Adherence to pharmacotherapy reduces symptoms of asthma and rhinitis, however, little is known of its impact on school performance.
ObjectiveTo evaluate the impact of pharmacotherapy in absenteeism and school performance in a child population.
MethodsA cross-sectional study, carried out in eight schools. All participants and their parents were given a questionnaire assessing parameters related to respiratory diseases and pharmacotherapy. Data on school performance was obtained from the academic history of each child who participated in the study. Adherence to pharmacotherapy was classified as a correct use of therapy for more than five days per week.
Results1109 children agreed to participate. Students were divided into two groups: symptomatic (36%) and asymptomatic (63%). The symptomatic group had a higher frequency of school absenteeism (1 vs. 3.1days/year/patient p<0.01) and lower academic performance (failed: 20% vs. 33% p<0.01). After dividing the symptomatic group between adherents and non-adherents to the pharmacotherapy, the group of adherents had a similar school performance to the asymptomatic group and it was significantly different from the no-adherent group.
ConclusionRespiratory symptoms are associated with poor school performance and with an increase in school absenteeism, but adherence to pharmacotherapy can reduce these negative impacts in children.
Several studies have shown the high prevalence of asthma and rhinitis worldwide, especially in children.1–6 These diseases have an important detrimental effect on the quality of life, as they alter the personal development and lifestyle of patients and their families.7,8 Several studies have shown the social impact of these diseases.9,10 Lack of clinical control could potentially lead to lack of concentration, poor school performance and school absenteeism. So far only few studies have investigated the impact of asthma and/or rhinitis on school performance.
The efficacy of pharmacotherapy in controlling allergic respiratory diseases has been demonstrated in several studies.11–13 However, it has not been studied whether if the negative impact for children in the process of learning can be recovered with adequate pharmacological treatment.9 In addition, as chronic diseases, they require prolonged management, which makes an adequate adherence difficult.
In a previous study,12 we observed that those children of school age who had asthma and/or rhinitis had, in comparison to children without respiratory diseases, more absences in school and lower school performance. In this article, taking into account the positive impact of pharmacotherapy on the control of symptoms of respiratory diseases such as asthma or rhinitis, we seek to explore whether pharmacological treatment can reverse the negative impact of these diseases in the learning process of children.
MethodologyPopulation and study designThis is a cross-sectional descriptive study. We included children over six years old of eight schools in two cities of Colombia (Medellin and Cartagena). Through medical records and questionnaires based on the ISAAC study, the ARIA guidelines and the GINA guidelines (www.ginasthma.org), we obtained information on the presence or absence of respiratory diseases and other chronic diseases, pharmacological treatment and severity of symptoms. Data were collected by the investigators from all families who agreed to participate, however, we used the Charlson Comorbidity index,14 to exclude patients with severe chronic comorbidities that could overestimate the severity of symptoms for causes other than the diseases studied and might influence the interpretation of the results.
Data on school performance in the previous school year was obtained from the academic history of each child who participated in the study. For the evaluation of the primary outcome (clinical impact of respiratory diseases in school performance), we used as measurement variables the number of absent days, the average grade of students in Mathematics and Spanish during the last academic year. Mathematics and Spanish have the same academic curriculum among the schools, so they were selected to evaluate school performance. Moreover, they are academic areas that use similar objective evaluative parameters for their grading in all schools. To present the academic score in the eight schools, we unified the results using a semi-quantitative scale: >80% (Excellent performance according to the scale of each school), 60–79% (average), and <60 (insufficient). For school absent days we took into account only those related to health issues that could be directly or indirectly related to the diseases we studied. We excluded absent days due to vacations, permits for non-medical procedures, etc.
To evaluate the secondary outcome (clinical impact of pharmacotherapy in school performance), we performed a stratified analysis among patients with respiratory diseases (asthma and/or rhinitis), according to whether the patient was receiving pharmacotherapy and if so, whether they had good adherence or not. We classify as good adherence patients who received treatment at least five days per week according to medical recommendations taking into account previous data.12
Ethical considerationsAll parents signed an informed consent (with the child's consent) authorizing the review of the academic data kept by the institution, the medical records and also agreed to complete the questionnaire. The ethics committee of the University of Cartagena evaluated and granted permission to carry out the present study.
