To compare intraoperative ureteral injuries in RIRS with UAS insertion with the rate of postoperative infections after RIRS without UAS insertion.
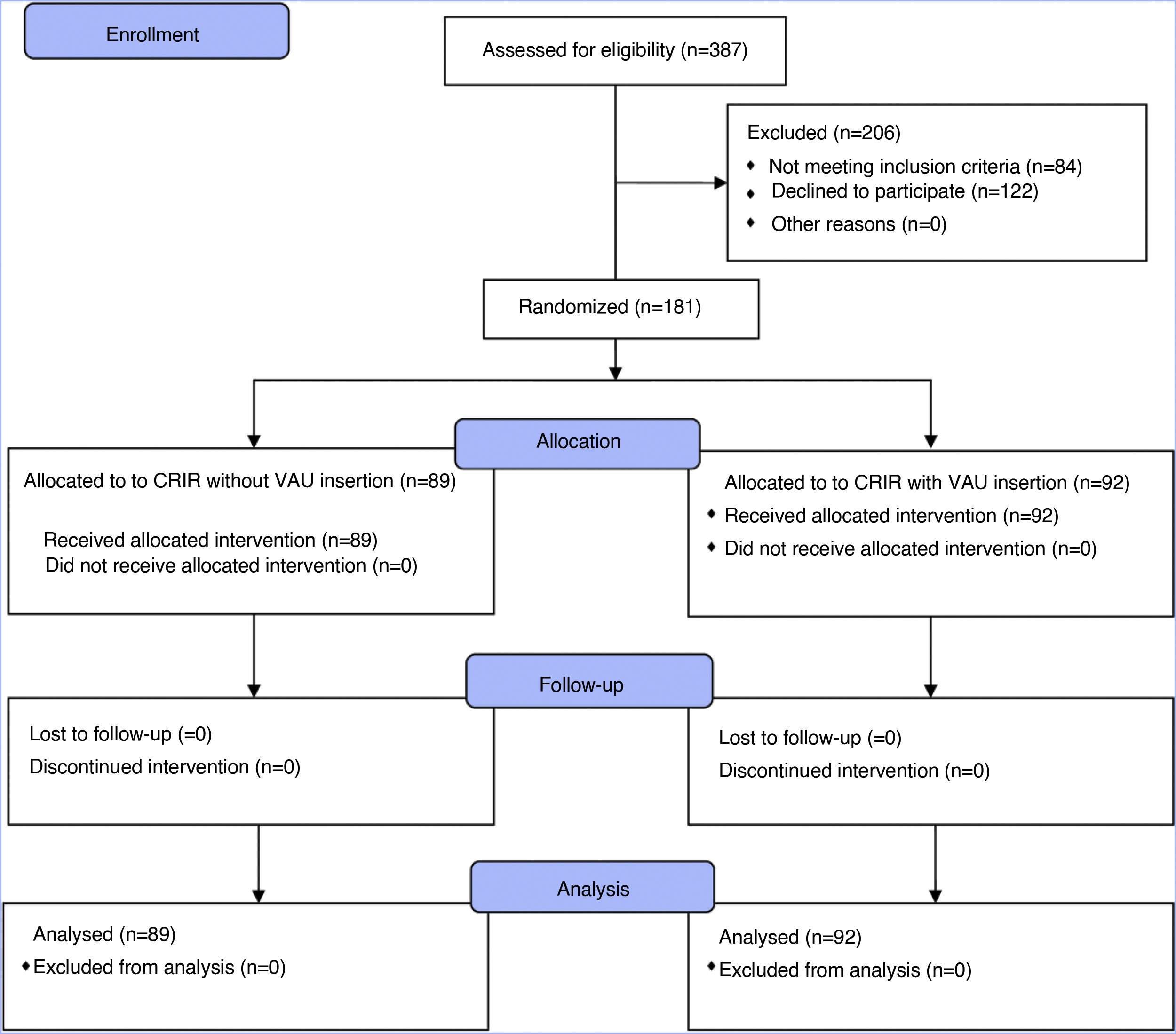
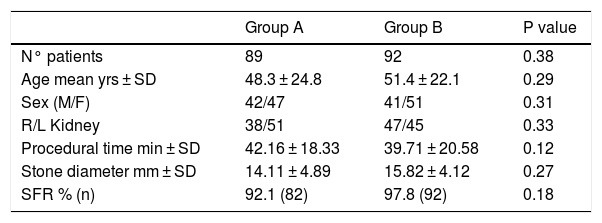
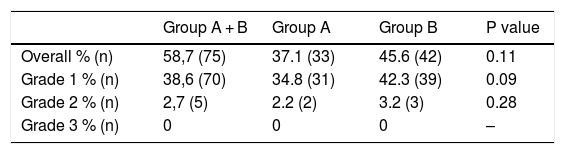
Patients and methodsIn this randomized trial, patients who received an indication for RIRS between January 2017 and December 2017 were divided into two groups. Group A had no UAS insertion and Group B had UAS insertion. Post-Ureteroscopic Lesion Scale (PULS) grading was performed after UAS or flexible ureteroscope removal. Proximal, middle and distal ureteral lesions were evaluated and compared according to the PULS scale. Additionally, patients in both groups were followed postoperatively to assess any infective complication.
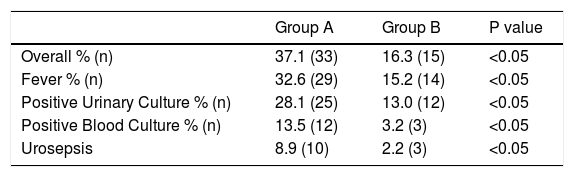
ResultsThe evaluation comprised 181 patients, 89 for group A and 92 for group B. Overall stone-free rate, clinically insignificant residual fragments, and final stone-free rate were 41.4%, 53.5%, and 95%, respectively. There were 33 (37.1%) patients with ureteral lesions in group A while 42 (45.6%) patients had ureteral lesions in group B, with no significant difference. On the other hand, the overall presence of postoperative infection rate was much higher for Group A (37.1% vs 16.3% P = 0.03).
ConclusionsUAS insertion does not result in a higher number of ureteral injuries. UAS insertion during RIRS allows a lower rate of postoperative infections.
Clinical Trial Registration Number (ISRCTN registry number)55546280.
