The Coronavirus/COVID-19 outbreak, declared a Public Health Emergency of International Importance on January 30, 2020 by the World Health Organization, has in many countries exceeded the capacity of health systems to respond, due to its high contagiousness and the capacity to manage the deceased, due to its high fatality risk.
A review is necessary of the principal guidelines and protocols promoted by the institutions and the main scientific societies, aimed at containing the pandemic by adopting professional protection measures and appropriately managing the high number of cadavers.
The temporary mortuaries in an epidemic crisis and the classification of bodies according to infectious risk are analysed. In particular the resolutions issued by the health authorities are summarised and the protocols for dealing with deaths during the COVID-19 pandemic are described, including forensic autopsies.
El brote por el Coronavirus/COVID-19, declarado Emergencia de Salud Pública de Importancia Internacional el 30 de enero de 2020 por la Organización Mundial de la Salud, ha sobrepasado en numerosos países la capacidad de respuesta del sistema sanitario por su alta contagiosidad, y la de gestión de las personas fallecidas por su elevado riesgo de letalidad.
Se revisan las principales guías y protocolos promovidos por las instituciones y las principales sociedades científicas, orientados a la contención de la pandemia mediante la adopción de medidas de protección de los profesionales y a la adecuada gestión del alto número de cadáveres.
Se analizan los centros especiales de recogida de cadáveres en situación de epidemias y las clasificaciones de los cadáveres en función del riesgo infecto-contagioso. Específicamente se resumen las resoluciones dictadas por las autoridades sanitarias y se describen los protocolos de actuación ante fallecidos durante la pandemia COVID-19, incluyendo las autopsias forenses.
Throughout history humanity has suffered pandemics that notably affected world population. The Justinian Plague was one of the first to be described, and it devastated Constantinople from the year 541–543. It caused up to 10,000 deaths a day, leading to extremely severe problems in how to dispose of corpses. The Black Plague in the 17th century took 20 million lives in Europe. More recently, cholera epidemics spread around the world after 1816, and the Spanish Influenza of 1918, caused by an outbreak of the H1N1 subtype of influenza virus A, caused more than 40 million deaths worldwide. We are now faced by a third outbreak of coronavirus, after severe acute respiratory syndrome (SARS) in the years 2002–2003, with 919 deaths in 32 countries (a 10% mortality rate), and middle east respiratory syndrome (MERS) in 2012, with 858 deaths in 27 countries1 and a mortality rate of 37%.2
It is obvious that medical advances in recent decades have largely made it possible to control the lethal effects of the biological agents which cause pandemics, fundamentally due to the strengthening of the pharmacological arsenal and advanced life support systems. Nevertheless, the recent appearance of the disease caused by coronavirus (COVID-19) showed itself to be different from the first, as it caused more deaths in the first phases of the new epidemic than SARS and MERS combined.3 Hardly one month after it was declared a pandemic by the WHO, its highly contagious nature and severe involvement of the respiratory system placed the healthcare systems of a good number of countries in an extremely difficult situation.
Although its lethality was initially calculated to stand at from 2.2%4 to 2.6%,1 other publications set this rate at 3%, with a number of transmissions of from 1.5 to 3.5.2 In our country, data updated to 25 April show 10.24% (22,524/219,764), while worldwide it stands at 6.90% (187,705/2,719,896).5
Subjectively, COVID-19 causes mild infections among the general population, although the risk of death is higher among young adults than is the case for seasonal influenza. The mortality rate among older adults with comorbidities requires special attention.6
The said high rate of mortality saturated and even overwhelmed the systems for managing corpses in some geographical areas, in which the incidence of the disease was greater. This made it necessary to set guidelines for action in situations of this type.
Forensic Medicine has norms in association with another type of multiple victim events (MVE)—deliberate, accidental or natural—that clearly have the purpose of dealing with them swiftly after checking the main medical-legal questions. This regulation can be applied in practice in severe pandemics, adapting it to different aims and different death rates. Thus questions which are priorities in forensic protocols, such as identification or the determination of cause of death, are generally resolved previously for epidemics. On the other hand, epidemics are not restricted to one or several specific events, as the flow of dead individuals continues for an indeterminate period of time. They may surpass the capacity of institutions to respond not only occasionally, but in a way that is prolonged over time. In such cases the rapidity of processing and managing corpses with as much dignity as possible is highly important, as is the adoption of biosafety measures for those who handle them. All of the above considerations have to take into account all norms that enable the swift evacuation of victims, such as those for the COVID-19 crisis, which permit incineration or burial without the need for the regulation 24 h to pass, as before.7
History has shown that we have to be prepared for epidemics of microorganisms which were thought to be harmless at first.2 Outbreaks such as the one caused by SARS-CoV-2 underline the importance of preparing healthcare systems and the need to continue strengthening their capacity to respond.8 The 1918 outbreak of influenza led to changes from an “outdated public health system to what we now call the modern welfare state”.9 The latest crisis makes it necessary to revise the guidelines for action in terms of the overall management of pandemics, including the organisation and management of those who die because of them.
