Minimally invasive surgery represents an attractive surgical approach in radical cystectomy. However, its effect on the oncological results is still controversial due to the lack of definite analyses. The objective of this study is to evaluate the effect of the laparoscopic approach on cancer-specific mortality.
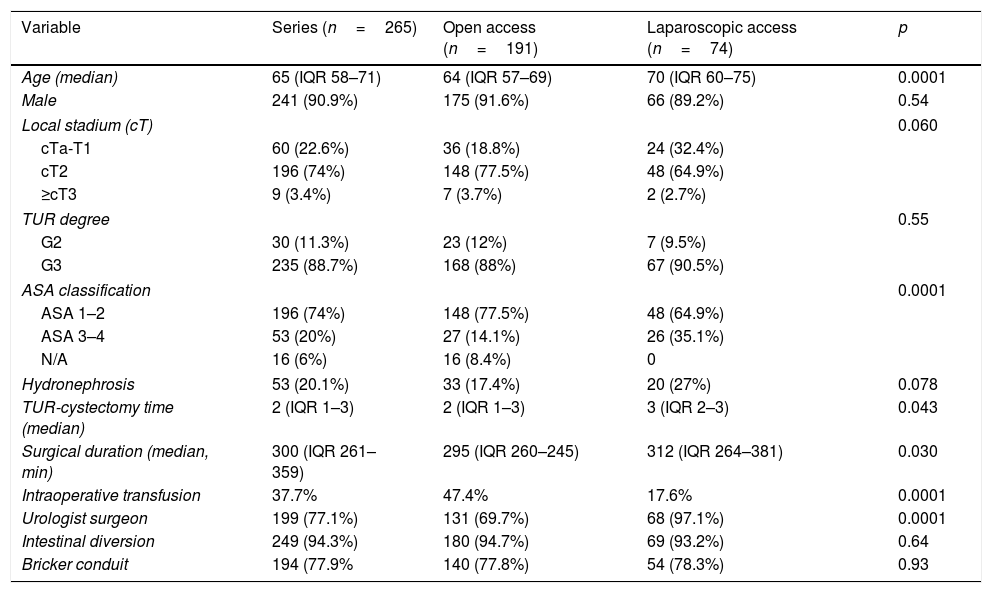
Material and methodA retrospective cohort study of two groups of patients in a pT0-2pN0R0 stage, undergoing open radical cystectomy (ORC) (n=191) and laparoscopic radical cystectomy (LRC) (n=74). Using Cox regression, an analysis has been carried out to identify the predictor variables in the first place, and consequently, the independent predictor variables related to survival.
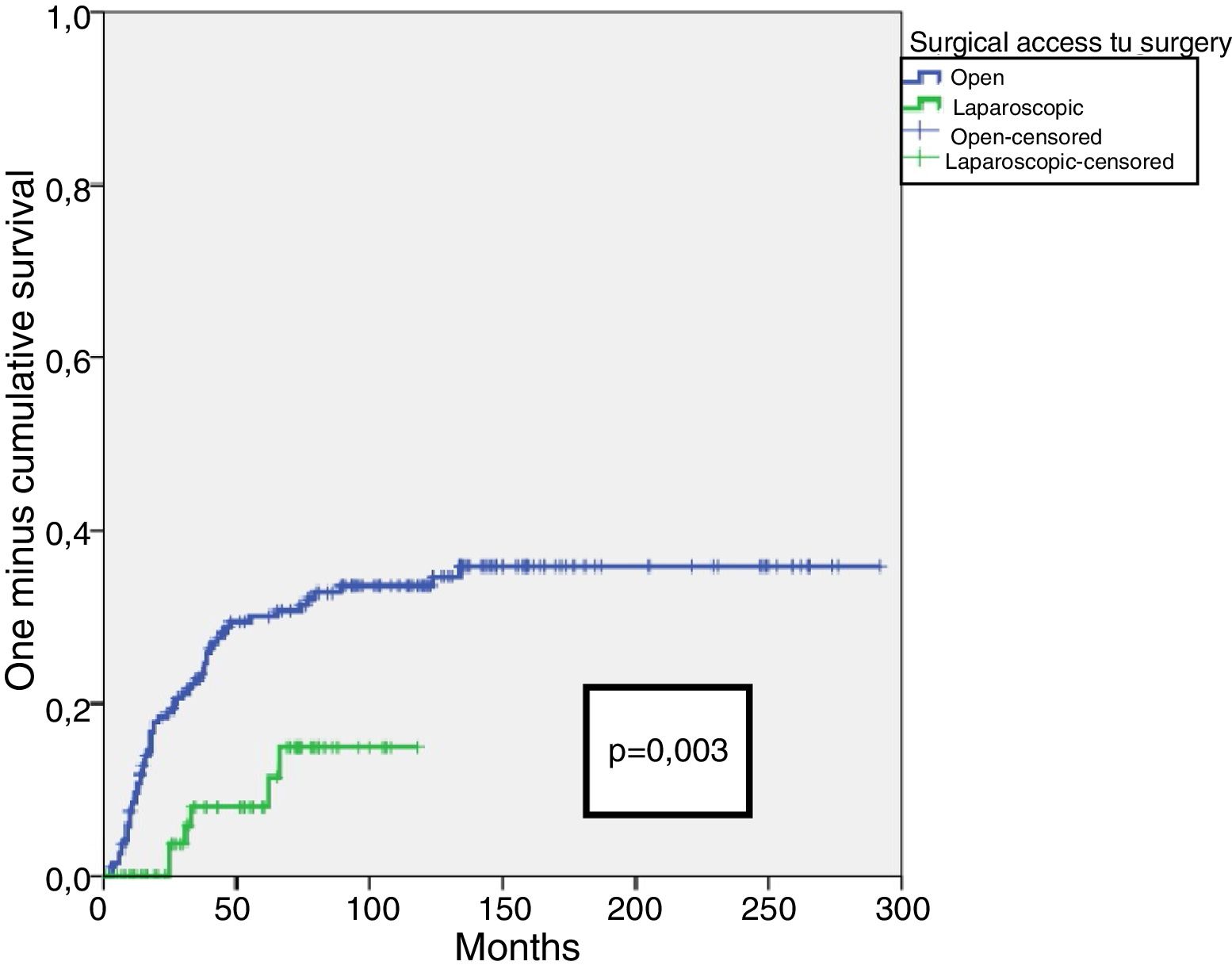
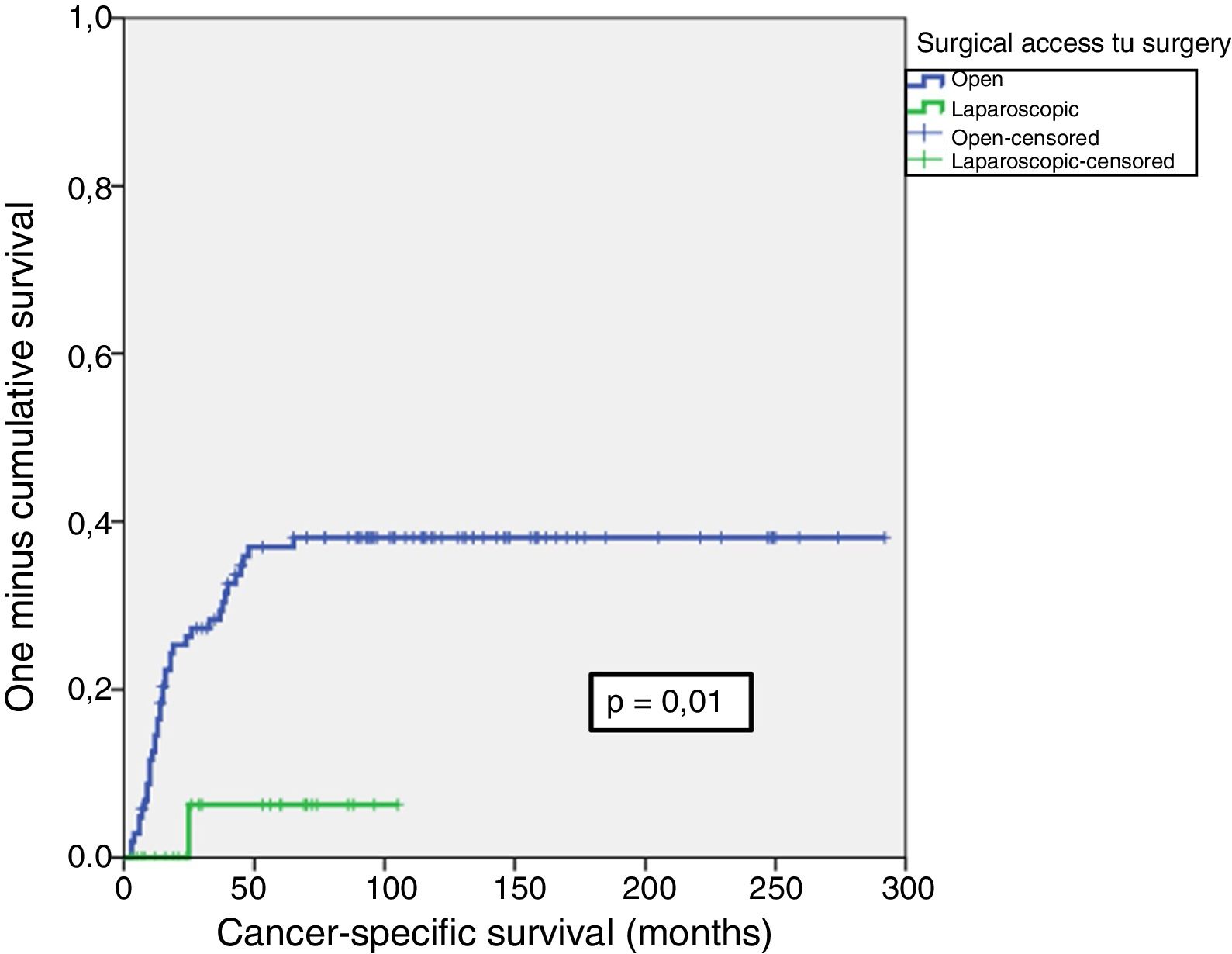
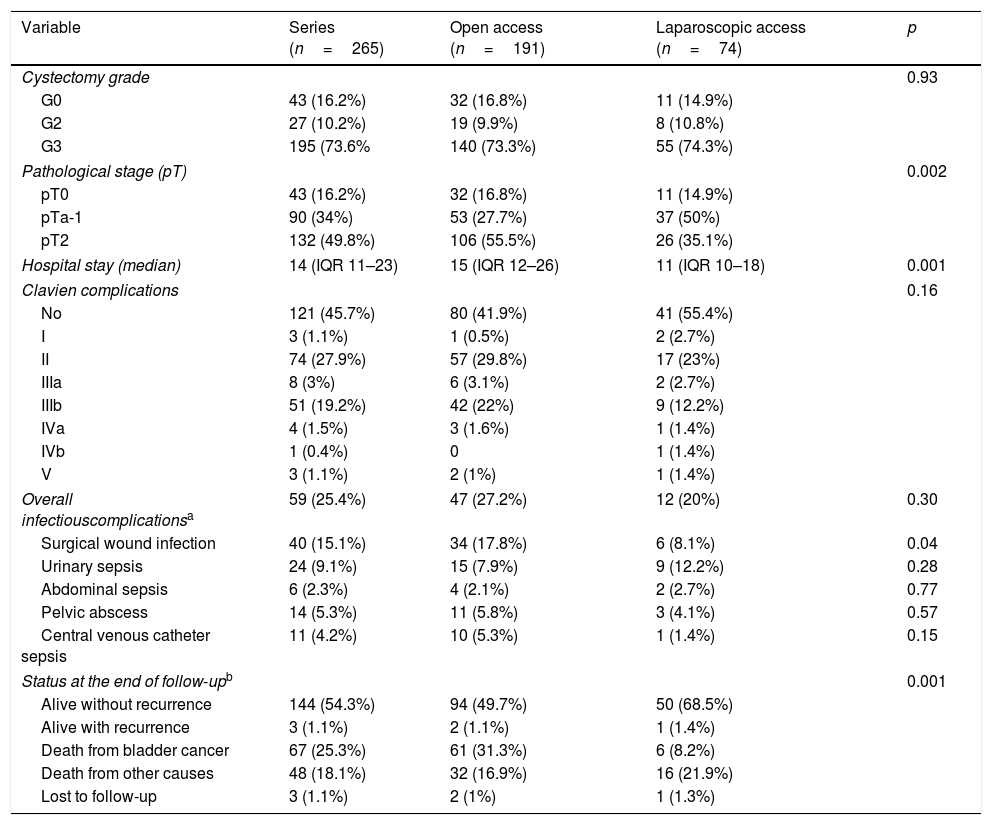
