Bilateral Acute Iris Transillumination (BAIT) syndrome is characterized by a severe pigment dispersion with secondary iris atrophy and increased intraocular pressure (IOP). We report two cases of female patients aged 31 and 37 years respectively with a diagnosis of BAIT syndrome who required management for ocular hypertension secondary to pigment dispersion syndrome including medical therapy and surgical management in one case. It is important to consider BAIT syndrome as a differential diagnosis in pigment dispersion syndrome or pseudo-uveitis cases because of the need for timely management to prevent visual loss secondary to glaucomatous optic neuropathy.
El síndrome BAIT (Bilateral Acute Iris Transilumination por sus siglas en inglés) se caracteriza por presentar una dispersión severa de pigmento con atrofia del iris e incremento de la presión intraocular (PIO) secundaria. Se reportan dos casos en pacientes femeninas de 31 y 37 años con diagnóstico de síndrome BAIT que requirieron manejo para la hipertensión ocular secundaria a la dispersión de pigmento incluyendo terapia médica y en uno de los casos manejo quirúrgico. Es importante considerar el síndrome BAIT como diagnóstico diferencial en dispersión pigmentaria o cuadros de pseudo-uveitis debido a la necesidad de manejo oportuno con el fin de prevenir una perdida visual secundaria a la neuropatía óptica glaucomatosa.
First described in 2004 by Bringas Calvo et al.,1 the bilateral acute iris transillumination (BAIT) syndrome is characterized by sudden and severe pigment dispersion with iris atrophy and an increase in intraocular pressure (IOP). It affects young women between the ages of 30 and 50, and has been associated with upper respiratory tract infections, including COVID-19,2 and the use of moxifloxacin, clindamycin, and fumigation.3 There are few reports in the literature, most of which were conducted in Europe.1 In South America, a case report from Brazil is known to exist.4 The clinical presentation is characterized by pigment dispersion that can be associated with an increase in IOP, transient mydriasis, and bilateral iris transillumination, which appears late.5 Patients report significant photophobia due to mydriasis and the loss of iridial pigment.1,4 Visual prognosis depends on IOP control. An early diagnosis prevents the development of secondary glaucoma.4
Two cases of BAIT syndrome are reported from Medellín, Colombia, along with their possible triggers, pathophysiology, and treatment alternatives.
Case report #1A 31-year-old woman presented with a 1-month history of red eye and changes in vision. She denied ocular or systemic history. The physical examination revealed corrected visual acuity (CVA) in her right eye (RE) of 20/30, and in her left eye (LE) of 20/70. Pigment was observed in the endothelium and anterior chamber in both eyes (BE), along with 3+ cells. In the chamber angle, pigment 3+ was also found, the IOP was 25 mmHg in the RE and 17 mmHg in the LE, and the fundus showed the optic nerve with a 0.3 excavation in BE. The initial diagnosis was pigment dispersion syndrome-related bilateral uveitis. Topical treatment with fluorometholone 0.1% every 6 hours and brimonidine 0.2%, dorzolamide 20%, and timolol 0.5% every 12 hours was started. One week later, the patient still had symptoms, and iris transillumination was documented for the first time. Oral prednisolone (1 mg/kg) was initiated, and paraclinical tests to rule out uveitis-related causes such as HLA B27, VDRL, FTA ABS, and chest X-rays were requested, all of which turned out negative. The patient was then referred for glaucoma evaluation.
