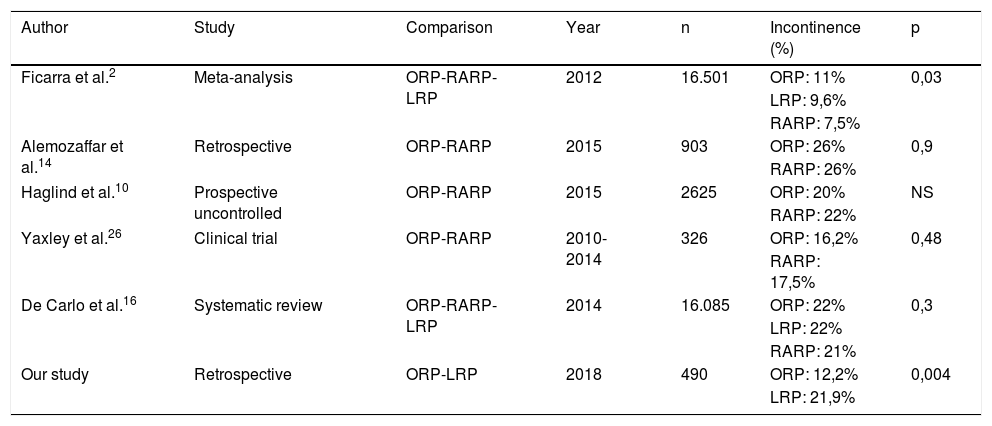
There are very few articles comparing open radical prostatectomy (ORP) vs. laparoscopic radical prostatectomy (LRP) and their functional results or urinary continence (UC), which is one of the most important objectives to pursue after oncological results.
Objectivesto compare postoperative UC in patients with localized prostatic adenocarcinoma treated with OPR or LRP.
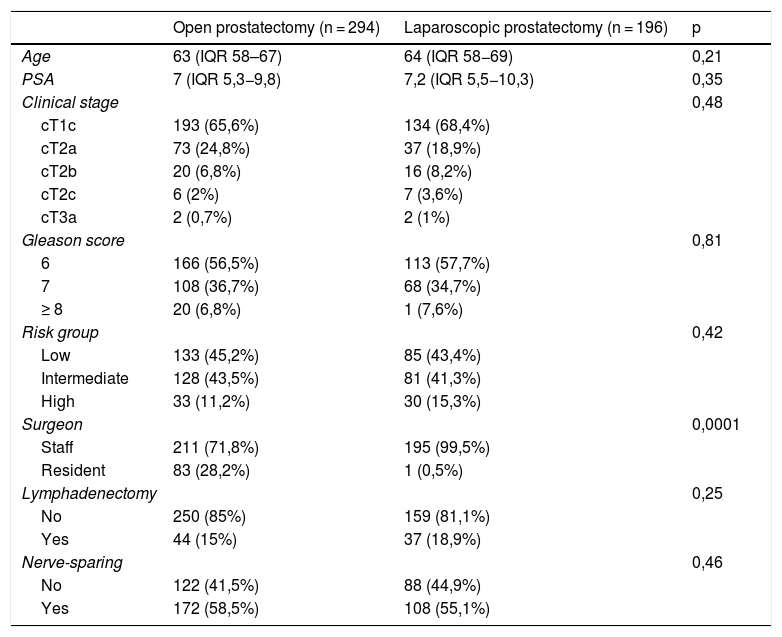
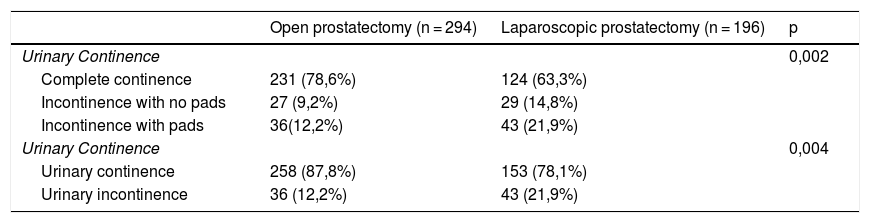
Materials and MethodsComparison between two patient cohorts (312 for ORP and 206 for LRP) between 2007−2015. The UC was evaluated at 3, 6, 12, 18 and 24 months. Continence was defined and classified as follows: a) UC, no need of pads, and b) urinary incontinence (UI), use of pads.
