Although in the 1940s there was an important decrease in global maternal/infant mortality rates, by the 1990s these rates had become stagnant. Many strategies to decrease maternal/infant mortality had been used, which included the prevention of pregnancy complications. Several studies showed an association between these complications and the stress perceived during pregnancy. However, there are some discrepancies which challenge this association. We believe that these discrepancies are due to the lack of understanding about the pregnant stress response and consequently the ways it is measured. The aim of this study was to understand how pregnant women perceive motherhood, pregnancy stressors and the psychological factors that attenuate the stress response.
Materials and methodsA qualitative study was conducted that explores the perception of gestational stress in 32 pregnant women who were recruited in different Health Centers. Semi-structured interviews were carried out which were conducted by the PhD student in charge of the project and each interview lasted 15–20min. Since the interviews were audio-recorded they were transcribed and the information was then categorized according to the three issues raised in the objective (motherhood, pregnancy stressors, and psychological factors that attenuate the stress response).
Results and conclusionsWe found that the gestational stress response and also its magnitude are influenced not only by how women perceive the aspects, but also and most importantly by its articulation. Likewise, results show that gestational stress is only attenuated when women perceive and cope with both the positive and negative aspects of pregnancy and motherhood.
Si bien en 1940 hubo una disminución importante en las tasas globales de mortalidad materno/infantil, hacia 1990 estas tasas se estancaron. Desde entonces se han utilizado muchas estrategias para disminuir la mortalidad materno/infantil, las cuales incluyen la prevención de las complicaciones del embarazo. Varios estudios mostraron una asociación entre estas complicaciones y el estrés percibido durante el embarazo. Sin embargo, hay algunas discrepancias que desafían esta asociación. Creemos que estas discrepancias se deben al poco entendimiento que tenemos sobre la respuesta al estrés durante el embarazo y, en consecuencia, en la forma en que esta se mide. Es por ello que el objetivo de este estudio es comprender cómo las mujeres embarazadas perciben la maternidad, los estresores propios del embarazo y los factores psicológicos que modulan la respuesta al estrés.
Materiales y métodosSe realizó un estudio cualitativo que explora la percepción sobre el estrés gestacional en 32 mujeres embarazadas que eran derechohabientes de los centros de salud. Para ello se realizaron entrevistas semiestructuradas, las cuales fueron realizadas por la estudiante de doctorado encargada del proyecto, y cada una tuvo una duración de 15 a 20min. Puesto que las entrevistas fueron audiograbadas, se transcribieron y se categorizó la información de acuerdo con los 3 temas planteados en el objetivo (percepción de la maternidad, estresores propios del embarazo y factores psicológicos moduladores de estrés).
Resultados y conclusionesEncontramos que la respuesta del estrés gestacional y su magnitud son influidas no solo por la percepción que tiene la mujer de estos aspectos, sino sobre todo por su articulación. Además, los resultados muestran que el estrés gestacional solo se atenúa cuando las mujeres perciben y enfrentan tanto los aspectos positivos como los negativos del embarazo y la maternidad.
Pregnancy is a bio-psycho-social process, characterized by significant changes in these three areas (Bjelica, Cetkovic, Trninic-Pjevic, & Mladenovic-Segedi, 2018; Cogollo-Jiménez, 2012; González-Ochoa, Sánchez-Rodríguez, Chavarría, Gutiérrez-Ospina, & Romo-González, 2018). During pregnancy, women are more sensitive in their social interactions and to the biological and physical changes that may result from emotional fluctuations (Farkas & Santelices, 2008). Because of all of these changes, pregnancy has been associated with disease since ancient times (Foster, 1980) and recently many authors view it as a stressful event (González-Ochoa et al., 2018; Huizink, Mulder, Robles de Medina, Visser, & Buitelaar, 2004; Lobel et al., 2008; Stanton, Lobel, Sears, & DeLuca, 2002).
In that respect, several studies in Mexico have shown that between 1922 and 1930 maternal/infant mortality rates had an important decrease (400 per each hundred thousand inhabitants). However, at the beginning of the 1930s, the Maternal Mortality Ratio (RMM) began to decrease considerably and in the mid and late 1960s there was a stagnation in maternal deaths. From 1990 to 2007 the MMR remained between 41 and 57 maternal deaths per thousand births (Aguirre, 2009). That is, in 1990 these rates become stagnant in spite of health strategies and medical policies. In fact, in 2015 the World Health Organization (WHO) found that 850 women die every day from preventable complications related to pregnancy and childbirth (i.e., severe bleeding, infections, gestational hypertension, complications during childbirth and dangerous miscarriages and abortions). In this context, many sanitary solutions have been implemented to reduce the number of maternal/child deaths. However, the results have not been as expected, since the numbers have decreased but nevertheless remain high (WHO, 2018).
This unimpressive result may be due in part to the fact that in underdeveloped countries such as Mexico, programs implemented are not necessarily based on scientific evidence, but more importantly, because the prevailing biomedical vision does not conceive pregnancy as a bio-psycho-social process. The same is true for gestational stress, even though several investigations indicate that maternal/child complications are associated with the stress experienced during pregnancy (Gangadharan & Jena, 2019; Goletzke et al., 2017). This association appears to be weak, due to the discrepancies observed and the methodological differences in their measurement (O’Donnell & Meaney, 2017). Thus, there are some studies that found associations between gestational stress and pregnancy/labor complications (Cole-Lewis et al., 2014) while others did not find this correlation (Kramer et al., 2009; Lukasse, Helbig, Benth, & Eberhard-Gran, 2014). Likewise, anxiety and depression during pregnancy are also associated with maternal/child complications that have been related to stress (Grote et al., 2010; Staneva, Bogossian, Pritchard, & Wittkowski, 2015). And there were no differences between the psychometric measures of stress and physiological markers such as cortisol (Bleker, Roseboom, Vrijkotte, Reynolds, & de Rooij, 2017; Peer, Soares, Levitan, Streiner, & Steiner, 2013). According to the reductionist view of stress, one tries to approach the phenomenon from one of these three perspectives: (1) stress defined as a physiological response, (2) stressors, which are conditions that activate a stress response and (3) coping strategies. This has generated inconsistencies in the study of the health-disease process. However, in the case of gestational stress, in which physiological, psychological and social changes are substantial, the reductionist standpoint of the phenomenon becomes unsustainable. For example, it would be nonsensical to leave aside the resources women have available to face the demands of pregnancy and to disregard both how motherhood is perceived by pregnant women and which aspects of pregnancy generate stress. In such a way that you can define the features that determine whether or not the accompanying challenges activate stress responses in pregnant women.