Statistical analysisFor the primary analysis, we divided the children between symptomatic and asymptomatic according to the presence or absence of symptoms of asthma or rhinitis. For the secondary endpoint we divided the group of symptomatic into two sub-groups between adherents and non-adherents. In Colombia the evaluation of Mathematics and Spanish subjects have the same objectives, and the same parameters are used in all schools, so we do not expect that variables in the system of qualification could influence the results. However, we conducted intergroup analysis in each school to identify other factors that could influence school scores that were different from the study objectives.
A sample size calculation was performed based on the probabilities difference technique (x2 test) with Yates continuity correction by the Fleiss formula. A Type I error of 0.05 was chosen; a Type II error of 0.20; a confidence level of 95%; we estimated a proportion of cases of rhinitis of 30% and of asthma of 12% based on previous studies carried out in this area; with an expected number of two controls per case. Therefore, a minimum sample size was obtained for the cases of 312 patients and for the controls of 628 patients.
The analyses were performed using the SPSS software version 21 for Windows using the Wilcoxon U test for intergroup analysis, Mann Whitney for intragroup and the T test for mean differences in independent samples. A p<0.05 was considered statistically significant. For analysis of multiple comparisons, we used the Dunn test. The proportions were analyzed using contingency tables and the Fisher exact test.
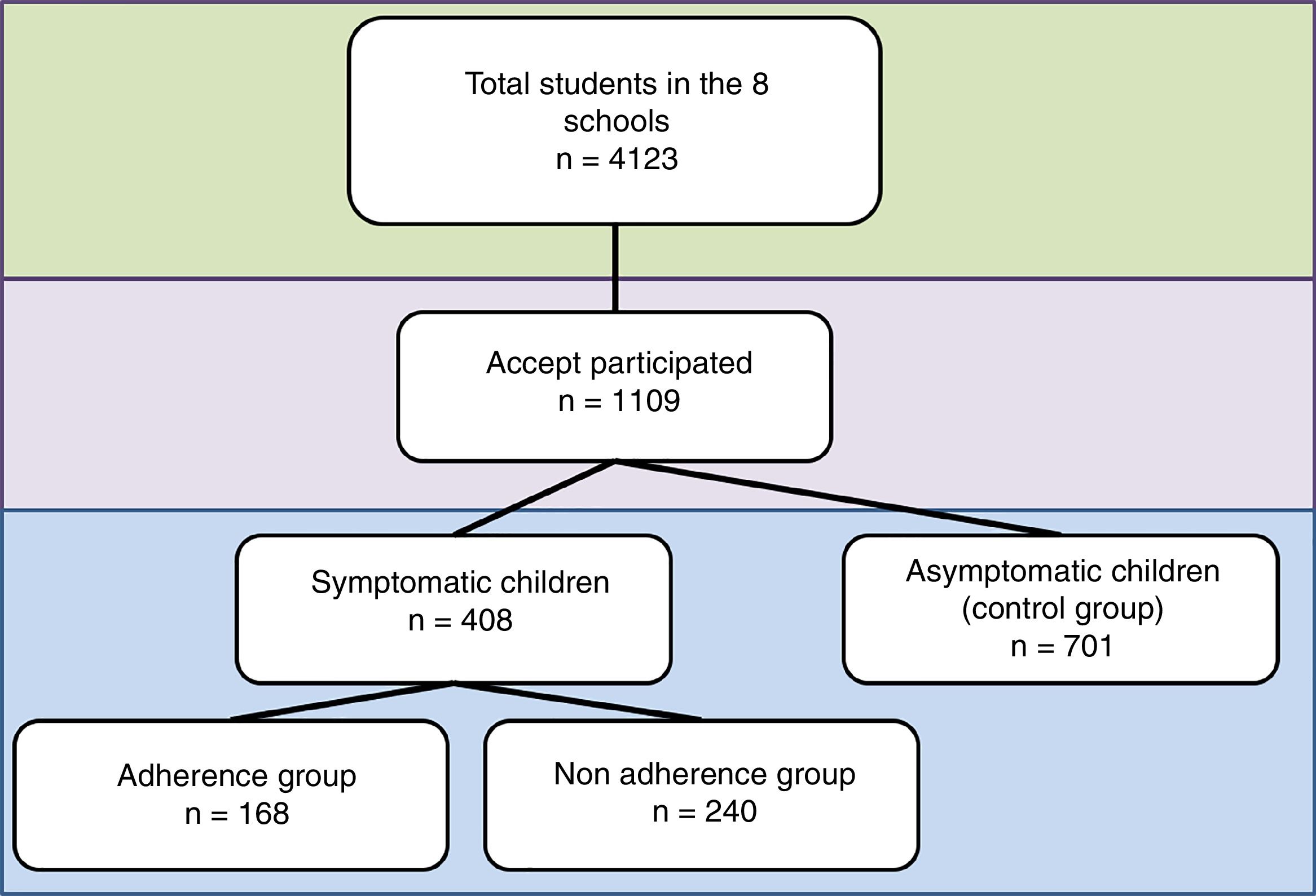
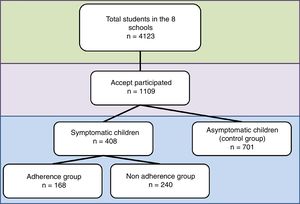
ResultsThe eight schools had a total of 4123 students. A total of 1109 children and their parents agreed to participate and were included (Fig. 1). 300 children who agreed to participate were not included for different reasons: (1) incomplete data in the clinical history (n 180); (2) abandonment of the school institution during the evaluation period (n 55); (3) suffering from other chronic comorbidities that could affect the evaluation of the primary objective of the study (n 65). The socio-demographic characteristics of the excluded patients were similar to the patients who remained in the study.