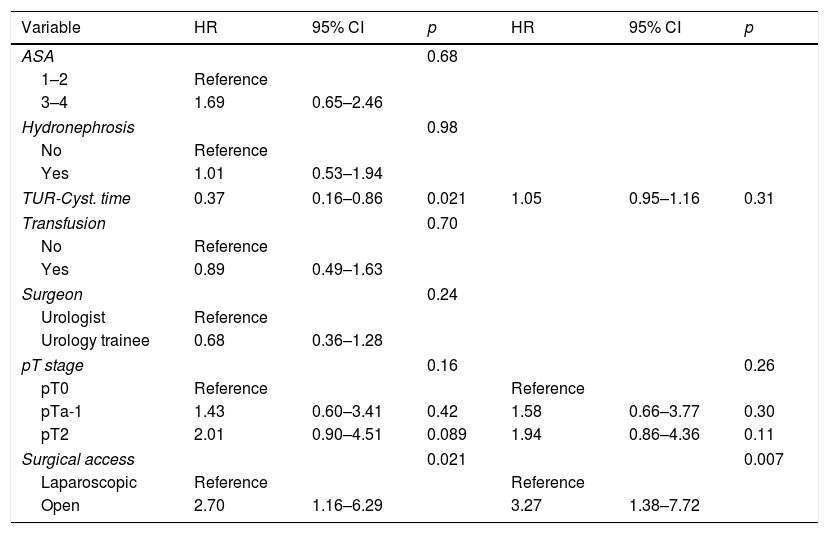
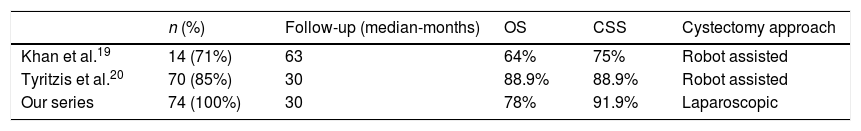
Results90.9% were males with a median age of 65years and a median follow-up period of 65.5 (IQR27.75–122) months. Patients with laparoscopic access presented a significantly higher ASA index (p=0.0001), a longer time between TUR and cystectomy (p=0.04), a lower rate of intraoperative transfusion (p=0.0001), a lower pT stage (p=0.002) and a lower incidence of infection associated with surgical wounds (p=0.04). When analyzing the different risk factors associated with cancer-specific mortality, we only found the ORC approach (versus LRC) as an independent predictor of cancer-specific mortality (p=0.007). Open approach to cystectomy multiplied the risk of mortality by 3.27.
ConclusionsIn our series, the laparoscopic approach does not represent a risk factor compared to the open approach in pT0-2N0R0 patients.