Special corpse collection centres in epidemic situationsThe state of emergency due to COVID-19, or any other pandemic, makes it necessary to have planned a response to the possibility that the corpse processing system (collection, preparation and subsequent incineration/burial) will be overwhelmed by large numbers of cases in hospitals, care homes and other places. Due to this, installations have to be planned that have sufficient resources to concentrate all of the resulting dead bodies in one or two places, depending on population levels, for conservation until their final destination. Funeral services overwhelmed by the existence of such a number of dead bodies that they cannot be managed rapidly will create a public health, human and social problem. This means that it is necessary to have a contingency plan that includes the necessary places and human and material resources to properly manage this situation. Concentrating the management of dead bodies minimises the risks of contagion and clears hospitals and other medical and social facilities, as well as funeral service installations.
The said installations should fulfil certain conditions of privacy, ease of access, enclosure and proximity to hospitals and medical-social centres. They should be equipped with changing rooms and a rest area, together with sufficiently powerful electrical connections for refrigeration equipment. Closed but accessible premises are therefore recommended, in zones protected against observation by the population to prevent any additional emotional impact. An indispensible condition is that they make it possible to conserve bodies at a temperature of from 2 °C to 4 °C.
Royal Decree (RD) 32/2009, of 16 January, which passed the Protocolo nacional de actuación Médico-forense y de Policía Científica en MVE,10 is specifically applicable to cases in which the judicial authority intervenes, together with scientific or judicial police teams and forensic doctors, to identify and analyse the causes of death in MVE. Nevertheless, it establishes a procedure with a series of actions that can be extrapolated for occasions associated with pandemics such as COVID-19, including cases in which no identification is necessary because of sufficient accreditation. This is especially so because forensic doctors are at the disposal of medical authorities during the state of emergency,11 and because they are experts in managing such situations due to their previous experience in MVE and natural disasters. Therefore, if necessary and coordinating with civil defence organisations and emergency coordination centres, forensic doctors may be assigned to the management of these installations while they are functioning, thereby adding additional medical resources to those of the Autonomous Communities (A.C.), which are then able to work in hospitals, primary care and medical-social care homes that are free of this occupation.
Dead body collection and management centres must have the following characteristics:
- -
Personnel: forensic doctors working in shifts are in charge of management, entry and exit control, checking documentation and the training of auxiliary staff. Administrative assistants in the collection centre will undertake the loading and unloading of bodies.
- -
Working protocol: this includes the documentation corresponding to the entry and exit of bodies, together with computerised registration of the same.
- -
Material: personal protective equipment (PPE).
- -
Security: security personnel, for access control as well as for citizen security.
- -
Maintenance staff for the installations to ensure the proper working of the same.
- -
Biological waste management.
- -
Installation cleaning and disinfection service.
- -
A staff rest area and canteen.
- -
Premises: once the usually used facilities are full, it will be necessary to have others. These include multipurpose sports centres, ice rinks, exhibition sites or sports pavilions where, if there is no suitable refrigeration system, it is possible to install refrigerated containers, lorries or tents. RD 32/2009 tasks the director of the Legal Medicine and Forensic Sciences Institute with the function of detecting such installations in coordination with the authorities, so that this function may and must be used in pandemics.
- -
Coordination with other institutions: the activation and deactivation of the said facilities must take place in coordination with Autonomous Community Emergency Centres or the body to which this competency is assigned.
In Spain, the Reglamento de Policía Sanitaria Mortuoria (RPSM), passed in 1974,12 classifies dead bodies into 2 major groups depending on the medical risk involved in their cause of death: group I includes the dead bodies of those whose cause of death is a medical hazard. This includes cholera, smallpox, anthrax and other causes defined by Resolution of the General Board of Health and published in the Official State Bulletin, together with dead bodies contaminated by radiation; group II includes all of the individuals who died for any cause not included in group I. The aim is to guarantee their conservation during storage or transport to their final destination in suitable hygienic and medical conditions.