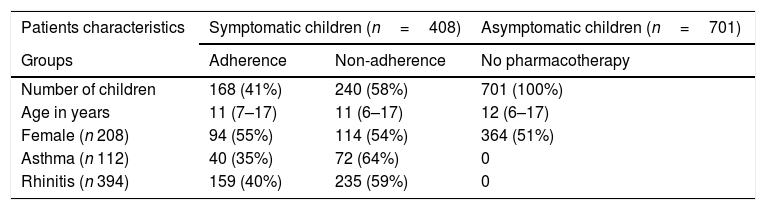
Description of subjectsA total of 408 patients had asthma (n=112) or rhinitis (n=394); taking in consideration that 94% of patients with asthma also had rhinitis, we decided to treat the sample as a single group (Table 1) and it was divided into patients who were adherent or non-adherent to pharmacotherapy. According to ARIA guidelines classification, among patients with rhinitis 66% had “persistent moderate/severe rhinitis”, 30% “persistent mild rhinitis” and 4% “intermittent rhinitis”. According to ISAAC questionnaire 17% of patients had “persistent severe asthma”, 33% “persistent moderate asthma”, 23% “persistent mild asthma”, and 27% “intermittent asthma”. A total of 701 patients were included in the asymptomatic group.
Characteristics of the patients.
| Patients characteristics | Symptomatic children (n=408) | Asymptomatic children (n=701) | |
|---|---|---|---|
| Groups | Adherence | Non-adherence | No pharmacotherapy |
| Number of children | 168 (41%) | 240 (58%) | 701 (100%) |
| Age in years | 11 (7–17) | 11 (6–17) | 12 (6–17) |
| Female (n 208) | 94 (55%) | 114 (54%) | 364 (51%) |
| Asthma (n 112) | 40 (35%) | 72 (64%) | 0 |
| Rhinitis (n 394) | 159 (40%) | 235 (59%) | 0 |
From the symptomatic group, 97% had a previous diagnosis of asthma and or rhinitis during the school period that was evaluated; 3% were diagnosed during this study. 93% of patients had a pharmacological treatment according to clinical management guidelines, however, a high proportion of them did not have adherence to the therapy recommended by their doctor for asthma (35% vs. 72% p 0.02) or rhinitis (40% vs. 59% p<0.01).