Thus, being aware of this is of utmost importance, since one of the first aspects of the definition of stress has to do with how a person perceives an event or a stressful demand that exceeds his/her resources to cope with it. In addition to this, the stress response is modulated by psychological variables; therefore, the consequences of stress will be different according to these aspects (perception of motherhood, pregnancy stressors, and pregnancy coping mechanisms). In this regard, Sapolsky (2013) has proposed five psychological factors that attenuate or intensify the stress response: predictability, control, empowerment, outlets for frustration and social support. However, it is unknown whether these factors are present in pregnancy, and if so, how they are manifested.
Thereby, in order to have a broader definition of gestational stress and therefore more sensitive strategies to measure and cope with it, these three main pillars of stress can be analyzed during pregnancy: (1) perception of motherhood, which is a relevant event, due to the evolutionary changes it represents, where the woman performs a cognitive assessment where pregnancy tends to be perceived as a threat or challenge (Lazarus & Folkman, 1984; Sandín, 2003); (2) stressors, which are those situations during pregnancy that generate ambiguity, uncertainty, lack of predictability, and make evident the lack of skills or behaviors needed to face the situation, and that trigger biochemical or electrical changes that produce a stress response (Boada-Grau & Ficapal-Cusí, 2012); and (3) the five psychological factors which are those variables that have the capacity to modulate the physiological stress response which can be explained briefly as follows: predictability: refers to accurate and relevant information of the situation that a person has in order to be able to cope with it. This predictive capacity is feasible only when the stressor appears with a certain frequency and intensity, since otherwise it may occur that people could adapt to the stressor, and therefore the stress response decreases. The second is control: extent to which a person feels that he/she can master a stressful event. The feasibility of this factor does not refer to how the person can exercise control over the stressful situation but rather that one feels in control of their own impulses. Thus control has to do with the degree of flexibility that the person has regarding a stressful situation. The third is social support which is the person or persons with whom the individual feels supported, heard, and nurtured when there is a stressful situation. The fourth is empowerment: it is the capacity to perceive that things are improving even if the stressor persists. The fifth is outlets for frustration: this is the capacity that the individual has to distract herself from the stressor and this is because the stress prepares the body for a sudden consumption of energy and therefore the person needs the distractor in order to discharge the energy generated by the organism; the distractor may arise from a positive activity or it may be a displacement of aggression (Sapolsky, 2013).
Thus, the objective of this research was to understand, by means of a qualitative study, how pregnant women perceive motherhood and to disclose pregnancy stressors and the psychological factors that attenuate the stress response.
Methodological strategyTo understand how pregnant women perceive motherhood and to disclose pregnancy stressors and the psychological factors that attenuate the stress response, the study was based on three definitions of stress, namely defined as a vital event that generates a stress response, a series of conditions or situations considered as stressors and variables that help regulate the stress response. The study was carried out with a qualitative methodology where semi-structured interviews were our main tool.
It should also be mentioned that a review of the literature (books and articles) was carried out on the subjects of stress and the bio-psychosocial process of the pregnancy, the relationship of these two variables allowed us to establish three aspects that help explain what is gestational stress (perception of motherhood, stressors and psychological factors). At the same time, it helped us to design the interview script and generate an interpretative framework for the responses given by pregnant women. Since our aim was to understand what gestational stress is, this research was based on a grounded theory model with a systemic design, which is used when the available theories do not explain the problem statement. Its main characteristic is that the data is preliminary categorized and then the resulting categories are organized in an interrelations model that explains the object of study (Hernández-Sampieri, Fernández-Collado, & Batista-Lucio, 2014).
The results presented in this research are derived from the testimonials given by pregnant women during the interview, whose objective is to illustrate the three aspects established for the understanding of gestational stress (perception of motherhood, stressors and psychological factors). These testimonies are true and were audio-recorded, transcribed and edited in order to present them in a fluid and coherent way.
In this sense a random sampling was carried out obtaining a total population of 34 pregnant women (18 primigravida and 16 multigravida-considered from the second pregnancy-) who were enrolled in any of the three pregnancy trimesters (1st trimester=10, 2nd trimester=13 and 3rd trimester=11). Those cases in which women reported a disease, that their pregnancy had been the result of rape, or those who did not finish the interview were excluded. Therefore, two interviews were eliminated because one of the participants had a chronic disease and the other interview was eliminated because it could not be concluded. The population consisted of women entitled to three different Health Centers belonging to the Ministry of Health, which provides care for people with low socio-economic status. It is worth mentioning that the ethics committee of this Health Institution reviewed and authorized the project (SESVER, 21 11 2014 UV-SESVER-IVEFIS). The average age of the participants was 24, most had attended junior high school (25%), senior high school (15.6%) and reported living with their partner (not married=53.13%, married=34.38%, single=6.25% and not specified=6.25%).
Pregnant women were approached in the waiting room of the three different Health Care facilities in the central area of the state of Veracruz: General Hospital Dr. Darío Méndez Lima, Huatusco Urban Health Center and the Banderilla Health Center. These places were chosen because of their proximity. The interviews were conducted by the PhD student in charge of the project, who conducted the interviews in the waiting room of these health centers since the women had no other time available to participate in the study. Each interview lasted from 15 to 20min. Before starting the interview, they were informed about the purpose of the study, and they were also asked for authorization to record the interviews. Personal data was used for research purposes only and confidentiality was guaranteed. Women who agreed to participate under these terms signed the informed consent.
For the analysis of the information, it was necessary to transcribe the interviews and to group the information according to the three core factors of our interpretative framework: maternity perception, stressors and psychological factors. It is worth mentioning that no software was used for the analysis, but rather a detailed reading of the information was carried out. The information was then classified according to the established points. In order to avoid individual prejudices, the analysis was carried out by consensus and the results were compared with the information found in the literature.
ResultsTo show the role that each core factor (perception of motherhood, stressors during pregnancy and psychological factors) had with gestational stress and its interaction, the content of the interviews was analyzed between multigravida and primigravida pregnant women and within different trimesters. The following analysis describes each of the core factors and their interactions.
MotherhoodMotherhood was perceived by all women as something beautiful and at the same time as something that generates concern, either because of the risk factors that may be present (multigravida) or because they do not know what to expect (primigravida). However, multigravidas use the qualifier beautiful to define motherhood and also some women use the term responsibility. For me it is a very beautiful thing, because having a baby is very beautiful, it is something that one does with love (multigravida of first trimester, 42 years). It is a very beautiful stage. Now I already have a nicer concept about what it is to carry a baby in your belly (multigravida of second trimester, 23 years). It is something very beautiful, but it is a lot of responsibility (multigravida of third trimester, 23 years).
