, presence of focal neurological signs, clinical evidence of intracranial hypertension, suspicion of skull fracture, seizures, intense headache, prior neurological pathology and severe TBI.8 In mild TBI, CCAT has a 95.4% sensitivity and specificity of 48.9%.9 The objective of this study was to demonstrate whether performing CCAT in non-severe traumatic brain injuries is determined by the presence or absence of the treating physician during evaluation in the emergency department.
2. Methods
2.1. Study population
This study was carried out from October 2012 through May 2014 in the Hospital Español de México (HEM) Emergency Department. Clinical files of 92 patients from 8 months of age to 4 years of age with diagnosis of TBI were included in the study. Patients were evaluated physically in the emergency department by the on-call physician or by the treating physician or by a treating physician who did not come in person to the emergency department but gave orders via telephone.
The intensity of the impact was classified as mild or moderate, depending on the height of the fall. Falls of >60 cm were considered as moderate injury. We excluded high-velocity trauma (such as vehicular accidents). An evaluation was done of the time elapsed between the TBI and arrival to the emergency services. Three groups were established: <1 h, from 1-24 h and >24 h-1 week.
The Glasgow coma scale (GCS) was used to evaluate the state of consciousness. Based on the GCS score, we selected patients with scores from 13-15, which was considered to be mild TBI. Also, the time of evolution between the TBI and arrival to the emergency services was assessed.
An on-call radiologist from the HEM interpreted the study. A normal CCAT was established when there was absence of skull fracture and absence of brain hemorrhage. Two groups were established: <2 years and between 2-4 years. Patients were also divided into those who had a CCAT performed and those who did not.
The Committee on Research, Ethics and Biosafety of the HEM approved the study protocol. The protocol was developed according to the Helsinki criteria.
2.2. Statistical analysis
Measures of frequency and percentages were developed for the statistical analysis of the variables of interest. A bivariate analysis was performed (c2 test for categorical variables) between the following variables: medical evaluation and performance of CCAT. The level of significance for the tests of hypothesis was p <0.05. Information was analyzed using the statistical program SPSS 20.
3. Results