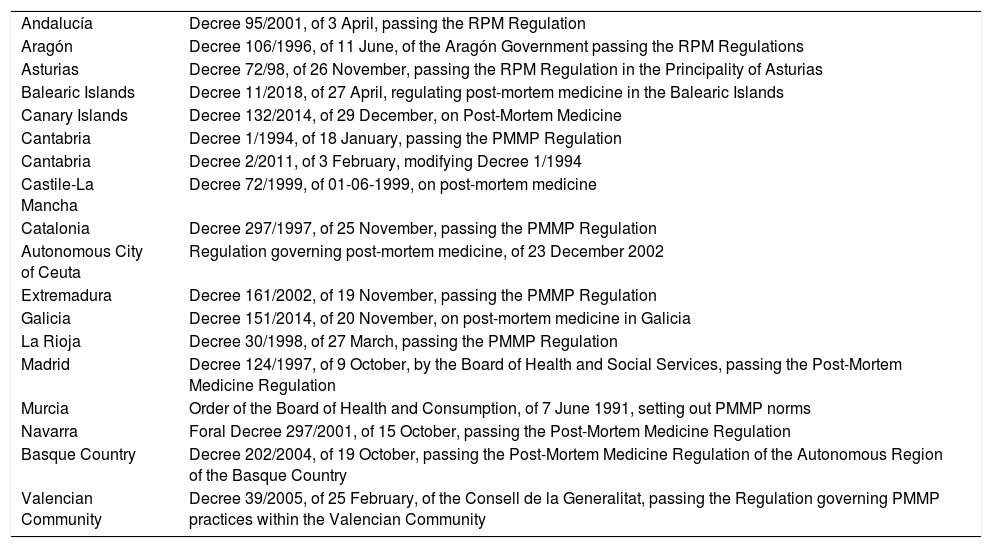
The classification contained in the RPSM no longer agrees with current social reality; in spite of this, it is still in force in some Autonomous Communities. Others within the scope of their powers have approved their own RPSM or specific norms which include modifications (Table 1), as they consider some risks associated with dead bodies to be insignificant now, as infectious-contagious diseases which were endemic in the past have now disappeared.13 The causes of death which represent a medical risk and classified as such in group i now include, with some variations between different A.C.,14 cholera, haemorrhagic fever caused by a virus, anthrax, plague and Creutzfeldt-Jakob encephalitis or other spongiform brain pathologies, as well as contamination by radioactive products (Table 2).
Autonomous Community Regulations for Post-Mortem Medical Practice (PMMP).
| Andalucía | Decree 95/2001, of 3 April, passing the RPM Regulation |
| Aragón | Decree 106/1996, of 11 June, of the Aragón Government passing the RPM Regulations |
| Asturias | Decree 72/98, of 26 November, passing the RPM Regulation in the Principality of Asturias |
| Balearic Islands | Decree 11/2018, of 27 April, regulating post-mortem medicine in the Balearic Islands |
| Canary Islands | Decree 132/2014, of 29 December, on Post-Mortem Medicine |
| Cantabria | Decree 1/1994, of 18 January, passing the PMMP Regulation |
| Cantabria | Decree 2/2011, of 3 February, modifying Decree 1/1994 |
| Castile-La Mancha | Decree 72/1999, of 01-06-1999, on post-mortem medicine |
| Catalonia | Decree 297/1997, of 25 November, passing the PMMP Regulation |
| Autonomous City of Ceuta | Regulation governing post-mortem medicine, of 23 December 2002 |
| Extremadura | Decree 161/2002, of 19 November, passing the PMMP Regulation |
| Galicia | Decree 151/2014, of 20 November, on post-mortem medicine in Galicia |
| La Rioja | Decree 30/1998, of 27 March, passing the PMMP Regulation |
| Madrid | Decree 124/1997, of 9 October, by the Board of Health and Social Services, passing the Post-Mortem Medicine Regulation |
| Murcia | Order of the Board of Health and Consumption, of 7 June 1991, setting out PMMP norms |
| Navarra | Foral Decree 297/2001, of 15 October, passing the Post-Mortem Medicine Regulation |
| Basque Country | Decree 202/2004, of 19 October, passing the Post-Mortem Medicine Regulation of the Autonomous Region of the Basque Country |
| Valencian Community | Decree 39/2005, of 25 February, of the Consell de la Generalitat, passing the Regulation governing PMMP practices within the Valencian Community |
The main infectious diseases which workers may be exposed to when handling corpses (professional risk).
