Clinical findings in many nail disorders are not usually pathognomonic. An accurate diagnosis therefore relies on inspection of the nail unit from different angles. We review clinical features of different nail disorders that can be observed during frontal examination of the distal edge of the nail plate and the hyponychium and correlate these with features observed when the nail is viewed from above. Frontal examination of the distal nail unit can help establish a clinical diagnosis in routine practice.
Los signos clínicos que acompañan a muchas alteraciones ungueales habitualmente no son patognomónicos de ninguna enfermedad concreta. Por tanto, la exploración del aparato ungueal desde diferentes ángulos de visión es fundamental para realizar un diagnóstico acertado. En el presente artículo se revisan los signos clínicos que pueden obtenerse mediante la exploración frontal del borde distal de la lámina ungueal y el hiponiquio, y se correlacionan con los signos de la exploración aérea. Dicho abordaje permite facilitar el diagnóstico clínico de la enfermedad ungueal en la práctica diaria.
In general, both the clinical examination and assessment of nail diseases are often performed from an aerial and quick perspective; however, this approach does not allow us to see all the details involved with nail disease. It is desirable to examine the nail from all angles (lateral, aerial, and frontal) to obtain as much information as possible to contribute to diagnosis, treatment, and assessment of the progression of nail disease.
The distal and lower region of the nail is the hyponychium. In its upper region, this space is outlined by the nail free ventral margin, depth-wise by the onychodermal band fibrous structure (the nail back door), in its lower region by an epithelium devoid of fingerprints and appendages covering a dense dermis, and in its most distant region by the distal nail fold.1–4
The hyponychium responds in variable way to certain stimuli, such as scaling, hyperkeratosis, hypertrophy, hyperplasia, and pigmentation of the epithelium, which can be accompanied by changes in the thickness and morphology of the nail plate. These clinical signs are not specific to a single disease and may appear in isolation or together. These nail changes are due, among others, to inflammatory, infectious, or tumoral processes, and they can be local or systemic.5,6 Overall, the toenails are more commonly affected than the fingernails.
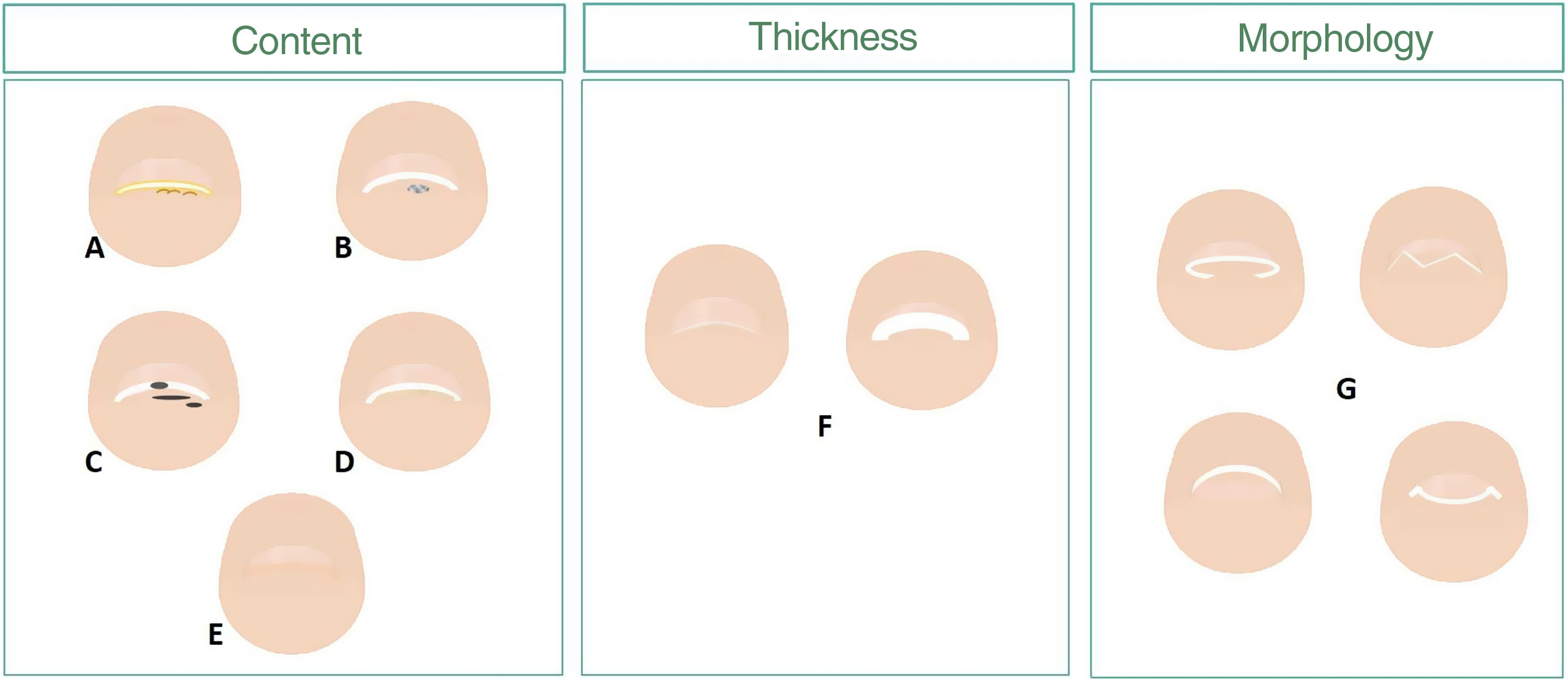
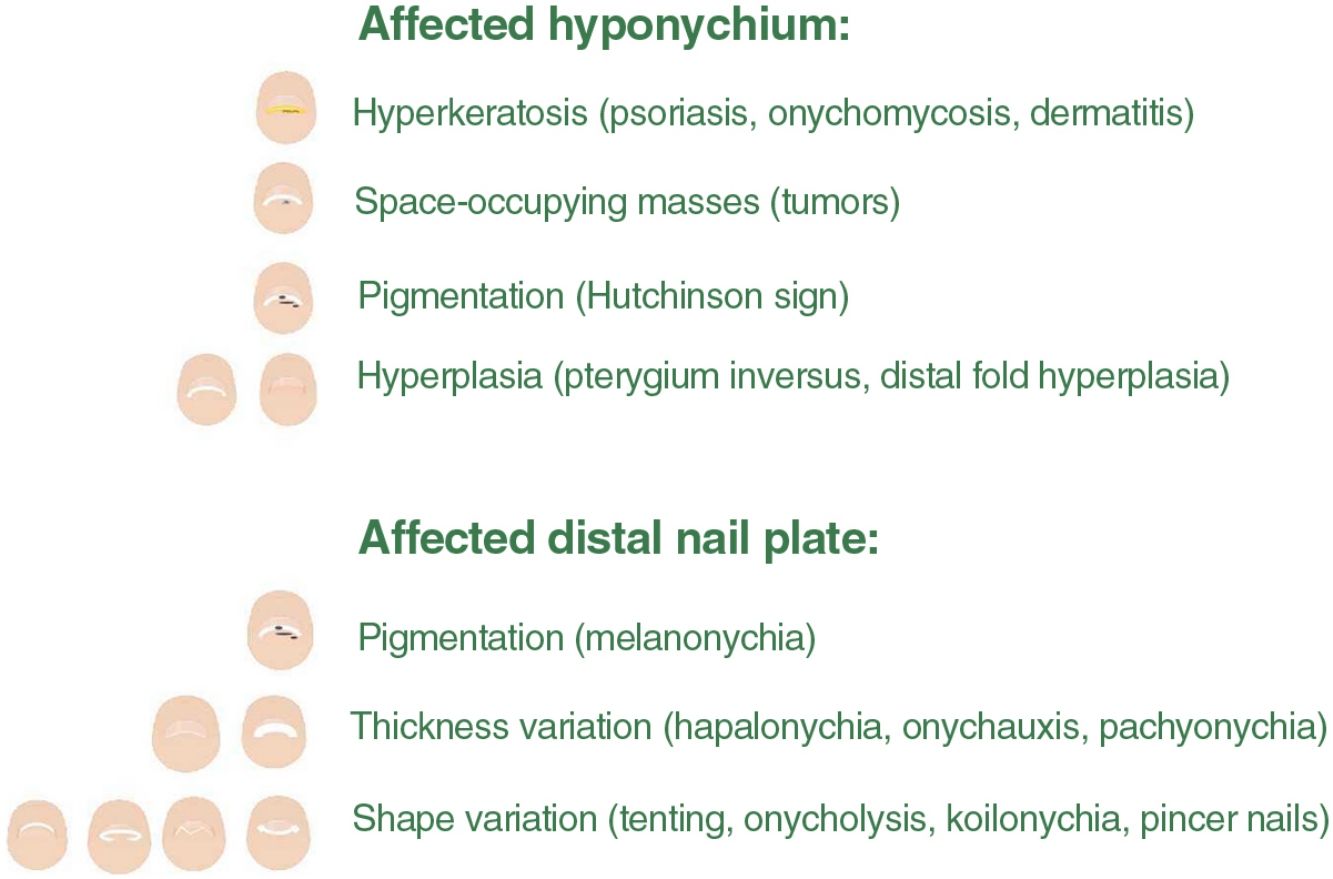
This article provides a description of nail abnormalities from the nail plate distal frontal view following a pattern scheme based on the area damaged, whether it is the nail epithelium, or the nail plate distal region (fig. 1). The information obtained, along with a detailed clinical history and examination of the nail apparatus, should help us achieve the proper clinical diagnosis.