While the primigravida define motherhood using words that involve learning and having to do with the care of the baby: Oh! I do not know, how hard will it be, but it is something very beautiful (laughter), yes, because you are creating a human being, that is motherhood for me, creating a human being and taking care of him (primigravida of first trimester, 27 years). For me it is a new experience, since I am primigravida I am learning (primigravida offirst trimester, 25 years). Having babies and taking care of them and attending to them (primigravida of secondtrimester, 16 years).
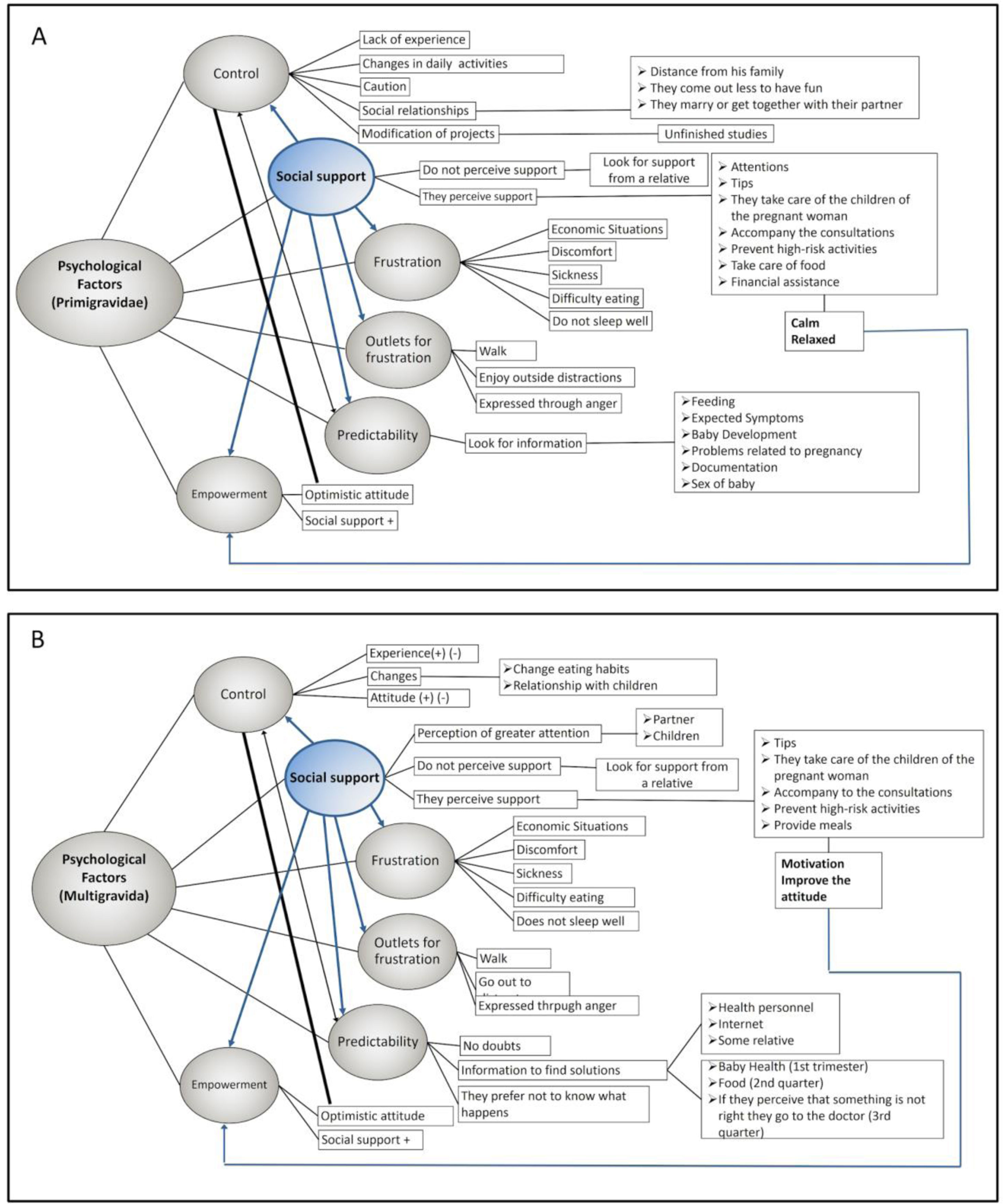
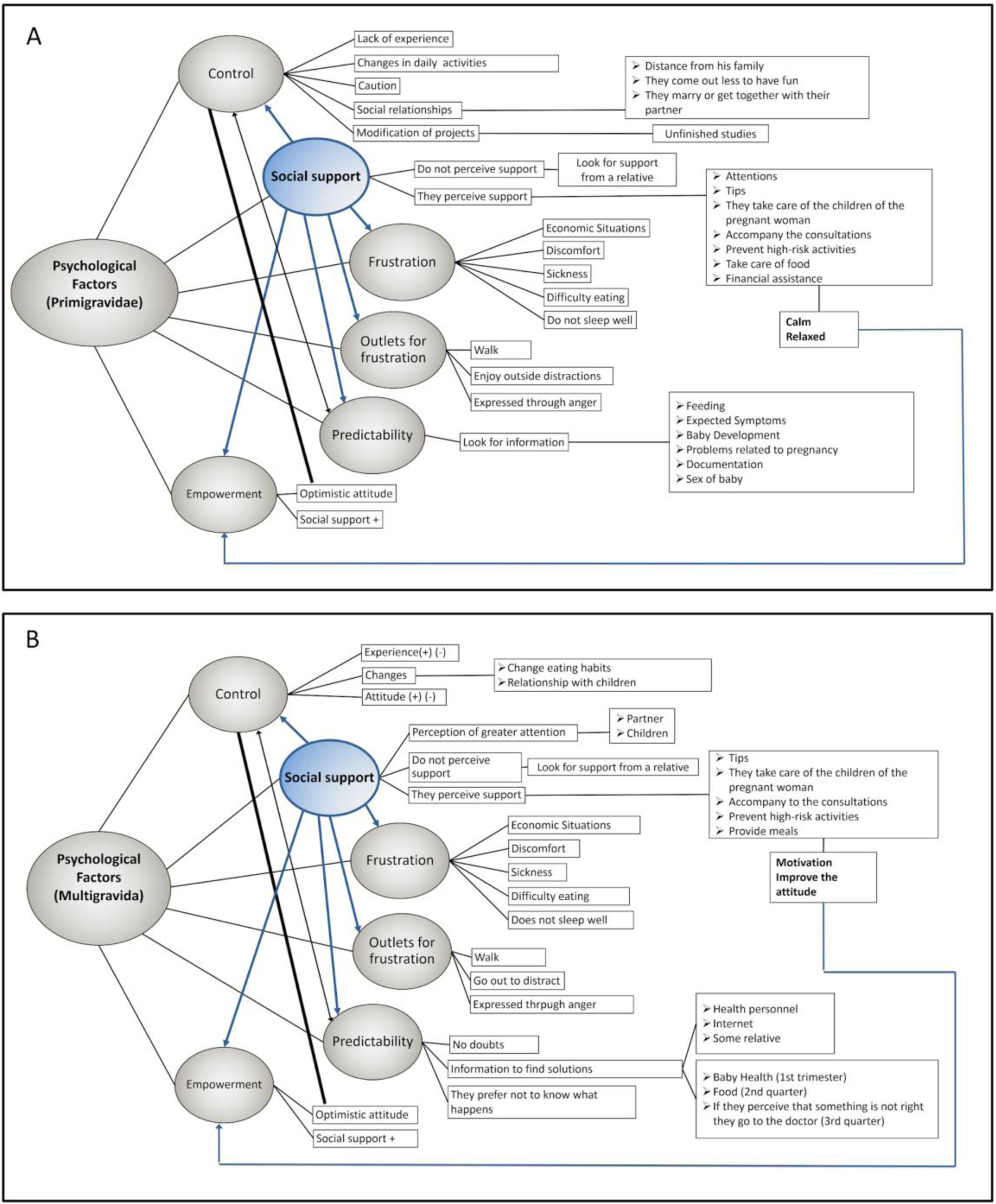
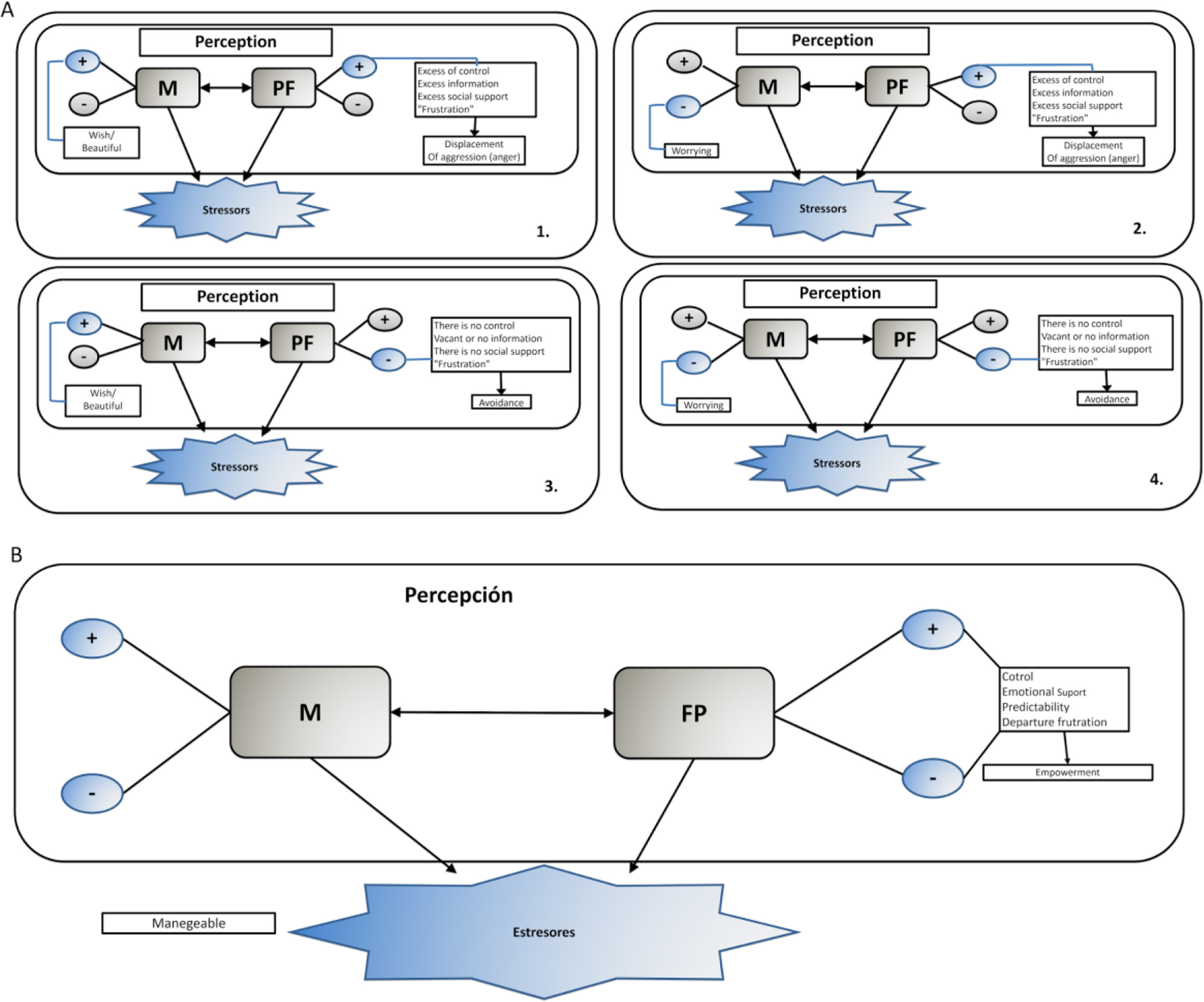
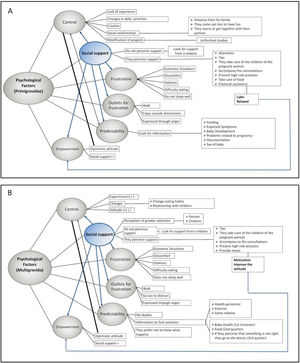
In general, it was observed that both the multigravida and the primigravida women presented similar stressors that are related to: physical and emotional states, health, age, previous experiences and those related to the baby (Fig. 1). The first stressors allude to the physical discomforts generated by the pregnancy changes (such as the belly (abdomen) growth that generates weight gain and itching). Although in this area (physical discomfort) it was observed that in each of the trimesters women reported the same changes that the literature refers to, where the primigravida manifested more discomfort than multigravida women. Well, it gave me a lot of headaches, nausea and dizziness (multigravida of first trimester 42 years). Mostly physical, my clothes do not fit me, obviously I had a lot of nausea (multigravida of first trimester, 23 years). Changes… well my belly is growing, and sometimes I had pain in my belly because of its growth, and itchiness when the belly stretches, I want to scratch (primigravida of thirdtrimester, 19 years).