Comparar las lesiones ureterales intraoperatorias ocasionadas durante la CRIR con inserción de VAU con la tasa de infecciones postoperatorias tras la CRIR sin inserción de VAU.
Pacientes y métodosEn este ensayo aleatorizado los pacientes que recibieron una indicación de una CRIR entre enero de 2017 y diciembre de 2017 se dividieron en 2 grupos. En el grupo A no se utilizó VAU y en el grupo B sí se utilizó VAU. Se realizó la clasificación de la escala Post-Ureteroscopic Lesion Scale (PULS) tras retirar la VAU o el ureteroscopio flexible. Las lesiones del uréter proximal, medio y distal se evaluaron y compararon según la escala PULS. Además, los pacientes de ambos grupos recibieron seguimiento postoperatorio para evaluar el desarrollo de cualquier enfermedad infecciosa.
ResultadosEl estudio incluyó a 181 pacientes, 89 del grupo A y 92 del grupo B. La tasa de ausencia de cálculos global, los fragmentos residuales clínicamente insignificantes y la tasa de ausencia de cálculos final fueron del 41,4%, 53,5% y 95%, respectivamente. Hubo 33 (37,1%) pacientes con lesiones ureterales en el grupo A y 42 (45,6%) pacientes con lesiones ureterales en el grupo B, sin diferencias estadísticamente significativas. Por otra parte, la tasa de infección postoperatoria fue mucho mayor en el grupo A (37,1% frente a 16,3% p = 0,03).
ConclusionesNo se ha visto un mayor número de lesiones ureterales tras la inserción de la VAU. La inserción de una VAU durante la CRIR resulta en una tasa menor de infecciones postoperatorias.
Número de registro del ensayo clínico (número de registro ISRCTN)55546280.