To determine the frequency of lymph node involvement in patients with clinically localized prostate adenocarcinoma who had radical prostatectomy and extended pelvic lymphadenectomy.
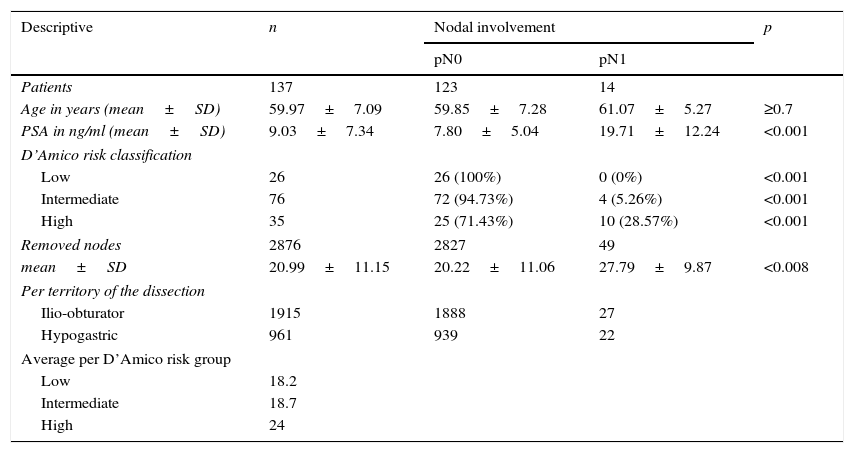
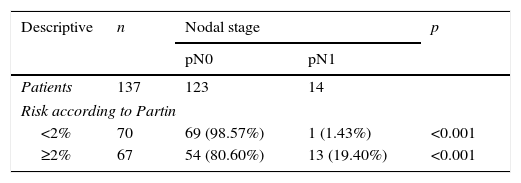
Material and methodsA prospective observational study was conducted on 137 patients with clinically localized prostate cancer of low, intermediate or high risk according to the D’Amico classification. All participants underwent radical prostatectomy plus extended pelvic lymphadenectomy in 3 reference centers in Bogota, Colombia, between 2013 and 2014. The following variables were assessed: age, prostate specific antigen levels, Gleason score of the biopsy, probability of lymph node involvement calculated with Partin tables and the histopathology result of the surgical specimen, with the definitive Gleason pattern and the total number of resected and involved lymph nodes per tumor, according to the territory of the dissection.
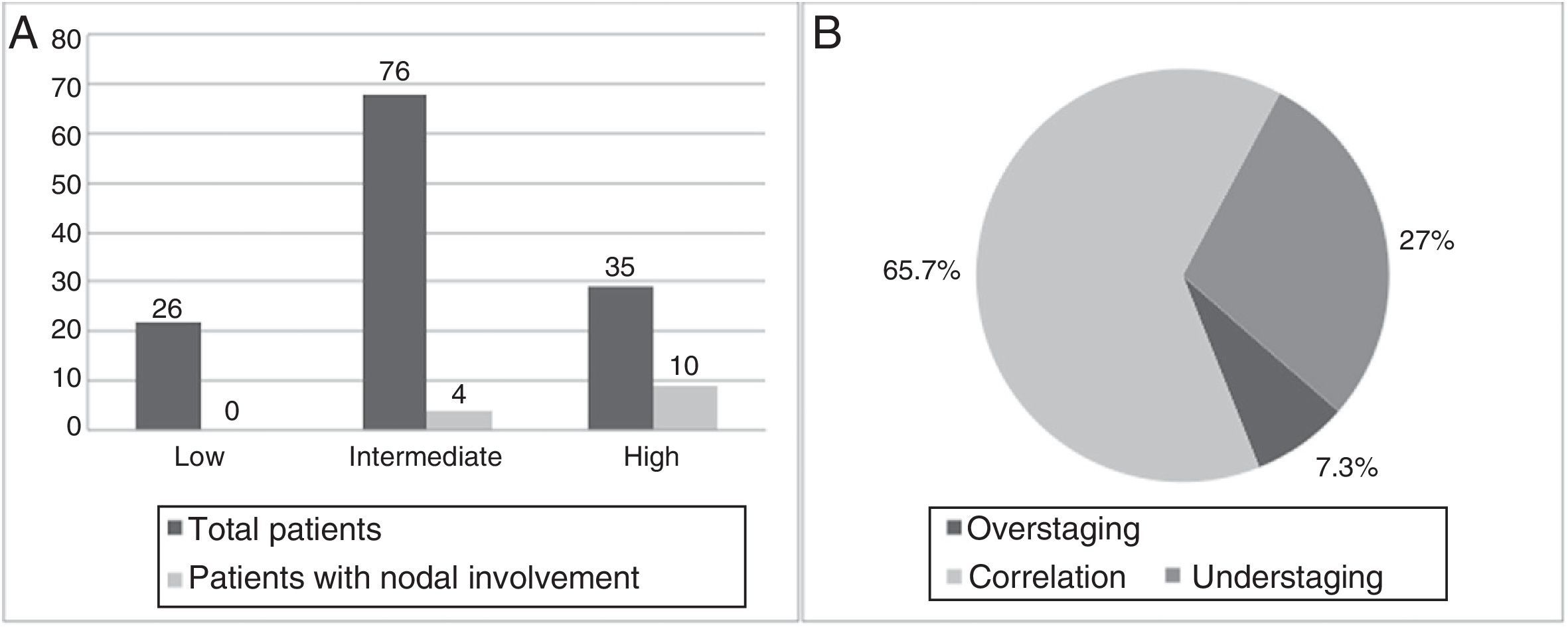
ResultsA total of 2876 lymph nodes were extracted (an average of 20.99 lymph nodes per patient). There was lymph node involvement in 14 (10.22%) patients. The high-risk and intermediate-risk group presented lymph node metastases in 28.57% and 5.25%, respectively. There was no lymph node involvement in the low-risk group. Of the patients at risk of lymph node involvement (≥2% according to the Partin tables), 19.40% had lymph node metastases.
ConclusionLymph node involvement in our population is similar to that reported in the worldwide literature. Extended pelvic lymphadenectomy increased the probability of detecting lymph node metastases in our community.