In emotional stressors both groups manifested emotional fluctuations with the difference that the primigravida presented different and persistent emotions in each of the trimesters. For example, primigravida women reported feeling scared while they were on these first three months; while in the second and third trimesters they reported having an emotional sensitivity that tended to lean toward crying for no apparent reason, anger and sadness, and at the same time they reported feeling excitement and hope about having the baby. In contrast, the multigravida, even when they reported having different emotions ranging from happiness to irritability and depression, one of the emotions that they manifested most often was fear, especially in those cases in which women had presented problems in their previous pregnancies or because they had young children. Whether or not my baby is ok physically, I think this is the main fear (primigravida of first trimester, 27 years). I have had mood changes: I am feeling well and happy and for no reason I get angry, I do not understand how that happens; you are well and then you get angry or sad, the mood changes very suddenly (primigravida, of second trimester, 19 years). I get angry for no reason, I get sad for no reason, because of insignificant things (mulitgravida of the third trimester, 20 years). Sometimes I feel the joy of expecting another baby, but I am afraid because my other child is very young, he is only a year and three months old (multigravida of the second trimester, 33 years).
For the health category, multigravidas made reference to some risk factors such as nutrition or previous cesarean sections and age (although this was only referred to by women over 39 years old). All of these aspects were related to the information that they received from both family and doctors, for example: My sisters reprimanded me: look, you are old, you do not have the same strength as before (multigravida of first trimester, 39 years). I was worried because my other baby was born by cesarean section and the doctors told me that I had to wait two years minimum to get pregnant again (multigravida of second trimester, 23 years). I have had some infections and the doctors tell me that it can anticipate the delivery (multigravida of third trimester, 20 years).
For the primigravida in addition to the nutritional concerns, they also commented on feeling worried about the complications that they can have during the cesarean section and the probabilities of developing preeclampsia and/or gestational diabetes. I am concerned about having some complications in the cesarean section (pimigravida of first trimester, 16 years). I have been calm but they tell me that everything can change and that I may suffer hypertension or some other problem since I am the daughter of a diabetic father and my mother is hypertensive, so yes, I am concerned because I can get those diseases right now at the end of my pregnancy (primigravida of third trimester, 19 years). My family tells me that I have to eat well in order for my baby to grow healthy (primigravida of second trimester, 16 years).
Contrary to what we expected of multigravida women, the experience of having one or several pregnancies also proved to be a stressor, even when they mentioned that they had no doubts about their pregnancy, they expressed concerns about not knowing what to do or how to care for two or more children, especially those mothers who had small children (1 or 2 years old). Also when we asked another participant for her concerns when she knew that she was pregnant, she replied; these concerns were different with those women whose young children were happy with the arrival of the new baby. My daughter became very moody and gave me a very hard time when she made tantrums, or when she says that I will not love her anymore or, for example, my husband's family tells me that she is going to have more tantrums when the baby is born, and that stresses me (multigravida of first trimester, 23 years). My child is very young, he is only a year and three months old, and I do not know how I will take care of both (multigravida of second trimester, 29 years).
Contrary to what happens to those women who have children over the age of 6 and who are happy with the arrival of a new baby: I am calm, there are no struggles with my child, he is very happy with his little brother (multigravida of second trimester, 23 years). My daughters are happy and they are great, the oldest is in high school, they take good care of me and help me with the household chores (multigravida of first trimester, 33 years).
As for social stressors, it was found that those women who were minors or who still lived with their parents reported concerns about how they were going to tell their parents the news or what people would say. I waited like two and a half or three months to tell my parents I was pregnant. I was afraid of what they were going to tell me or how they were going to react (primigravida of first trimester, 15 years). How am I going to go out with this belly, what will people say (primigravida of first trimester, 16 years). More than anything I was worried about how to tell my parents. I told them the news when I was about two and a half months pregnant, I am 18 years old and yes, I had doubts about what they would say or how they would react, but then they reacted well and they support me (multigravida of second trimester, 18 years).
Another relevant aspect that emerged in this factor is that they reported having difficulty finding work due to their pregnancy and because of their age in the case of minors. They do not hire you when you are pregnant (primigravida of first trimester, 27 years). I am not prepared to have the baby. I need to work, but people do not hire me because I am under-age (primigravida of first trimester, 16 years).
Additionally, the people from whom they feel the most support when they have doubts or concerns are family members such as their partner, mother, sisters, and aunts. I talked with my partner about what is happening to me and he gave me the same advise as my mother (primigravida of first trimester, 15 years). Well, no one was born knowing how to be a mother, but I hope to put a lot of enthusiasm into it and to face all the problems that may come and be calm, since I am not alone: I have my partner, my parents and my sister who support me (primigravida of first trimester, 20 years). When I feel worried, I turn to my husband or my sisters (multigravida of first trimester, 42 years).
In the case of the baby-related stressors, the first and third trimester mothers-to-be reported feeling scared that the baby might be born with some illness or disability. Another thing that generated curiosity in them was the sex of the baby although none reported having any preference either way. In addition, the primigravida were not only concerned about the baby's health during pregnancy but also with the care that the baby would need when he or she was born, for example: I’m curious about the sex of the baby, and it scares me that they could be born sick (multigravida of first trimester, 23 years). I do not know what will happen after the baby is born, how am I going to feed him/her, how I have to bathe him/her, how I have to carry him/her, how will I educate him/her (primigravida of second trimester, 20 years). Sometimes I wonder how I am going to take care of him, if I am going to know how to take care of him (primigravida of third trimester, 27 years).
Finally, with regards to labor-related stressors, primigravida women reported being concerned that the scheduled birthdate was too early or they had doubts about what to do in case they could not feel when the birth time arrived, as well as their fear of pain. My family told me that at seven months the delivery could occur, this scares me because what if the baby wants to be born and I do not feel it. I am also afraid of the pain I can feel during childbirth, since people have told me that the pain is strong, or what if I repress the pain and something bad happens (primigravida of the third trimester, 19 years). I worry about the delivery since I do not know how the pain will be, if I am going to experiment pain or not, or if I am going to be well (primigravida of third trimester, 23 years). My first concern is about the delivery, about how it is going to be, I feel fear, sometimes I ask myself, will the baby arrive well? Or am I going to be well (primigravida of third trimester, 27 years).
Psychological factors were manifested in all pregnant women (Fig. 2). However, in each of the factors there were some differences between the multigravida and primigravida women and also in each gestational trimester. The results are shown as follows:
Control: It was found that in the multigravida the perception of control was influenced by the experience that women had in their previous pregnancies, such as if they had any pregnancy complications or if they had any loss (miscarriage or fetal death); and also if they perceived changes in their lifestyles, in their relationships, in their daily activities, or in their emotions. It was also observed that they use expressions such as to “do your best”, to “entrust themselves to God” and to “think that everything is going to turn out well” as a way of facing uncertain situations. This could favor the feeling of control. In my previous pregnancy my baby was born dead and because of that I am afraid that the same thing can happen to me again. Additionally, I have concerns about my age, it is not easy, but I commend to God, everything will turn out well and I will do my best (multigravida of third trimester, 42 years). When I have to face problems in my pregnancy, sometimes I put them aside since I realize that it is not good to worry about that, or to worry so much about things that maybe have a solution, or to be worried about something that sooner or later has to pass (multigravida of third trimester, 31 years). I cling to the idea of doing my best and I have faith that we are going to be well (multigravida of first trimester, 39 years).