A total of 92 patients with non-severe TBI (8 months to 4 years of age) were included in the study: 68.5% between 2 to 4 years of age and 31.5% <2 years of age. There were 45.7% females and 54.3% males; 38% (35) had CCAT. From these, 82.8% (29) required sedation. When comparing the groups of patients with and without CCAT, intensity of the moderate impact was higher in the groups with CCAT (60% CCAT vs. 42.2% without CCAT) without significant differences.
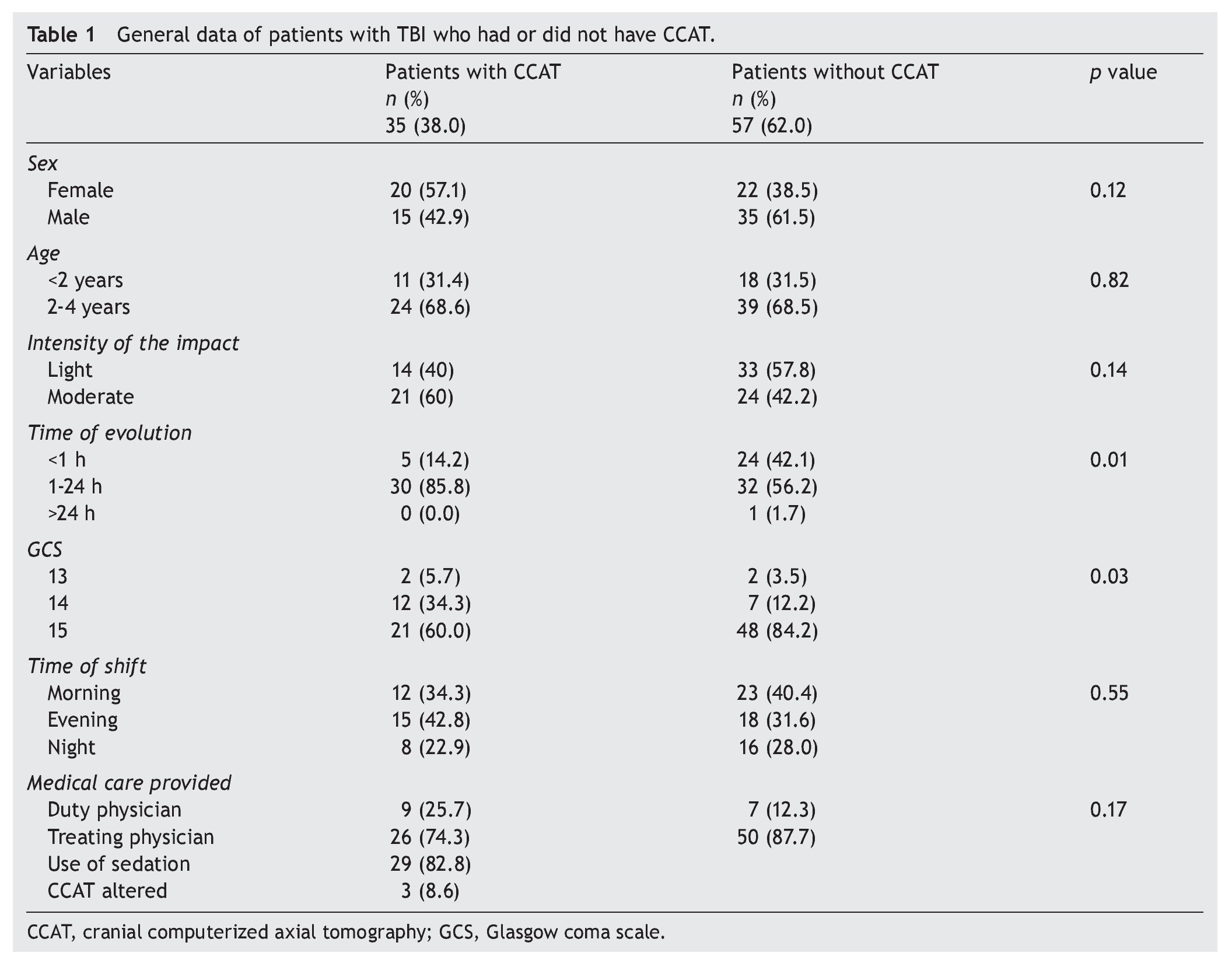
When the bivariate analysis was done between the group of patients with CCAT and the group of patients without CCAT in relation to the time of evolution of the injury, a similarity was found in both groups: the time of evaluation in the emergency department was 1-24 h (p = 0.01), although this factor did not modify the decision to carry out the study. According to the GCS classification it was found that the majority of the children were in the scoring group of 15 (p = 0.03). Table 1 shows the distribution of the characteristics of the participants.
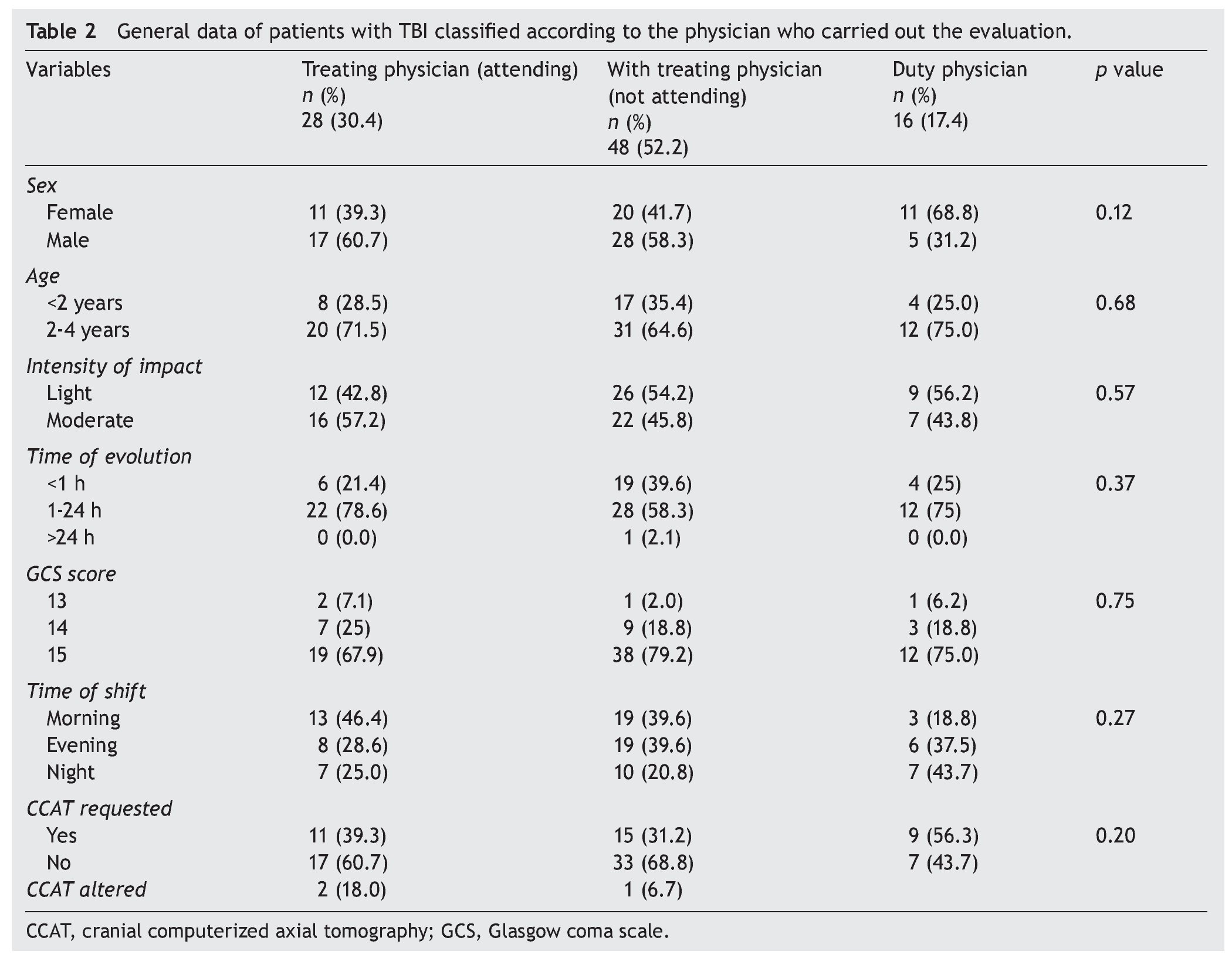
When the analysis was done according to the clinical evaluation by the physician, it was found that 52.2% (48) were evaluated by the treating physician who did not arrive to evaluate the patient in the emergency department. For the other groups, when the treating physician did arrive at the emergency room, 39.3% of patients had CCAT requested (11 patients); when the treating physician did not come to the emergency room, CCAT was requested in 31.2% (15 patients). In the group of patients evaluated by the on-call physician, CCAT was requested in 56.3% (9 patients) (p = 0.20). Three patients with CCAT (8.6%) showed findings positive for intracranial injury, two with subgalael hematoma and one with linear nondisplaced occipital fracture. Table 2 shows the distribution of the variables by classification from the physician who made the evaluation.
4. Discussion
In the present study it was found that in 38% of patients with non-severe TBI a CCAT was done at the time of presentation to the emergency services of the HEM. TBI is the most common trauma in pediatric patients, representing 6% of childhood accidents. Although it is generally mild, it is the first cause of mortality in children between 1 and 14 years of age and can result in severe sequelae.10
When comparing the groups of patients with and without CCAT, it was found that in the group of patients with CCAT the impact of the intensity was mostly moderate as opposed to the group without CCAT in which TBI were mainly of mild intensity.
In a study conducted in the pediatric population, it was found that the majority of patients evaluated for TBI in an Emergency Department were classified as mild (97.05%).11 According to the GCS classification, in this study it was found that most children in the groups studied had a score of 15 (mild TBI).