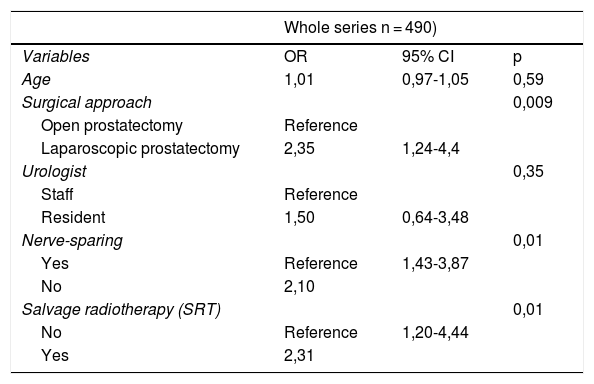
To compare the qualitative variables, we employed the chi-squared test and ANOVA for quantitative variables. We performed a multivariate analysis using logistic regression with dependent qualitative variable UI. Statistical significance when p < 0,05.
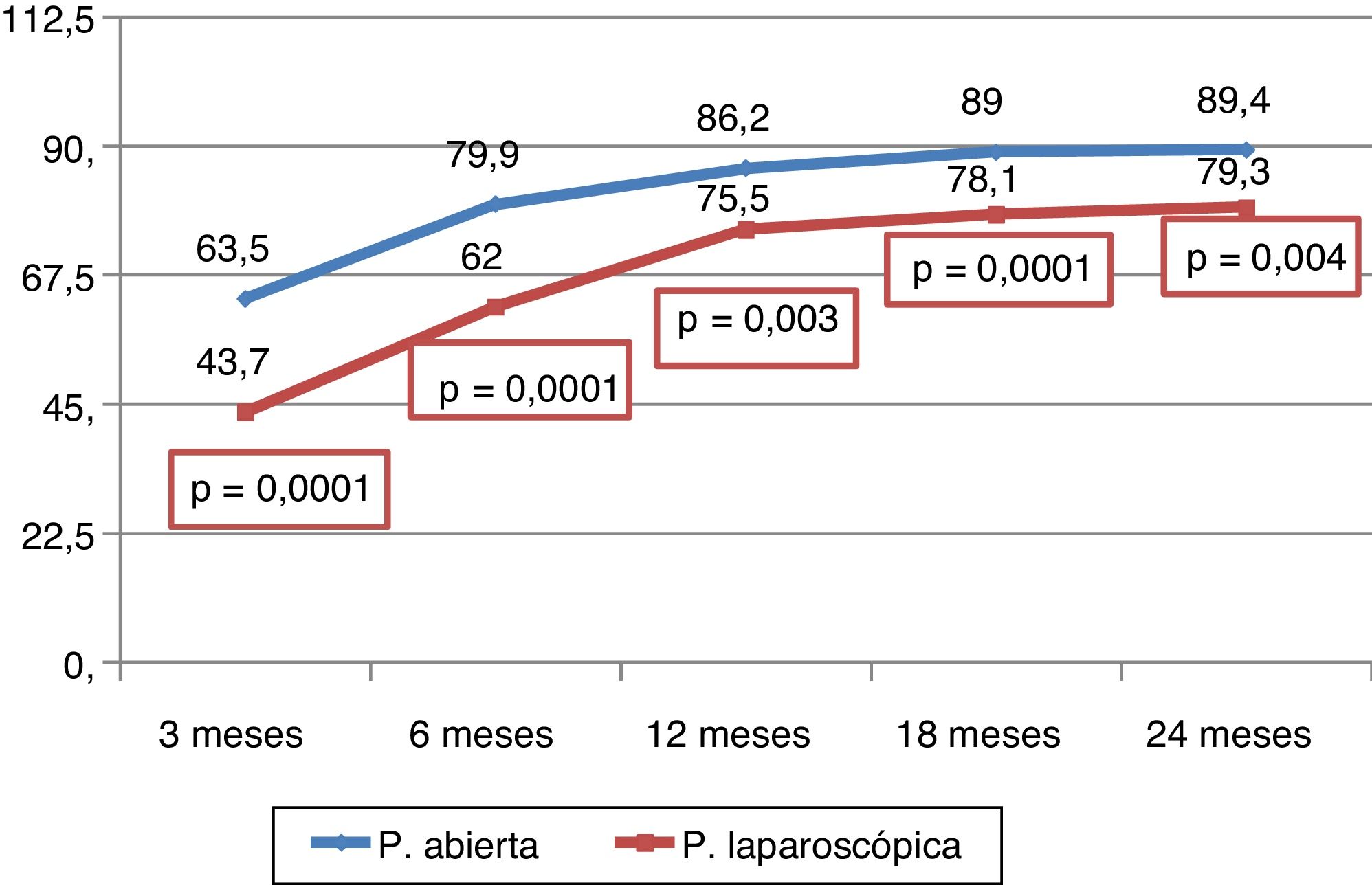
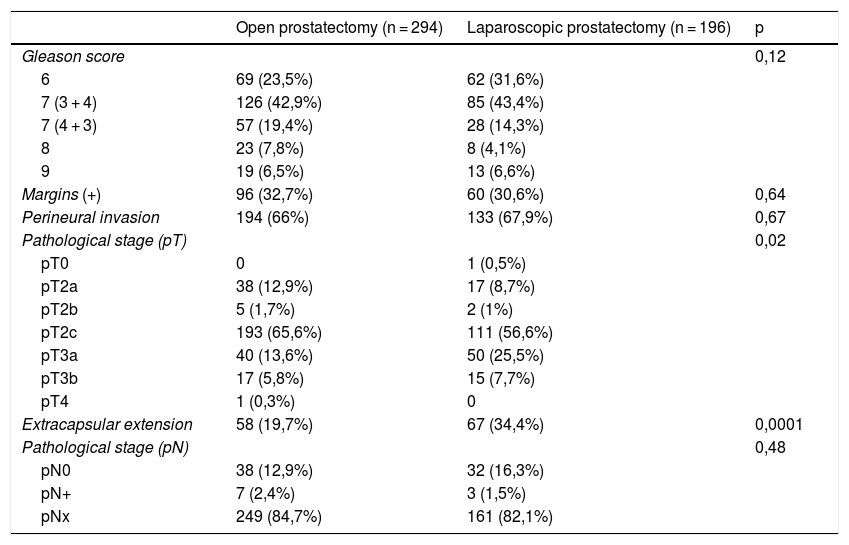
ResultsNerve-sparing was performed in 51,7% cases. At 24 months after surgery, 72,4% patients had UC, of which 87,7% were from the ORP group and 78,1% in the LRP group (p = 0,004). 22,7% of patients experienced biochemical recurrence (BR), with 83% treated with salvage radiotherapy (SRT), presenting greater UI percentage (p = 0,036). ORP patients showed a higher percentage of anastomosis stricture (p = 0,03).
ConclusionsLRP, non-nerve sparing, and SRT were directly related to postoperative IU.
Pocos son los estudios que comparan la prostatectomía radical abierta (PRA) con la prostatectomía radical laparoscópica (PRL) y sus resultados funcionales como la continencia urinaria (CU), siendo éste uno de los objetivos prioritarios tras el control oncológico.
Objetivoscomparar la CU postoperatoria en los pacientes con adenocarcinoma de próstata localizado, intervenidos mediante PRA frente a PRL.