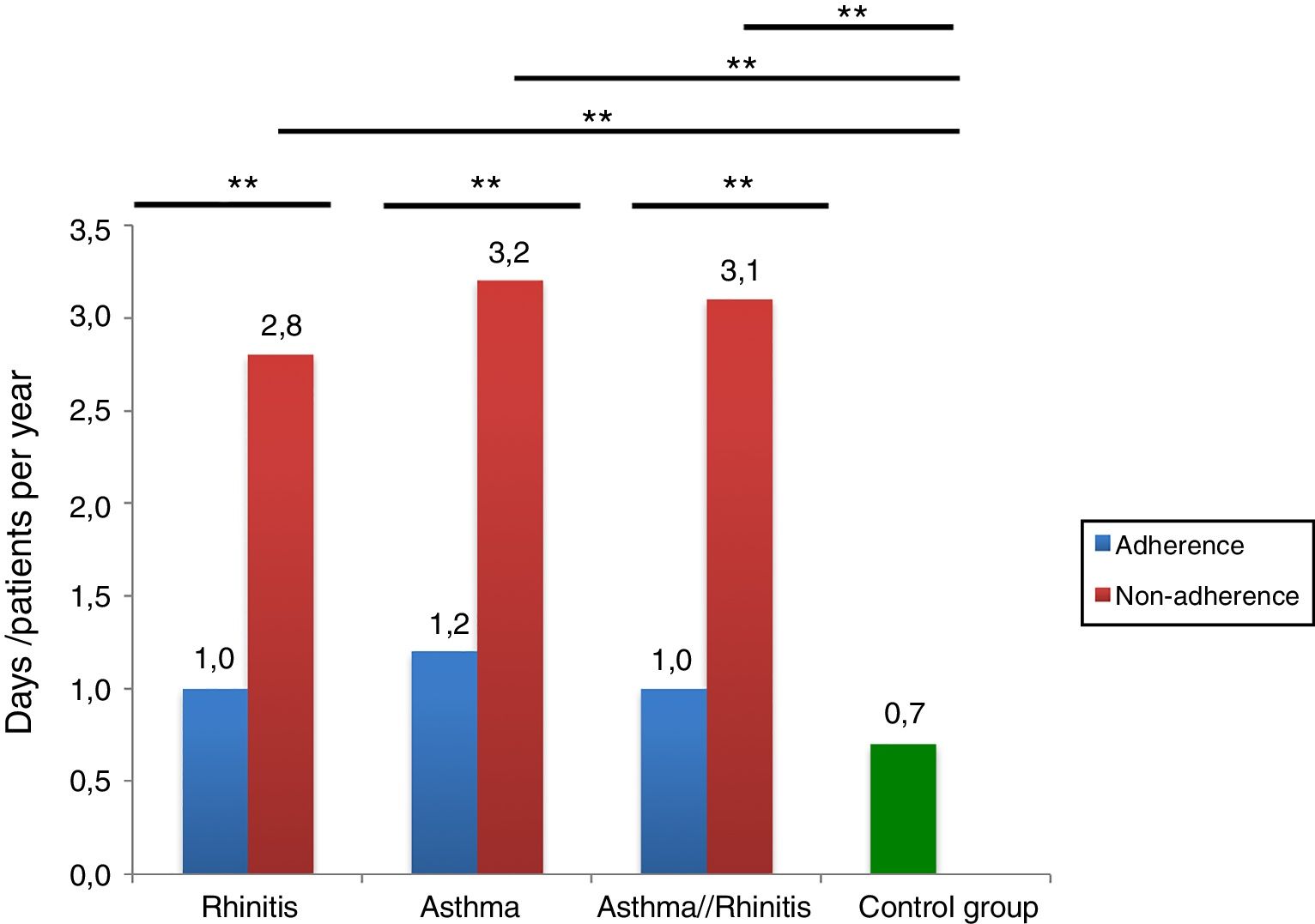
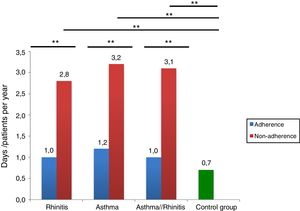
Absenteeism and pharmacotherapy impactThe main cause of absenteeism was associated with acute illnesses like rhinitis exacerbation (39%), asthma exacerbation (18%) or medical control consultation (27%).
Fig. 2 presents absenteeism according to days/year by number of people in each group. In the symptomatic group, the frequency of absenteeism was higher in comparison to the asymptomatic group. Among the symptomatic group, we observed that those children receiving pharmacological treatment with good adherence, presented lower absenteeism due to allergic diseases compared to those who did not receive it continuously (day/year/patient: 0.8 vs. 3.1 p 0.02). Patients in the adherent group had no statistically significant differences in frequency of absenteeism compared to the asymptomatic group (Fig. 2).