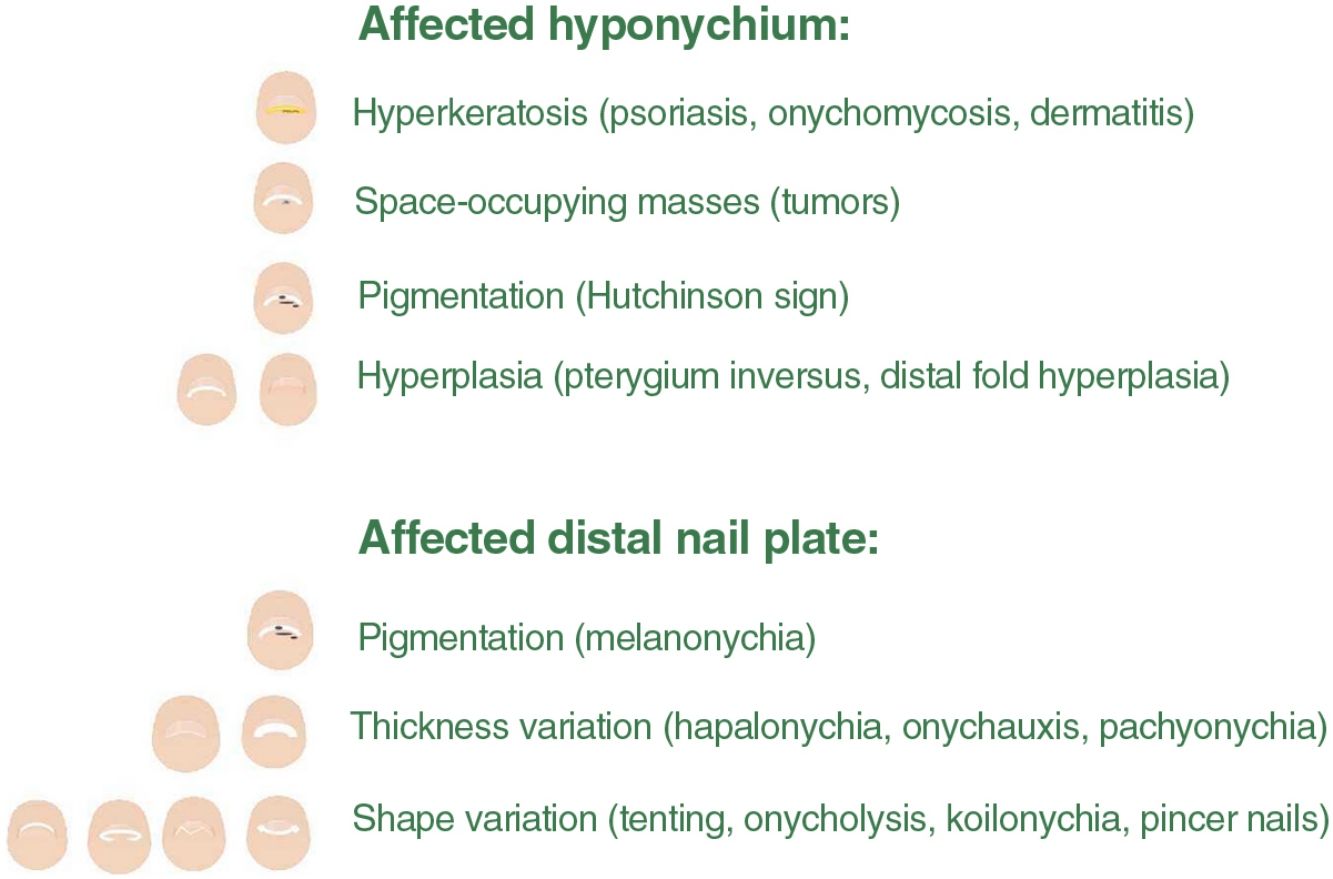
Scheme of changes to the nail distal frontal view, hyponychium, and nail plate. The hyponychium response to a change can be with hyperkeratosis (A), space-occupying masses (B), pigmentation (C), and/or hyperplasia (D). Variations in thickness (F) and morphology of the nail distal edge (G) are some of the changes to the nail plate we can find (D and E).
Subungual hyperkeratosis is defined as the thickening of the stratum corneum of both the epithelium of the hyponychium and the nail bed, with an accumulation of keratinocytes and debris underneath the nail plate distal region.7,8 Numerous causes can lead to subungual hyperkeratosis, including inflammatory, infectious, tumoral, or various process inducing changes to the nail bed—such as trauma, drugs, or systemic diseases—and that produce onycholysis. Subungual hyperkeratosis is more common in the toenails, likely due to repetitive trauma.9
Hyperkeratosis can be diffuse or localized. It is diffuse in diseases with extensive involvement of the nail bed, such as dermatitis, onychomycosis, and psoriasis. When hyperkeratosis is localized, a tumoral process should be suspected.10
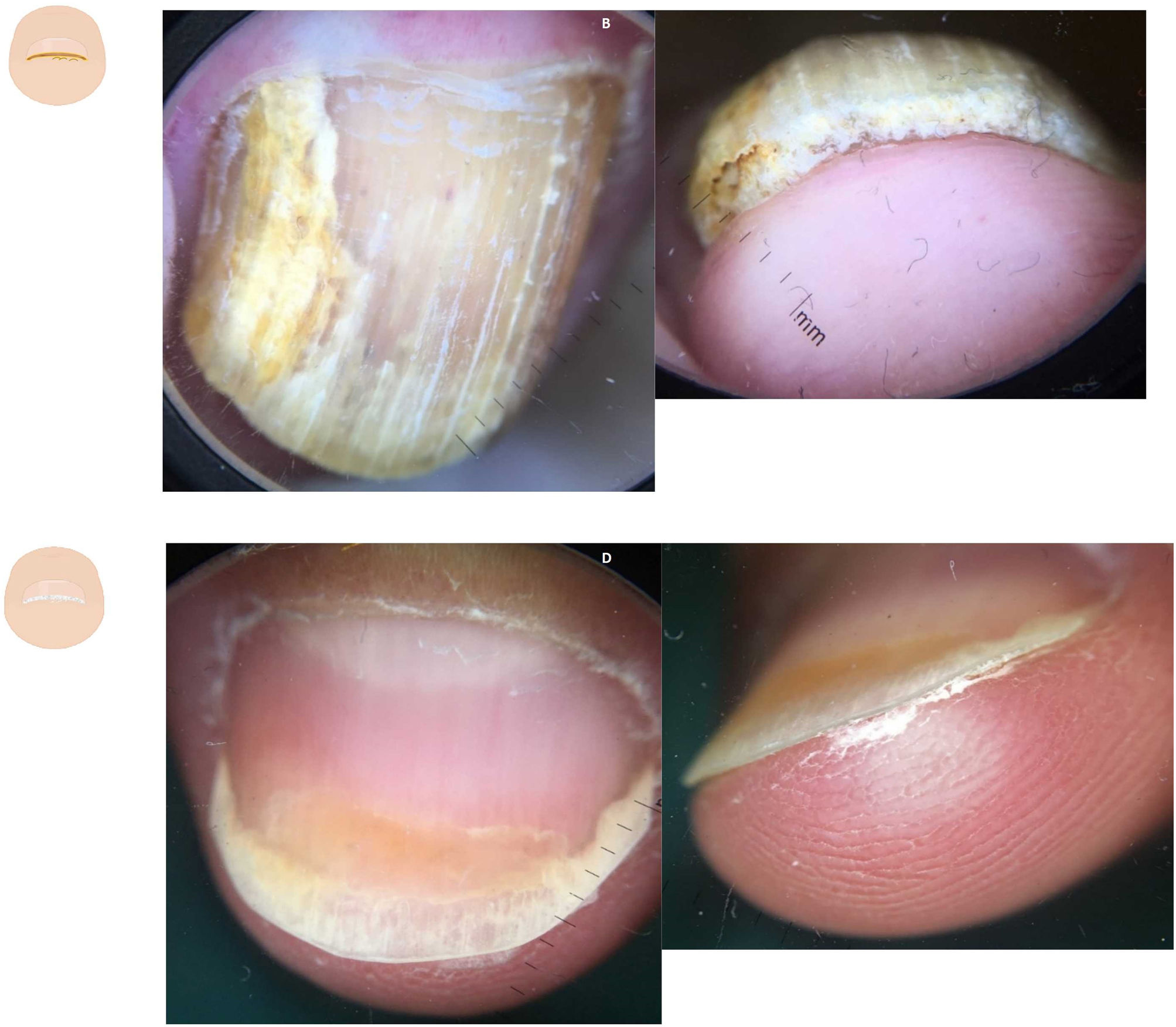