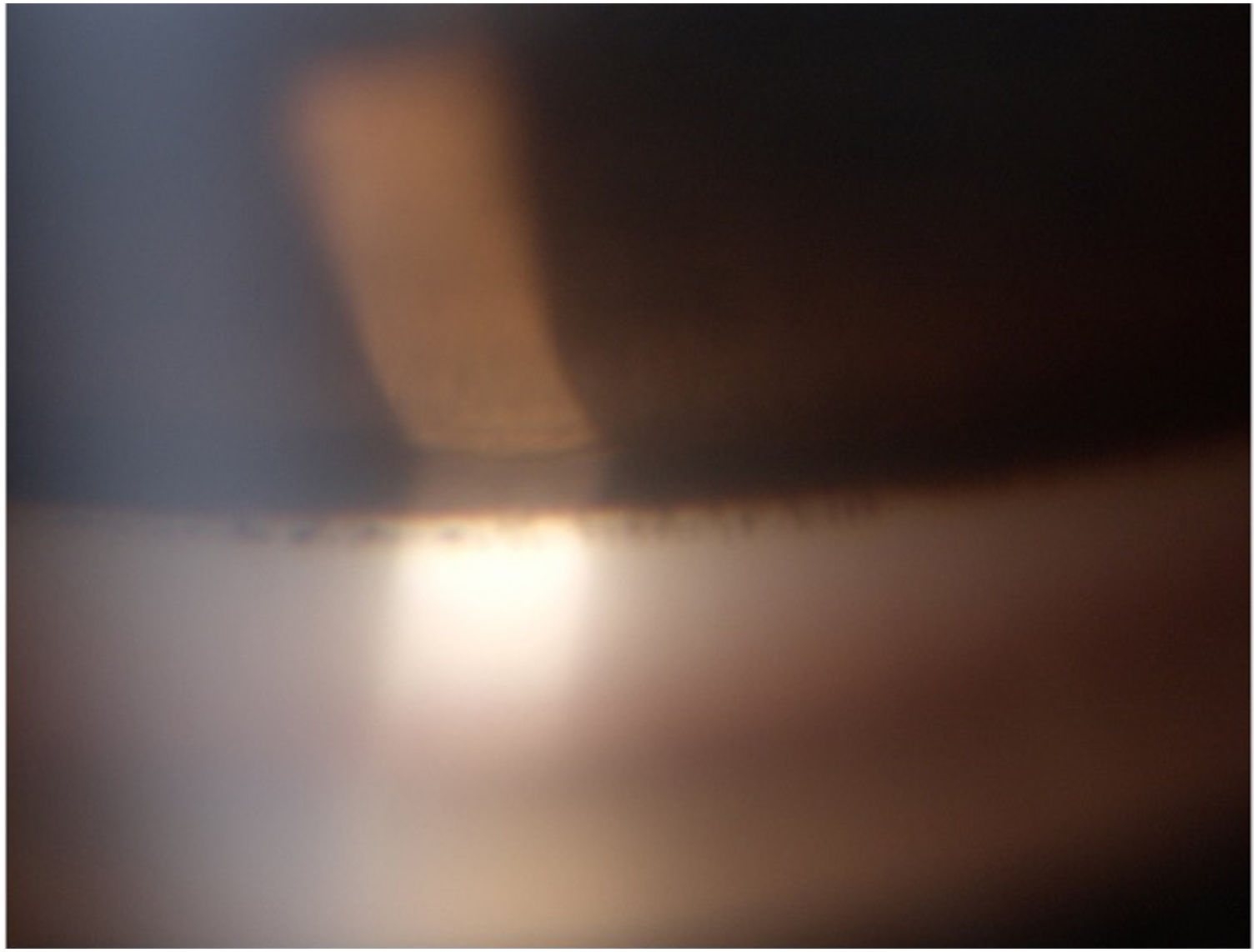
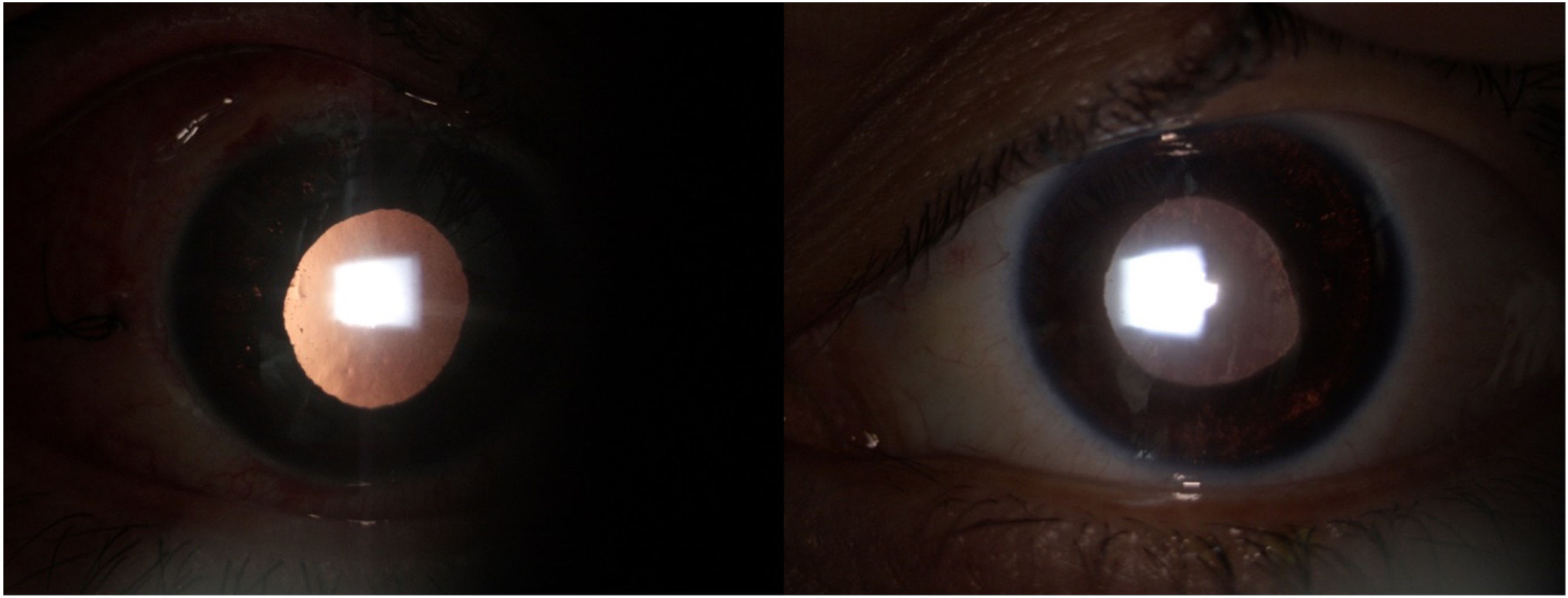
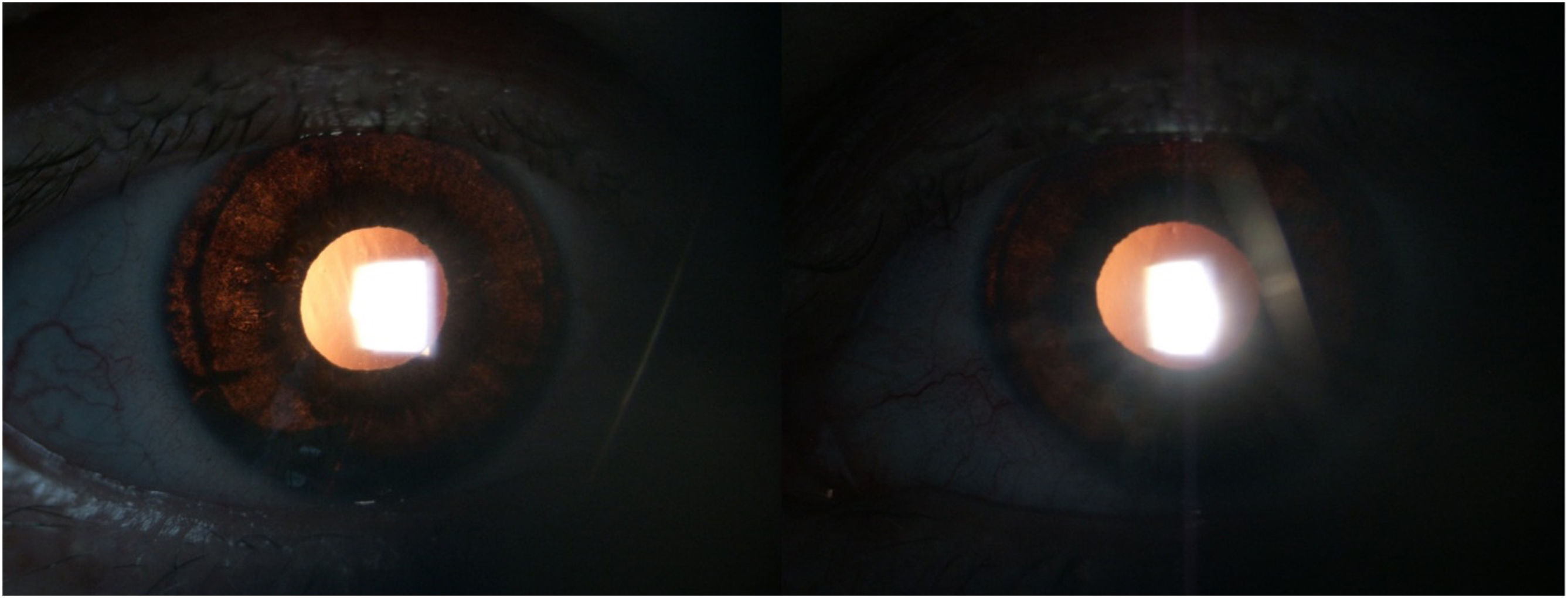
During the glaucoma evaluation, 2 months later, the IOP was found to be 41 mmHg in BE, despite the use of the prescribed drug, with abundant pigment in the anterior chamber, cornea, and angle (Fig. 1). Iris transillumination (Fig. 2) was evident and there was a marked increase in excavation: RE, 0.5 and LE, 0.7. Further questioning revealed that the patient had undergone surgery (lipolysis of abdominal fat) with postoperative treatment using oral moxifloxacin (400 mg/day for 7 days) prior to symptom onset. She also mentioned having had a flu-like illness two weeks before symptoms onset. Due to poor IOP control despite medical treatment and secondary glaucomatous neuropathy, a valvular implant (Ahmed, New World Medical, CA) was decided for BE, achieving adequate control of IOP and glaucomatous optic neuropathy.