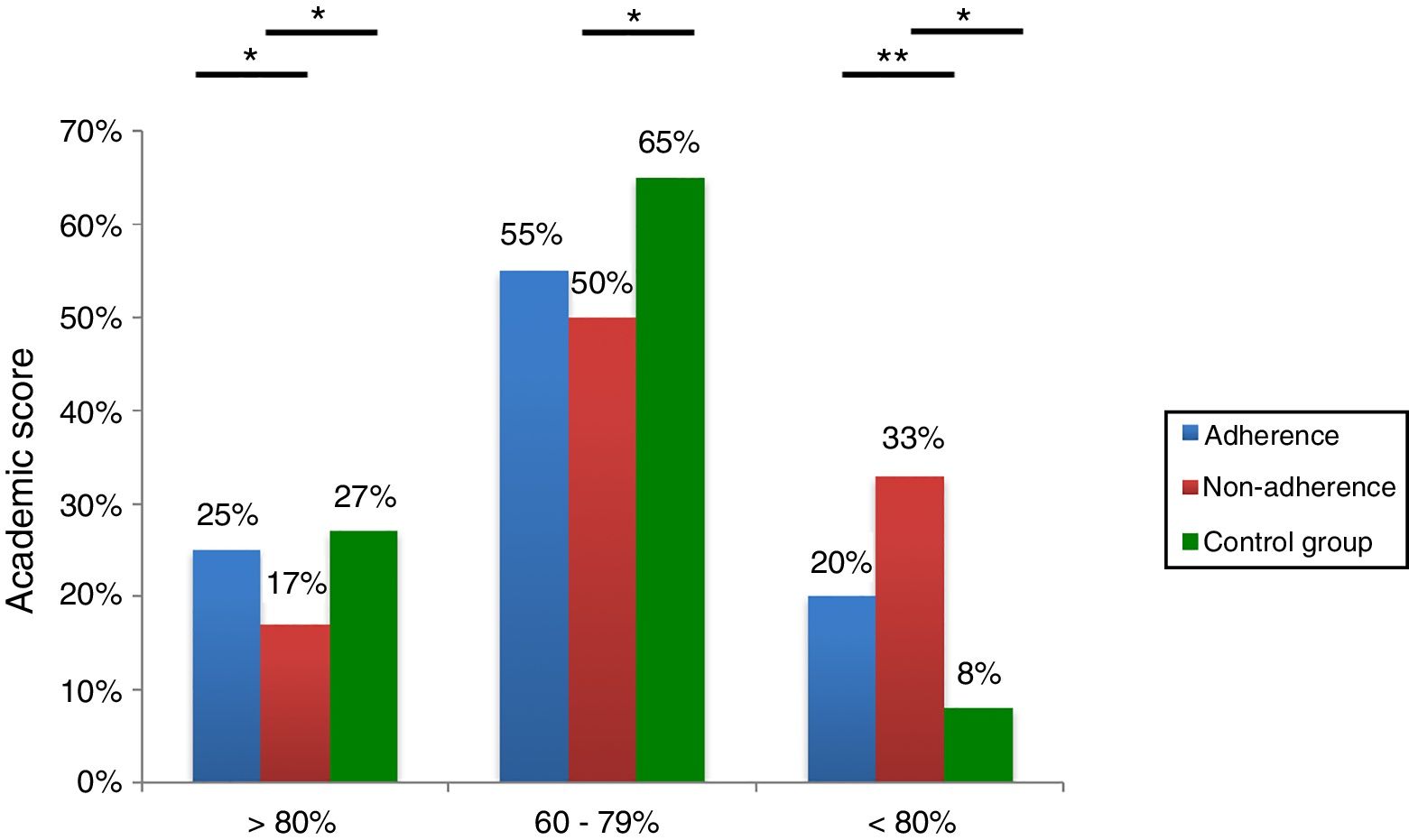
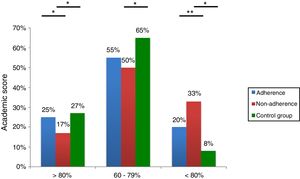
School performanceRegarding school performance, in the symptomatic group it was observed that the number of students with insufficient score (<60%) for Mathematics and Spanish was higher than in the asymptomatic group (Fig. 3). There were no significant differences between the two areas or among the eight schools. Patients with adequate therapy and adherence had better performance than patients who did not receive continuous treatment and were similar to the asymptomatic group. There were no significant differences between patients with asthma or rhinitis.