A smaller number of patients from this study (3 patients) had an abnormal CCAT result (8.6%). They were kept under neurological surveillance and were provided follow-up. Fortunately, this group of patients did not have subsequent neurological complications. This last percentage agrees with the results worldwide where it is estimated that 6% of patients with non-severe TBI will have some alteration in the CCAT.
CCAT has the capacity for observing acute traumatic injuries and is considered a diagnostic and follow-up method in children with TBI. In this study performed in a pediatric population in a Mexican hospital, it was found that the most common indications for CCAT were headache, convulsions/ epilepsy, structural abnormality, neurodevelopmental delay and attention deficit disorder and hyperactivity, which can be considered to be an overuse of CCAT without adequate justification for its use.12
Routine performance of CCAT in patients with non-severe TBI is unjustified. It is proposed that in all patients in whom there is doubt about performing CCAT, a complementary clinical assessment be done that would have a direct influence on the confidence of the family.
Results of this study cannot be extrapolated to the entire HEM population. It would be interesting to carry out a prospective study and to develop a scale that measures the anxiety level of the family. In those cases where the preoccupation of the family is observed to be linked to performing a CCAT, if a relationship is found, a method could then be established for controlling the fears of the parents and, in this manner, contribute to decreasing unnecessary CCAT exams from being performed.
Results of this study suggest the use of CCAT for diagnosis of TBI. It is essential that in all pediatric patients with a history of non-severe TBI without previous neurological pathology and without loss of consciousness, a detailed clinical assessment be done before requesting CCAT.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interest
The authors declare no conflict of interest of any nature.
Acknowledgments
The authors extend their appreciation to the authorities of the Hospital Español de México and to the Faculty of Medicine, Facultad Mexicana de Medicina Universidad la Salle for authorization and facilities for developing the study.
Received 24 March 2015;
accepted 18 May 2015
☆ Please cite this article as: Franco-Koehrlen CA, Iglesias-Leboreiro J, Bernárdez-Zapata I, Rendón-Macías ME. Decisión clínica para la realización de tomografía axial computarizada de cráneo en niños con traumatismo craneoencefálico no severo. Bol Med Hosp Infant Mex. 2015. http://dx.doi.org/10.1016/j.bmhimx.2015.05.007
* Corresponding author.
E-mail:linefra@hotmail.com (C.A. Franco-Koehrlen).