Diffuse subungual hyperkeratosisOnychomycosis often presents with onycholysis and thick—predominantly yellowish—scaling next to the nail plate ventral region11,12 (Fig. 2A and fig. B). The presence of ruin-like appearance and/or distal irregular termination at the nail distal end, due to fragility caused by fungal invasion, supports this diagnosis.13 The aerial view reveals the presence of onycholysis with sharp irregular borders, and various matte colors of the nail (the so-called Aurea borealis), etc.
Content changes. A: Dermatoscopy of onychomycosis in the aerial view; onycholysis with an irregular border, dermatophytoma, and the aurora borealis sign can be seen. B: Dermatoscopy of onychomycosis in the distal frontal view with presence of onycholysis, diffuse subungual hyperkeratosis, and the ruination sign. C: Dermatoscopy in nail psoriasis showing oil drop sign and onycholysis. D: Dermatoscopy in psoriasis with presence of onycholysis with diffuse, fine, silver-white subungual hyperkeratosis.
Onycholysis with fine, silvery-white scaling—slightly more significant in the sides—is indicative of psoriasis (Fig. 2B and fig. C). Dermatoscopy may reveal elongated and dilated capillaries with irregular distribution in the hyponychium and fingertip.14,15 The clinical signs typical of psoriasis in the aerial view, such as pitting, the oil-drop sign, and vascular involvement of the nail bed, among others, can also be present. Associated onychomycosis may exist, and typical signs of fungal infection should be looked for during the physical examination.16
Diffuse hyperkeratosis is typical of periungual dermatitis, pityriasis rubra pilaris, and repetitive trauma, among other conditions.7,17
Localized subungual hyperkeratosisOnicoclavus, also known as subungual heloma or horn, presents as a painful hyperkeratosis with a translucent center, sometimes associated with hemorrhagic areas. Onicoclavus is often found in the nail bed middle distal region18 (fig. 3A, and fig. B). When lifting the nail, the keratotic formation with an area of bleeding can be seen. Onicoclavus is a reactive process to persistent pressure or trauma to the nail bed, often occurring as a consequence of anatomical or biomechanical changes to the foot.
Content changes. A: Onychoclavus: onycholysis with pigmented spot in the nail middle distal region. B: Onychoclavus: hyperkeratosis with a hemorrhagic area in the hyponychium middle section. C: Onychopapilloma: discreet longitudinal erythronychia with splinter hemorrhage and mild distal “V” onycholysis. D: Onychopapilloma: onycholysis with focal subungual hyperkeratosis attached to the nail plate ventral region. F: Fibrokeratoma: lateral onycholysis with a hemorrhagic pigmented area. G: Fibrokeratoma: onycholysis with presence of well-demarcated subungual hyperkeratosis.