La cirugía mínimamente invasiva representa un abordaje quirúrgico atractivo en la cistectomía radical. Sin embargo, a la espera de estudios definitivos todavía es controvertido el efecto que pudiera tener en los resultados oncológicos. El objetivo de este estudio es evaluar el efecto del abordaje laparoscópico sobre la mortalidad cáncer-específica.
Material y métodoEstudio de cohortes retrospectivo de dos grupos de pacientes en estadio pT0-2pN0R0 sometidos a cistectomía radical abierta (CRA) (n=191) y laparoscópica (CRL) (n=74). Se realizó un análisis mediante regresión de Cox para identificar primero las variables predictoras y posteriormente las variables predictoras independientes relacionadas con la supervivencia.
ResultadosEl 90,9% fueron varones; la mediana de edad fue de 65años y la mediana de seguimiento, de 65,5 (IQR 27,75-122) meses. Los pacientes con acceso laparoscópico presentaron de forma significativa un mayor índice ASA (p=0,0001), un mayor tiempo entre la resección transuretral (RTU) y la cistectomía (p=0,04), una menor tasa de transfusión intraoperatoria (p=0,0001), un menor estadio pT (p=0,002) y una menor incidencia de infección asociada a herida quirúrgica (p=0,04). Al analizar los distintos factores de riesgo asociados a mortalidad cáncer-específica, solo encontramos el abordaje mediante CRA frente a CRL como factor predictor independiente de mortalidad cáncer-específica (p=0,007). El acceso abierto a la cistectomía multiplicó el riesgo de mortalidad por 3,27.
ConclusionesEn nuestra serie, cuando limitamos los distintos factores identificados asociados a mortalidad cáncer-específica analizando pacientes pT0-2N0R0, el abordaje laparoscópico no representa un factor de riesgo frente al abordaje abierto.