Case report #2A 37-year-old woman, Colombian, residing in Canada, with a past medical history of upper blepharoplasty and frontoplasty, began experiencing intense photophobia the day after surgery. She was evaluated in the ophthalmology emergency department and diagnosed with bilateral anterior uveitis. Treatment with topical prednisolone 1% and tropicamide 1% in BE was started. One week later, she presented with worsening ocular pain, vision issues, photophobia, and nausea. Upon physical examination, corrected visual acuity (CVA) was 20/20 in the RE and 20/70 in the LE. The RE had endothelial pigment, 1+ cells, moderate mydriasis, and an IOP of 20 mmHg, with gonioscopy showing 2+ pigment. The LE showed conjunctival hyperemia, micro-cystic corneal edema, fixed moderate mydriasis, iris retro-illumination, and an IOP of 68 mmHg. The treatment for primary angle closure was started with a 150 cc mannitol bolus (20%) as a single dose and topical treatment with brimonidine 0.2%, dorzolamide 20%, and timolol 0.5% every 12 hours in BE. Tropicamide and prednisolone were discontinued. During follow-up, CVA was 20/20 in both eyes, IOP was 22 mmHg in BE, and optic nerve excavations were 0.2/0.2. Pupils were in moderate mydriasis, minimally reactive, and bilateral iris transillumination was reported (Fig. 3), along with endothelial pigment and anterior chamber pigment in BE.
Further questioning revealed that the patient denied any flu-like symptoms but mentioned previous abdominal fat extraction to be used as facial filler during surgery two weeks prior, with prophylactic oral cephalexin treatment (500 mg every 6 hours for 7 days). Based on this past medical history and the physical examination findings, a diagnosis of BAIT syndrome was established. The patient is currently on ocular hypotensive agents, with no progression of optic nerve damage but continued photophobia.