Onychopapilloma is a specific nail tumor. Hyperkeratosis is often localized, attached to the nail plate ventral region, and painless.10,19 (Fig. 3C and fig. D). The most common clinical sign is a longitudinal erythronychia band with distal onycholysis. However, it can also show as leukonychia, longitudinal melanonychia, or splinter hemorrhages.20
Warts typically appear as a papule or plaque with hyperkeratosis and black dots on the surface. Dermatoscopy reveals papillomatous areas with intracorneal hemorrhages in the papilla central region, resembling “frog eggs,” or black dots with an irregular distribution on the surface.21
Other causes of localized hyperkeratosis include conditions such as Bowen's disease, or squamous cell carcinoma.10
Space-occupying lesions in the hyponychiumTumorsSpace-occupying lesions in the hyponychium are often accompanied by onycholysis. Various tumors should be considered in these cases, and here the patient's clinical history can provide significant diagnostic information.22
Subungual fibrokeratoma is more commonly found in the periungual location. However, it can also be found in the subungual area23 (Fig. 3E and fig. F). It shows as a sausage-shaped mass or tumor of fibrous consistency, distal hyperkeratosis, and gradual growth.24 The aerial view can show onycholysis.
Subungual exostosis appears as a hard, slowly growing, progressive tumor, often accompanied by pain.22 The physical examination reveals the presence of distal hyperkeratosis and onycholysis. The diagnosis is confirmed through a simple x-ray, but it may not be evident in the early stages of the disease.25
Subungual keratoacanthoma is a rare type of tumor. It should be suspected in the presence of a painful, rapidly growing keratotic nodule with a centrally depressed area filled with cornified material in the nail distal region.22 Phalangeal involvement is a common finding, and x-rays often show the presence of a cup-shaped erosion.26
In the presence of chronic nail abnormalities unresponsive to standard treatments, the possibility of Bowen's disease or squamous cell carcinoma should be considered. The clinical signs of these conditions are varied mimicking warts, onychomycosis, ingrown toenails, or any of the tumors mentioned earlier.27,28
Digital or subungual metastases can also resemble an inflammatory, infectious, or traumatic process affecting a finger. Both the patient's clinical history and physical examination of the lesion—which is often accompanied by excessive pain relative to the clinical presentation—help achieve the proper diagnosis.29,30
Pterygium inversum unguisPterygium inversum unguis is a rare entity that can only be diagnosed by looking at the nail from the front.8 Examination reveals a reduced hyponychium due to the presence of a fibrous membrane that connects the hyponychium floor to the nail plate ventral region. There is a congenital form and an acquired form of the disease, the latter being further categorized into reversible and irreversible. The former is associated with connective tissue diseases (systemic sclerosis, systemic lupus erythematosus), neurofibromatosis, hemiparesis, and nail cosmetic treatments, among others.31
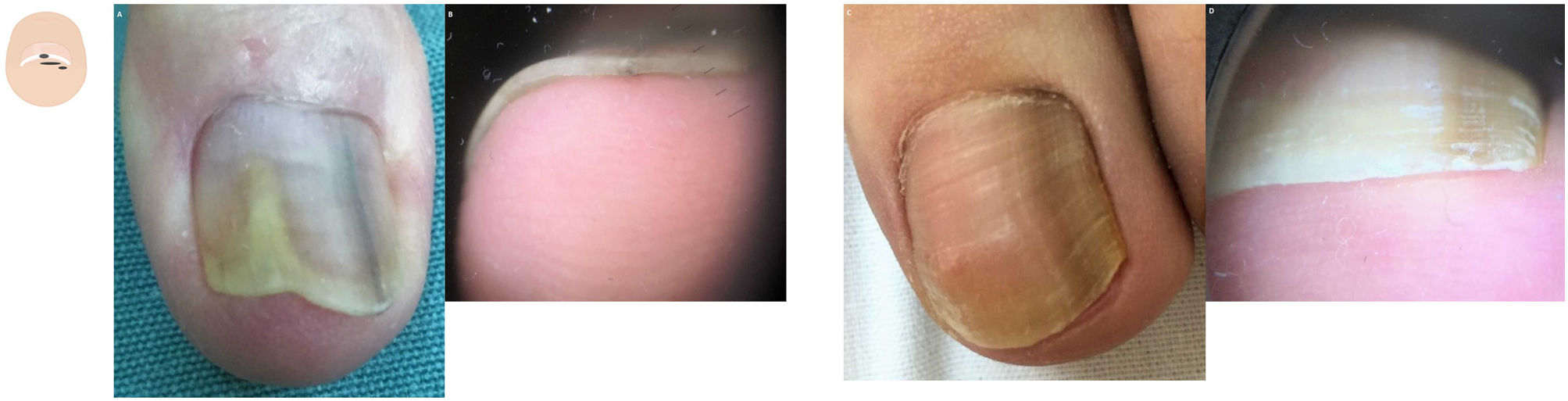