Determinar la frecuencia de compromiso ganglionar en pacientes con adenocarcinoma de próstata clínicamente localizado llevados a prostatectomía radical y linfadenectomía pélvica extendida.
Material y métodosSe realizó un estudio observacional prospectivo con 137 pacientes con cáncer de próstata clínicamente localizado, de riesgo bajo, intermedio y alto según la clasificación de D’Amico. Todos los sujetos fueron llevados a prostatectomía radical más linfadenectomía pélvica extendida en 3 centros de referencia en Bogotá, Colombia, entre los años 2013 a 2014. Se evaluaron las siguientes variables: edad, PSA, Gleason de la biopsia, probabilidad de compromiso ganglionar por tablas de Partin, y el resultado histopatológico del espécimen quirúrgico con el patrón de Gleason definitivo y el total de ganglios resecados y comprometidos por el tumor, de acuerdo al territorio de la disección.
ResultadosSe extrajeron un total de 2.876 ganglios, en promedio 20,99 ganglios por paciente. Se encontró compromiso ganglionar en 14 (10,22%) pacientes. El grupo de riesgo alto e intermedio presentaron metástasis ganglionares en el 28,57% y el 5,25% respectivamente. No hubo compromiso ganglionar en el grupo de bajo riesgo. De los pacientes con un riesgo de compromiso ganglionar ≥2%, según las tablas de Partin, el 19,40% presentó metástasis ganglionares.
ConclusiónEl compromiso ganglionar en nuestra población es similar al reportado en la literatura mundial. La linfadenectomía pélvica extendida aumentó la probabilidad de detección de metástasis ganglionares en nuestro medio.