On the other hand, this same group of women said that they felt ready to have another baby. Since they had already raised other children, they felt they could also succeed with this one. When I found out I was pregnant the first thing I thought was that I’m only going to start all over again, I will have the same pains, the same symptoms (multigravida of the third trimester 20 years). I do not feel prepared but if I have already raised the others, why wouldn’t I be able to raise this one (multigravida of first trimester, 42 years). I feel that no mom is ready to have a baby, right? my girl, thank God, is four years old and she has been a healthy girl until now, sometimes with tantrums, but I feel that I have done a good job and that I am prepared to have another baby (multigravida of first trimester, 23 years).
This was contrary to women who were in the second trimester of pregnancy, who said that they did not feel prepared and that they were very afraid of going through the experience of childbirth again. When I found out that I was pregnant I felt fear, because I had not planned it. Currently the only thing I am afraid of is the delivery (multigravida of second trimester, 29 years). Honestly, I cannot say that I feel prepared, I have fear. I don’t know if I going to make it with two kids (multigravida of second trimester, 33 years). I feel especially afraid about the moment of childbirth because I am going to have to live through it again but now, I know what they do to you when you have a baby (multigravida of second trimester, 23 years).
On the other hand, the primigravida stated that they did not to feel prepared to take on everything that the pregnancy entails. At the same time there were many women who commented that because of their pregnancy they had stopped doing activities that they normally would do, but there were also some women in the third trimester who mentioned that they continued carrying out their activities, however with certain precaution not to generate risks to the baby. Within the changes perceived by women were the shifts in their social relationships. I don’t think I am ready. I got married because I have no social security or anything, so he married me to give me that benefit and now I live with him and yes it has changed my entire life (primigravida of first trimester, 27 years). Well I think you are never sure enough that you are prepared, there always doubts about your ability to educate another person (primigravida of first trimester, 27 years). Well, no one is born knowing how to be a mother, but we hope to do our best and to face all the problems. Currently, I cannot do the same things as before, like have fun, because I have to take care of the person I am carrying inside (primigravida of third trimester, 23 years).
Social support: In general, it was observed that women tended to perceive more attention from their partners than from their family. For example, pregnant women receive advice and help from their partners in the form of care of the other children, companionship in the consultations, protecting the women from engaging in risky behaviors and taking care of their nutrition. My daughters help me a lot in the house, even though it is not their responsibility. The older one arrives from school and says to me: “mother have you already eaten, or I can make you a soup or something else”. They support me a lot, as much as my husband (multigravida of first trimester, 39 years). Until now everything is well with my husband, my children and my sisters, they help me, guide me and that makes me feel good, calm (multigravida of first trimester, 42 years). I am calm, there are no fights, my child is very happy with his little brother. My husband is a good man and now with the pregnancy he became even better (multigravida of second trimester, 29 years). They all support me, my partner, my mom and my mother-in-law. When I talk to them I feel good, they pay attention to me and give me advice (multigravida of third trimester, 20 years).
However, the primigravida also reported that they received so much attention that they sometimes felt overprotected. All attention is put on me, my dad and my mom all the time say to me “Eat breakfast, take lunch with you, it is time for dinner, you have to feed him” and so on. Everyone always says to me “You have to take care” (primigravida of first trimester, 27 years). The situation with my family is different, it is all about caring for the pregnancy, they do not let me go out so much, sometimes I feel overprotected (primigravida of third trimester, 20 years). Sometimes I feel that my family exaggerates a little taking care of me, they try to keep me from eating junk food, keep me from carrying heavy loads or climbing many stairs (primigravida of first trimester, 23 years).
On the other hand, multigravida women from the third-trimester reported that the support that they received from their families helped them to assimilate the fact that they were pregnant; it was also noted that some second-trimester women reported that when they did not receive support from their partner, it led them to have a negative attitude toward their pregnancy. I do not feel supported by my family. I feel alone, my partner did not support me in this pregnancy and that is why I start to feel depressed, sometimes I cry (multigravida of second trimester, 23 years). The situation with my family is bad because I have many problems with them and I think that hurts me, sometimes I think it was a wrong decision to get pregnant again (multigravida of second trimester, 18 years). Since my husband does not support me, I ask for support from an aunt, I tell her all my problems, I feel a little bit calmer after these talks with her (multigravida of second trimester, 23 years).
Outlets for frustration: At this point, women experienced frustration due to economic concerns or some physical discomforts such as nausea, in turn, some women expressed their frustration through anger; while some other women commented that when they feel frustrated they do some activities to distract themselves. Sometimes I feel despair, because I cannot sleep, my whole back starts to hurt and that frustrates me a lot (multigravida of third trimester, 20 years). I have been very frustrated by economic problems, sometimes I do not know what to do (multigravida of second trimester, 18 year). When I am frustrated I leave my house, go for a walk to see other people, I take my daughter to the park and then we buy a juice, or something like that (multigravida of first trimester, 23 years).
Primigravida women in the first and second trimesters reported that they take a walk or practice yoga in order to benefit the baby's health, to feel peaceful or for their wellbeing. The grandmothers said that if you walk a lot and drink a lot of water the delivery is easier, thus I go for a walk pretty often (primigravida of second trimester, 18 years). Now that I am pregnant I walk in order for my baby to be born healthy (primigravida of first trimester, 19 years). With so many mood changes, I decided to do yoga, this activity brings me peace (primigravida of first trimester, 27 years). If I going out for a walk I feel better (primigravida of first trimester, 28 years).
Predictability: Some multigravida women report that since they had been pregnant before, they did not have any questions about gestation; however, they also preferred not to understand what was happening. With this pregnancy I feel scared, in my other pregnancies I did not feel like this, thus I prefer to pretend that I do not know anything about what happens in pregnancy (multigravida of first trimester, 39 years). Well, since this is the fourth one I have no doubts (multigravida of second trimester, 39 years).
At the same time, they also commented that although they already had information about pregnancy, they tend to look for information when doubts arise, and women on the last trimester go to the doctor when they perceive that something is not well. Sometimes I ask the doctor if everything is okay or I go to the doctor if I feel that something is not right and he explains things to me (multigravida of third trimester, 20 years). When I consult the nutritionist I ask what foods I cannot eat, and to the doctor for things that I can take to feel calm or to get better from the stomach inflammation (multigravida of third trimester, 29 years). I searched for information related to the newborn, for example, about crib death, foot massages to help the baby sleep, things that I did not do for my other baby (multigravida of first trimester, 23 years).