Hypertrophy of the distal nail foldHypertrophy of the distal nail fold is physiological in the early years of life and pathological at older ages. The first toe is the most commonly affected of all, and the extent of hypertrophy can only be assessed in the frontal view. The physiological form seems to be due to a lack of nail pressure on the subungual tissue (Fig. 4A and fig. B). The pathological form is common in situations where the nail is overwhelmed by the forces exerted by the lateral and distal folds (Fig. 4C and fig. D).32 The most typical clinical sign is an increased distal nail fold and fingertip stopping nail growth. Hypertrophy of the distal fold is closely associated with onycholysis, especially in its stage 5 (nail bed loss), in which the nail bed undergoes progressive size reduction.33
Pigmentation. Hutchinson's SignHutchinson's sign is pigmentation of the periungual skin. Hutchinson's sign can be a benign or malignant clinical sign and be associated with local or systemic disease. When it appears accompanying melanonychia in adult patients, it is probably suggestive of melanoma. Conversely, it is a common finding in melanonychia in children and is often indicative of a congenital melanocytic nevus.34
Frontal view assessment of melanonychias help us identify which part of the matrix is responsible for pigmentation. If pigmentation is located in the nail plate upper region, it is related to the proximal matrix; if located in the middle-lower region, by distal matrix35 (fig. 5, fig. 5A-C). When numerous pigmentation spots are found in the thickness of the nail plate in melanonychia, it may be indicative of melanoma.
Thickness changes to the nail plate free edgeThickness variations of the nail plate are often associated with other changes affecting the matrix and nail bed. The causes are diverse, including local or systemic issues, traumatic processes, and stop of nail growth, among others. These changes can affect the entire nail or part of it, and involve a single or multiple nails. The nail free edge can only be studied through frontal inspection of the nail plate. A reduced thickness of the nail plate is more common in the fingernails, while an increased thickness is more common in the toenails.
Reduced nail plate thicknessThe term hapalonychia refers to a decreased nail thickness (< 0.5mm).5 It is often seen in fingernails with physiological aging, but it is also a typical finding of the brittle nail syndrome, specific local nail diseases (such as occupational dermatitis, trachyonychia, psoriasis, or lichen planus), and systemic diseases (such as chronic arthritis, leprosy, myxedema, peripheral neuritis, hemiplegia, and cachexia, among others).6 (fig. 6A-C). Thinning of the nail plate can be total or focal and affect one or multiple nails. If thinning is seen in a single finger and is localized, the most likely cause is a tumor, such as onychopapilloma. In Darier's disease, this partial thinning of the nail plate can be seen in multiple nails.17
Increased nail plate thicknessNail growth stop can be due to local or inflammatory causes, repetitive microtrauma, and systemic processes (such as yellow nail syndrome, for example). In these situations, the nail thickens while changes of color—turning yellow—and morphology.6,36 These changes also occur physiologically with the aging of the toenails and pathologically in retronychia, among others.37 (fig. 7A, fig. B).