DiscussionThe BAIT syndrome has been described in middle-aged women. The clinical presentation includes severe pigment dispersion associated with conjunctival injection, ocular pain, blurred vision, transient or permanent increase in IOP, fixed mydriasis, and pigment deposition in the trabecular meshwork.1 Symptom duration ranges from weeks to months, requiring medical management and, in some cases, surgery. After the acute phase, patients may experience pupillary atony, bilateral iris transillumination, photophobia, and, if not diagnosed in time, ocular hypertension and glaucoma.1
Risk factors include upper respiratory infections and the use of antibiotics.3,4 In cases described in Europe, 75% were women with a mean age of 46 years, 81% of whom had upper respiratory tract infections treated with antibiotics (66% of these infections were treated with moxifloxacin.1) Other reports have associated the BAIT syndrome with COVID-19 infection. One of the most accepted theories regarding etiology is an inflammatory response to a viral infection.
To date, no direct relationship has been established between the use of moxifloxacin and BAIT syndrome. Among the adverse effects of quinolones (the class to which moxifloxacin belongs) is phototoxicity.1 Some authors suggest that moxifloxacin has an affinity for structures containing melanin, which could induce toxicity to iris pigment in previously sensitized patients.1 Wefers Bettink-Remeijer et al.6 reported 5 cases of patients with symptoms similar to uveitis after using oral moxifloxacin, concluding that iris transillumination and sphincter paralysis are recognized drug-related adverse effects.6
In the described cases, case report #1 presented earlier and more severely as pigment dispersion syndrome and required Ahmed valve implantation in BE for IOP control, whereas case report #2 presented less prominently, with no pigment dispersion. Initially treated as uveitis, it was later focused on medical treatment after signs of pigment dispersion were present, achieving IOP control without surgical intervention and no glaucomatous optic neuropathy.
The two hypotheses for increased IOP are the reduction of drainage in the trabecular meshwork due to excessive pigment obstruction1 or a secondary response to trabeculitis due to a viral infection, as seen in herpetic uveitis.7
Differential diagnoses should include pigment dispersion syndrome (PDS), hypertensive phase uveitis (Fuchs’ heterochromic iridocyclitis, Posner-Schlossman syndrome, herpetic iridocyclitis5), or bilateral acute depigmentation of the iris (BADI), which involves the release of pigment from the peripheral iris stroma,1 causing a geographic change in texture and color,8 with no epithelial involvement or transillumination. Some authors consider them different spectrums of the same disease.7 PDS shows pigment release in the middle peripheral iris, associated with localized transillumination in a radial distribution, iris concavity, and Krukenberg spindle. It ranges from asymptomatic patients to those with mild symptoms vs the BAIT syndrome, where patients are more symptomatic and exhibit severe and irreversible diffuse iris transillumination with secondary photophobia and pupillary atony, which are not typical findings in PDS.1
Treatment of BAIT syndrome should focus on controlling IOP and inflammation, initially with optimal medical therapy, and sometimes requiring surgical procedures such as external trabeculectomy, internal trabeculectomy, or even valvular implantation.1 Patients with adequate IOP control have a good visual prognosis, according to published results by Kawali et al.9 and Tugal-Tutkun et al.5
Among the described complications—in addition to glaucoma1—is cystoid macular edema, reported by Altan et al.10 in a patient with BAIT syndrome and cystoid macular edema at the 10th month of the clinical course. Another important side effect is iris transillumination, which presents bilaterally, asymmetrically, severely, and irreversibly, generating secondary photophobia. It is associated with pupillary atony and, sometimes, persistent ocular hypertension despite optimal medical therapy.1
ConclusionsBAIT syndrome must be recognized early, suspected in patients showing characteristic signs such as acute pigment dispersion, iris transillumination, and increased IOP, particularly in those with a history of respiratory illness or antibiotic treatment. This will allow for timely treatment and prevent secondary complications such as glaucomatous optic neuropathy.
Informed consentThe authors declare that they have obtained informed consent for the handling of patient data and the publication of their results.
FundingThis research did not receive any specific grants from funding agencies in the public, commercial or non-profit sectors.