It should be mentioned that in primigravida women, the type of information that they look for depends on the trimester in which they are. They all agreed that the information is obtained by consulting the Internet, books or brochures provided by the health center and friends who are doctors. I look for information about feeding and baby development (primigravida of first trimester, 25 years). I am looking for information about the problems that could occur during pregnancy, the problems that babies have, all the infections, everything about the moment of childbirth, what happens in childbirth, how many types of childbirth exist, what kind of paper work is needed before delivery, or where I should go (primigravida of second trimester, 20 years). I look for information related to pregnancy risks and the care of the baby (primigravida of third trimester, 23 years).
Empowerment: According to Sapolsky (2013) the individual's perception that a stressful situation can improve reduces the stress response, he calls this “capacity empowerment”. On pregnant women this factor was found in both groups and was observed to be related to the optimistic attitude that the woman acquires during her pregnancy. On the other hand, it was also observed that when women hear that the pregnancy is going well or when they begin to perceive the movements of the baby, despite the discomfort they experience, this gives them a sense of calm. I went to an appointment with the doctor and he told me everything was fine, that I have a normal pregnancy, so I feel calm (primigravida of first trimester, 25 years). The fact that my baby moves motivates me to go out and not think about what people say, I look forward to it with joy in order for the baby to feel that he is welcome (primigravida of second trimester, 18 years). Thank God I have been calm and I have not suffered any complication or disease (multigravida of third trimester, 23 years).
Due to stagnation observed in maternal and infant death rates (Aguirre, 2009), and its associations with gestational complications, the WHO has been given the task, through the Sustainable Development Objectives, to study the origin of these complications in order to combat the problem (WHO, 2018). Even when several studies have found that gestational stress is associated with some of the pregnancy, childbirth and the postpartum complications (Gangadharan & Jena, 2019; Goletzke et al., 2017), this association does not seem to be clear. That is, there are studies that find these links while others do not, in addition, this same association has been made with emotional states such as depression and anxiety (Weerth, van Hees, & Buitelaar 2003; Kramer et al., 2009; Sandman, 2006). With regards to all these discrepancies of the role of stress in pregnancy and the diversity of models that explain it (physical, psychological and social), the purpose of this study was to understand how pregnant women perceive motherhood, pregnancy stressors and psychological factors which in turn lead us to propose a better definition of gestational stress, and therefore more sensitive strategies to measure and combat it.
The results show an interaction of the three core factors of gestational stress. Motherhood is perceived as an ambivalent factor: on one hand, it is seen as something beautiful, on the other, there are a lot of concerns that seem to be translated into all the stressors encountered (physical, health, emotional, among others). At the same time, it can also be seen that psychological factors, with the exception of empowerment, show two polarities that, if left unbalanced, could alter the perception of stressors and thus affect the stress response.
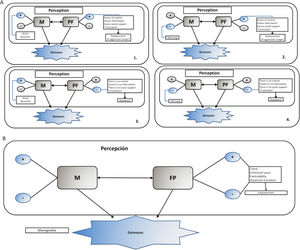
The perception of motherhood and the psychological factors are interrelated, as can be observed in figure 3, therefore according to the polarity (positive or negative) that they are perceived in, will be the perception of the stressors and the modulation of the stress response. For example, in box 1 of figure 3, the perception of motherhood tends to lean toward the positive pole (desire, beauty) and the psychological factors are manifested positively, thereby the denial of the negative pole of these two aspects causes an excess of control, social support and predictability, which synergizes between them and could intensify the sense of power. Thus, the intensification of positive perception and the denial of the negative one in this case could result in frustration manifested by aggression (anger).
On the other hand, box 2 of figure 3, shows how, when motherhood is perceived on the positive side and psychological factors are negative (women perceive no control, no social support and they do not have information or the information is vague), the stress response is not well managed, since releasing control completely implies that the pregnant woman is not doing what she needs to do, and the little information she may have is not enough to generate a coping strategy.
Similarly, the stress response is not good when motherhood is perceived in the extreme of the negative pole and is combined with the positive or negative perception of the psychological factors. That is, both polarities of the motherhood perception and psychological factors must be kept in a state of equilibrium. Being aware of these facts allows women to apply better coping strategies, which can be reflected in a sense of empowerment (see box 3 figure 3).
It is worth noting that social support is a psychological factor that is related to all of the other psychological factors; that is, social support in the form of care and advice that can be given to the pregnant woman, triggers the feelings of lack of control and predictability. In addition, frustration can be present as an avoidance of responsibilities or can be manifested as a passive coping strategy where the woman remains in a state of doubt or expectation. Empowerment, in the other hand, is a factor that seems to have only one pole that is reflected as an optimistic attitude and in a more active role in regard to her pregnancy. Therefore, when this factor is present it may be an indicator that pregnant women are coping with stress adequately. Finally, while social support seems to be the factor that connects all psychological factors, it is important to note that it generally generates empowerment, since otherwise women tend to be overwhelmed by the information they receive, express fear or concern when negative beliefs are confirmed, and if they do not feel this support they may even feel depressed.
As expected, we found that the three models of stress (physiological, psychological and psycho-social) are present during pregnancy, and they are linked closely. Thus, gestational stressors (physical, emotional, social, health related, and related with the baby and with childbirth) are only perceived and somatized when the pregnant woman assumes that she does not have the resources (psychological factors: control, social support, outlets for frustration, predictability) or when the resources she has are not enough to cope with stress and when the social construct of motherhood is negative. Therefore, the assessment of gestational stress should include these three aspects and how they are related and also a deeper understanding of the influence that the social construct of maternity has on the ways of perceiving pregnancy must take place. Regarding the social construct of motherhood, our results showed that becoming a mother generates ambivalence because it is perceived as a beautiful fact and at the same time a worrying situation, this observed ambivalence may be due to the social ideals that a woman faces, since she could be evaluated in her social environment as a “good” or a “bad” mother. Thus the “good mother” construct is defined by a series of qualities that she has to engage in and the more she covers them the “better” mother she will be. Some of these qualities are, for example, to possess a maternal instinct, maternal love, to be tolerant, patient and to have the capacity to console, care for, attend, listen to and protect, etc.; on the other hand, the “bad mother” is the denatured woman who goes against what is socially expected. In general, these last women are singled out or penalized depending on the severity of their non-compliance (Palomar-Verea, 2004). This is important since the degree of positivity or negativity with which maternity is valued will affect the perception of stressors and psychological factors. Also, the medical construct of pregnancy pretends to have control of what happens during gestation, this is reflected in the excess of attention and care that is given to the pregnant woman causing them to feel overwhelmed or even more worried. Regarding this point it should be noted that the social construct of motherhood is determined by three dimensions: gender and kinship, social organization and normativities, which are related to conceptions about the nature of the body, pleasure and the physiology of both pleasure and procreation. The dimension of gender and kinship refers to the way in which the couple's schemes and the exercise of a sexual life are organized; for example, the appropriate age for courtship and marriage, reproduction rate, the positive or negative evaluation of non-procreative sex or sex outside the conjugal bond. Social organization has to do with local traditions and economic conditions, which govern the hierarchical order of a society that establishes who has the right to do what and to whom, depending on the role that each one plays in society. Finally, the norms established mainly by legal codes and religious precepts that have the function of indicating the behaviors that are morally adequate according to gender, age and socioeconomic status (Córdova, 2003). As must be noted, the social construction of motherhood follows an order and stable status of what is right and what is not, placing the woman in a situation of struggle between what she wants and the ideals that society expects her to achieve.