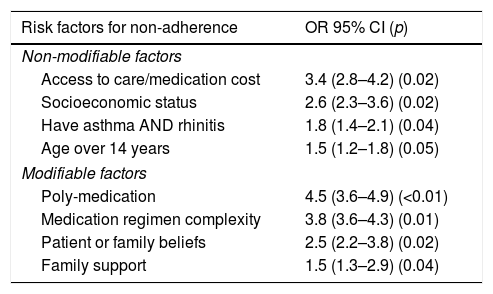
No adherence risk factorsWhen we analyzed the adherent and non-adherent groups, some risk factors were identified as possible causes for non-adherence (Table 2). The main non-modifiable factors were access to the healthcare system/cost of medication, and socioeconomic status. The principal modifiable factor was poly-medication.
Risk factors for non-adherence. Risk factors were classified according to being modifiable or non-modifiable.
| Risk factors for non-adherence | OR 95% CI (p) |
|---|---|
| Non-modifiable factors | |
| Access to care/medication cost | 3.4 (2.8–4.2) (0.02) |
| Socioeconomic status | 2.6 (2.3–3.6) (0.02) |
| Have asthma AND rhinitis | 1.8 (1.4–2.1) (0.04) |
| Age over 14 years | 1.5 (1.2–1.8) (0.05) |
| Modifiable factors | |
| Poly-medication | 4.5 (3.6–4.9) (<0.01) |
| Medication regimen complexity | 3.8 (3.6–4.3) (0.01) |
| Patient or family beliefs | 2.5 (2.2–3.8) (0.02) |
| Family support | 1.5 (1.3–2.9) (0.04) |
Asthma and rhinitis are chronic diseases with high prevalence. Their impact on health and socio-economic status is high.15 For this reason, they represent a public health problem and it is necessary to evaluate its impact on the patient, their family and social nucleus.
Similar to what was previously observed in Europe and the United States,8,16 we observed that rhinitis and asthma are an important cause of absenteeism and poor school performance. Additionally, our results indicated that adequate treatment in these patients allows a better symptomatic control, which also significantly improves the academic performance of the patients, achieving similar results to asymptomatic children.
Economic Evaluations (EEs) show that the necessary drug therapy required for proper control of rhinitis and asthma has a high economic cost for the patient and the healthcare system; these costs are even greater when there is no clinical control because patients have to attend the emergency department and in addition, school and work absenteeism increases. All EEs agree that the cost is greater for the patient, since they are the ones who assume the direct and also indirect costs of the disease, which according to some studies represents the greater part of the expenses associated with rhinitis and asthma.13 Our results indicate that pharmacotherapy leads to better symptomatic control and that most patients have access to it, but the adherence rate is very low. We identified some factors that could explain the low adherence to treatment: the main non-modifiable factors were access to the healthcare system/cost of medication, and socioeconomic status, both associated with accessibility to medication. We also observed that modifiable factors added a greater risk of non-adherence, which is important because they can be modified during the medical consultation, but promotion and prevention campaigns are necessary to enable a greater awareness of the problem to the patient, their family and their medical doctor.
Similar to our results, among the few studies on the subject, Velástegui et al. observed in Chile that school patients with severe asthma have up to twice the health-related economic expenses compared to non-asthmatic subjects and also higher school absenteeism.15 Another form of loss is incurred by “presenteeism”, a term used to describe the phenomenon of ill employees who show up for work but cannot perform effectively, but this is more but to assess and it is usually not registered.17 This type of assessment should be done in each region taking into consideration its healthcare system and its particular social and economic situation.
The selection of Mathematics and Spanish as parameters of evaluation of school performance has some limitations; the variability in the educational strategies used, and the students’ skills could influence the results of the scores. However, these variables are compensated by the fact that all children included in each school were subject to these variables and the differential variable was the presence or absence of respiratory symptoms. In addition, the best performance among all children with asthma and/or rhinitis receiving medication compared to those who were untreated reinforces the hypothesis that the decrease in productivity found among children with respiratory diseases was largely due to disease and not to other factors such as the evaluation methodology of each institution.
In summary, we observed that rhinitis and asthma are important risk factors for school absenteeism and poor school performance in the child; however, the impact of these diseases can be reduced with appropriate treatment. It is necessary to carry out promotion and prevention programs to make patients, physicians and healthcare institutions aware of the importance of good clinical control of these diseases.
FundingThis work was supported by the Group of Clinical and Experimental Allergy, IPS Universitaria, and the University of Antioquia.
Conflict of interestThe authors declare no conflict of interest.
To the students, teachers and other members of the school institutions who collaborated in the study. To Javier Estarita and Carolina Salemi for data collection.