Morphological changes. A: Aerial view of the feet of an elderly patient with xanthonychia of the first 2 nails. B: Onychauxis, uniform thickening of the nail plate entire distal edge. C: Aerial view of the feet of a patient with a decreased transverse diameter of the nails middle distal region. D: Pachyonychia: nail of cylindrical morphology due to thickening of the nail plate middle distal region and union of both ends of the nail. E: Aerial view of onychomatricoma: discreet splinter hemorrhages and distal “V” onycholysis in the nail plate distal region. F: Localized honeycomb-shaped nail plate thickening.
Congenital pachyonychia is a genodermatosis characterized by very distinctive nail changes, along with other symptoms. The nails gradually thicken in the middle distal region at the expense of the nail plate and bed. This results in an increased transverse curvature that gives the nail a cylindrical morphology and a dark brown color. These changes can cause pain and difficulty during finger manipulation.38 In advanced stage of the pincer nails, we can observe this morphology (Fig. 7C and fig. D)
Sometimes, the nail plate increased thickness is due to a localized change to the matrix. This is called onychauxis (the nail longitudinal thickening). An example of this is onychomatricoma, a benign fibroepithelial tumor (Fig. 7E and fig. F). It shows as the nail longitudinal and transverse thickening, xanthonychia, splinter hemorrhages, and the typical honeycomb shape or distal woodworm appearance.39 The histopathological analysis of distal nail clippings could confirm the diagnosis.40
Changes to the morphology of the nail plate free distal edgeThe morphology of the nail is determined, among other things, by its longitudinal and transverse axes, the latter being slightly convex. The angle of these axes varies between fingers and the toes. Transverse axis variations can lead to different nail shapes and be indicative of certain diseases. These variations are only evident during frontal inspections of the nail.
Clinical signs of nail lichen planus vary depending on whether the matrix and/or nail bed are damaged. Focal damage to the nail bed causes onycholysis, with or without hyperkeratosis that gives it a characteristic “tent-shaped” nail morphology17 (Fig. 8A and fig. B).
Thickness changes. A: Aerial view of lichen planus: onycholysis with nail plate loss. B: Lichen planus: tent sign. C: Aerial view of idiopathic onycholysis with a smooth proximal border on the fingers. D: The degree of onycholysis can be better seen in the frontal view. E: Aerial view of nail lichen planus, with a central fissure and hapalonychia. F: Lateral view shows koilonychia, with a concave transverse axis. G: Aerial view of the first toe nail with narrowing of the transverse axis in the nail middle distal region. H: Type 1 or common pincer nail, with an increased angle of the nail distal transverse axis.
Onycholysis is one of the most common clinical signs of nail disease and is associated with the detachment of the nail plate from the nail bed (Fig. 8C and fig. D). The causes of onycholysis are varied. Although it may be challenging to see from the aerial view, the frontal view will reveal a greater or lesser degree of separation of the nail from the bed depending on the associated disease and its evolution.41,42
In koilonychia or spoon-shaped nails, both the transverse and longitudinal axes of the nail become concave, with the central region being depressed and the lateral edges elevated.43 It is physiological in 5% of the children within the first 2 years of life and is common in old age. Koilonychia can be the clinical sign of severe iron deficiency, occur in mountaineers who spend time at high altitudes, and be associated with conditions such as psoriasis, lichen planus, and trachyonychia, among others.5,44 (Fig. 8E and fig. F)
Pincer nails are characterized by an increased angle of the transverse axis in the nail distal region. Various factors can cause this condition, such as ill-fitting footwear, subungual exostosis, submatrix mucoid cysts, drugs (beta-blockers), osteoarthritis, local inflammatory or infectious nail disease, previous surgery in the area, or other.45 The degree of transverse axis involvement determines the appearance of 3 types of pincer nails: 1) type 1 or common pincer nail (trumpet or omega-shaped), where the distal transverse axis is very pronounced; 2) type 2 or tile shaped nail with an increased transverse curvature along the longitudinal axis; and 3) type 3 or plicated nail, with a flat curvature and well-demarcated lateral margins (Fig. 8G and fig. H). In extreme situations and chronic processes, the nail 2 distal edges may converge, damaging part of the nail bed (Fig. 7C and fig. D). In these cases, the nail can take on a tunnel or cone-like shape, or mimic congenital pachyonychia.5
FundingNone declared.
Conflicts of interestNone whatsoever.
I would like to thank all the patients who allow me to learn and enjoy observing their nail diseases day by day, and use the photographs.