On the other hand, with regard to the differences between primigravida and multigravida women, it was found that the former see motherhood as a process in which they are acquiring a technique for how to care for the baby, while the latter see it from a more personal or developmental scope, that is, how they feel about having another baby.
With regards to the Lazarus and Folkman theory (1986) and according to the emotions identified in each of the groups, it could be inferred that since multigravida women made more allusion to fear, they tend to evaluate pregnancy as harmful, as loss or as a threatening event. However, in the primigravida this valuation seems to be changing every trimester.
In this study we also found that stressors are typical of pregnancy: physical, emotional, social, health related, related with age, those related to the baby and childbirth. This is of great importance since most studies that measure gestational stress use psychometric instruments built for the general population (men and women) and at other stages of life (Brouwers, Van Baar, & Pop, 2001; Davis et al., 2004; Harville, Savitz, Dole, Herring, & Thorp, 2009; Kramer et al., 2009; Paarlberg et al., 1999; Salacz, Csukly, Haller, & Valent, 2012). In addition, within the emotional stressors, although both groups of women (primigravida and multigravida) reported feeling fluctuations and emotional liability, it is observed that primigravida perceive different emotions according to the trimester of gestation in which they are found; whereas in multigravida women, fear was an emotion that persisted throughout gestation. The latter seems to indicate that knowing what is happening in pregnancy and knowing the responsibility that comes with having a child, generates more fear than not having the experience of being pregnant. As reported by Sapolsky (2013), the stressful effects have to do with subjecting the organism to a novelty, however believing that we know how to deal with things and what will happen afterwards causes a state of alertness and excitement in order to avoid mistakes. It is also observed that women on the first and second trimesters mentioned more emotions than those in the last trimester, which seems to indicate that their emotions fluctuate more or in any case, that they are more aware of their emotions, or that there is a process of habituation. Also, in the primigravida women it was observed that social stressors could be related to the support they perceive from their families, this having greater importance in the younger mothers.
With respect to psychological factors, it was observed that during pregnancy that all factors are present and that the way in which they are manifested can attenuate or increase the stress response. For example, in terms of control and predictability, it seems that these factors require a degree of flexibility since not having them or having them too much generates a greater stress response. On the other hand, empowerment is favored by the attitude toward pregnancy and social support. Also, these psychological factors are not only present and change the response of the pregnant woman to stress, but they are all related. For example, many of the multigravida women said that since they knew what it means to be pregnant, they preferred not to know what was happening. It seems that this is a way of letting go of control in pregnancy and they then felt less guilty if there was a complication. According to Sapolsky (2013) when a person believes that he or she has a certain degree of control over an inevitable stressor, it can lead them to the belief that they are guilty in the face of an unexpected situation. On the other hand, it has also been observed that women who have a strong sense of internal control have a greater stress response than those who assume their limitations in the face of an uncontrollable event. Furthermore, it was observed that one of the psychological factors that most influence women to having a positive attitude toward their pregnancy was social support. In that respect it was interesting that women who did not receive social support from their partner manifested the emotions of depression, loneliness and despair, as well as an attitude of disdain for the information they received and what happened during pregnancy. Likewise, it was observed that the information provided by the social support network (family and health personnel) seemed to be generating stress. According to Sapolsky's works, the outlets for frustration can be given as a displacement of the aggression or as something more positive for the person, that is, something that helps the subject to re-signify that there are more positive things than the stressful event that is being experienced. In pregnant women, both multigravida and primigravida, outlets for frustration seem to be related to anger and irritability (displacement of aggression) and tend to be more present in the first and second trimester, which is where there are several physical discomforts such as nausea and sleeping difficulties.
Finally, when we analyzed gestational stress according to the gestational trimester, differences were observed in the perception of stress according to the type of stressor and the psychological factor presented. For example, it was generally observed that the second trimester is a period in which multigravida women reported that even when they feel prepared to have a baby, they have fear and even depression. It was interesting that this group of women does not perceive having social support. This situation is noteworthy since, according to several studies, the second trimester is a period of physical and emotional stability for pregnant women (Aller & Pagés, 1999; Gaviria, 2006; Gómez-López, Aldama-Calva, Carreño-Meléndez, & Sánchez-Bravo, 2006; Guyton & Hall, 2005; Maldonado-Duran, Sauceda-García, & Latirge, 2008; Moore, Persaud, & Shiota, 1996; Purizaca-Benites, 2008), however, our findings seem to contradict this assertion.
In summary, this qualitative study shows that even if pregnancy is an event that involves several sources of stress or stressors, the intensity in which these stressors are experienced and the way in which they are maintained over time depends on the quality of the psychological factors that the women have to cope with stress. In other words, during pregnancy, these psychological factors are able to modulate stress since through them women develop the capacity to keep their physiology in equilibrium, and therefore the psychological factors might improve or worsen the gestation process.
It is important to point out that our study has some limitations. The fact that the interviews were conducted in the hospital prevented a more in-depth study of the variables. Furthermore, these findings may not be generalized since all the women interviewed came from a low-income status and they included only those women who visited a specific public health service. Therefore, it will be important in future studies to analyze whether this result applies to women with a different socioeconomic stratum and/or those who visit another kind of health service.
Authors’ contributionsTRG and RGO conceived of the study and participated in its design, analysis and coordination. DMSS design the figures. RGO and TRG drafted the manuscript together. RCP, MRHP and ABE conducted a critical review of the manuscript. All authors read and approved the final manuscript.
Conflict of interestThe authors declare that they have no conflict of interest.
RGO is recipient of doctoral fellowship from CONACYT. Sara Robledo Waters proofread all the manuscript.