Material y métodosComparación de dos cohortes (312 con PRA y 206 con PRL) entre los años 2007 y 2015. El estado de CU se recogió a los 3, 6, 12, 18 y 24 meses. Para el manejo estadístico hemos agrupado la continencia en: a) CU, pacientes que no precisaron absorbentes y, b) Incontinencia urinaria (IU), pacientes que precisaron absorbentes.
Para el contraste de variables cualitativas se ha utilizado el test de la Chi cuadrado para las variables cualitativas y ANOVA para las cuantitativas. Análisis multivariable mediante regresión logística para la variable dependiente IU. La significación estadística se consideró cuando existió una p < 0,05.
ResultadosEn el 51,7% se realizó conservación neurovascular. A los 24 meses de la cirugía, el 72,4% presentaban CU, de los cuales PRA 87,8% frente al 78,1% de PRL (p = 0,004). El 22,7% presentaron recidiva bioquímica (RB), siendo el 83% tratados con radioterapia de rescate (RTR). En los pacientes con RTR presentaron mayor porcentaje de IU frente a los que no la recibieron (p = 0,036). Se objetivó mayor porcentaje de estenosis de la anastomosis en PRA (p = 0,03).
ConclusionesLa PRL, la no CNV y la RTR se relacionaron directamente con la CU postoperatoria.