| Form of transmission | Disease | Causal agent |
|---|---|---|
| Direct contact with the skin or contaminated objects | Invasive infection by group A streptococcus | Streptococcus pyogenes (group A) |
| MRSA | Methicillin-resistent Staphylococcus aureus | |
| Hand-mouth contact with faecal material or objects contaminated with the same | Typhoid. | Salmonella typhi |
| Hepatitis A | Hepatitis A virus | |
| Others | Salmonella no typhi | |
| Shigella dysenteryae | ||
| Cryptosporidium | ||
| Helicobacter pylori | ||
| Airways, through bioaerosols | Tuberculosis | Mycobacterium tuberculosis |
| Severe acute respiratory syndrome | SARS (coronavirus) | |
| Meningitis | Neisseria meningitidis | |
| Haemophilus influenzae | ||
| Diphtheria | Corynebacterium diphtheriae | |
| Contact with blood or other biological fluids, through the skin or mucosa (puncture wounds, cuts or damaged skin, splashes of blood or other biological fluids in the eyes, nose or mouth). | Hepatitis B | Hepatitis B virus |
| Hepatitis C | Hepatitis C virus | |
| Acquired immunodeficiency syndrome | Human immunodeficiency virus | |
| Contact with blood | Viral haemorrhagic fever | Ebola and Marburg virus |
| Lassa fever virus | ||
| Puncture wounds, cuts or splashes onto mucus membranes | Creutzfeldt-Jakob disease or transmissible spongiform encephalopathy | Prions |
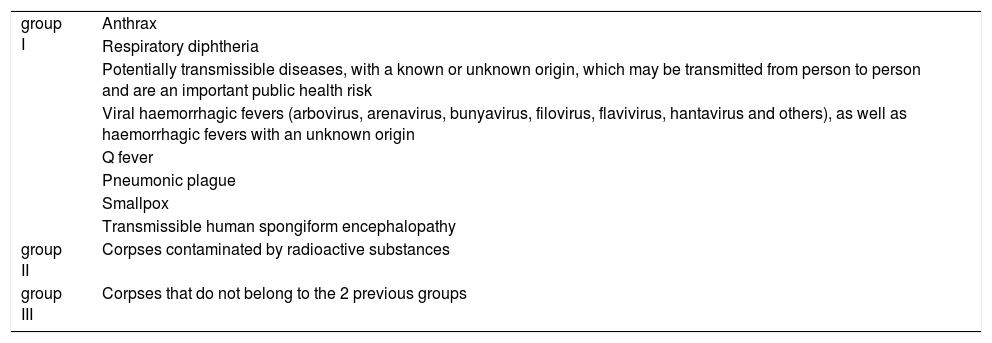
To agree the regulations governing Post-Mortem Medical Practice, which has sometimes led to disagreements in management due to the incompatibility of different A.C. regulations, in 2018 the Ministry of Health approved a Consensus Guide on Post-Mortem Medical Practice (Guía de consenso sobre sanidad mortuoria).15 This may be used as a standard by the A.C. and the National Government when drawing up or modifying their own regulations, thereby keeping shared and harmonised criteria. This guide classifies dead bodies, human remains and cadaveric remains in 3 groups; group I: those which are a risk for public or professional health, because the individual had one of the infectious-contagious diseases included in the appendix to the said guide, which may be modified according to available scientific evidence; group ii: those which give rise to a radiological risk because they contain radioactive substances or products, and which will be processed according to the regulations governing nuclear safety, and group III: those with none of the risks included in groups I and II15 (Table 3).
Appendix I of the Consensus Guide on Post-Mortem Medicine. Classification of corpses according to cause of death (15).
| group I | Anthrax |
| Respiratory diphtheria | |
| Potentially transmissible diseases, with a known or unknown origin, which may be transmitted from person to person and are an important public health risk | |
| Viral haemorrhagic fevers (arbovirus, arenavirus, bunyavirus, filovirus, flavivirus, hantavirus and others), as well as haemorrhagic fevers with an unknown origin | |
| Q fever | |
| Pneumonic plague | |
| Smallpox | |
| Transmissible human spongiform encephalopathy | |
| group II | Corpses contaminated by radioactive substances |
| group III | Corpses that do not belong to the 2 previous groups |
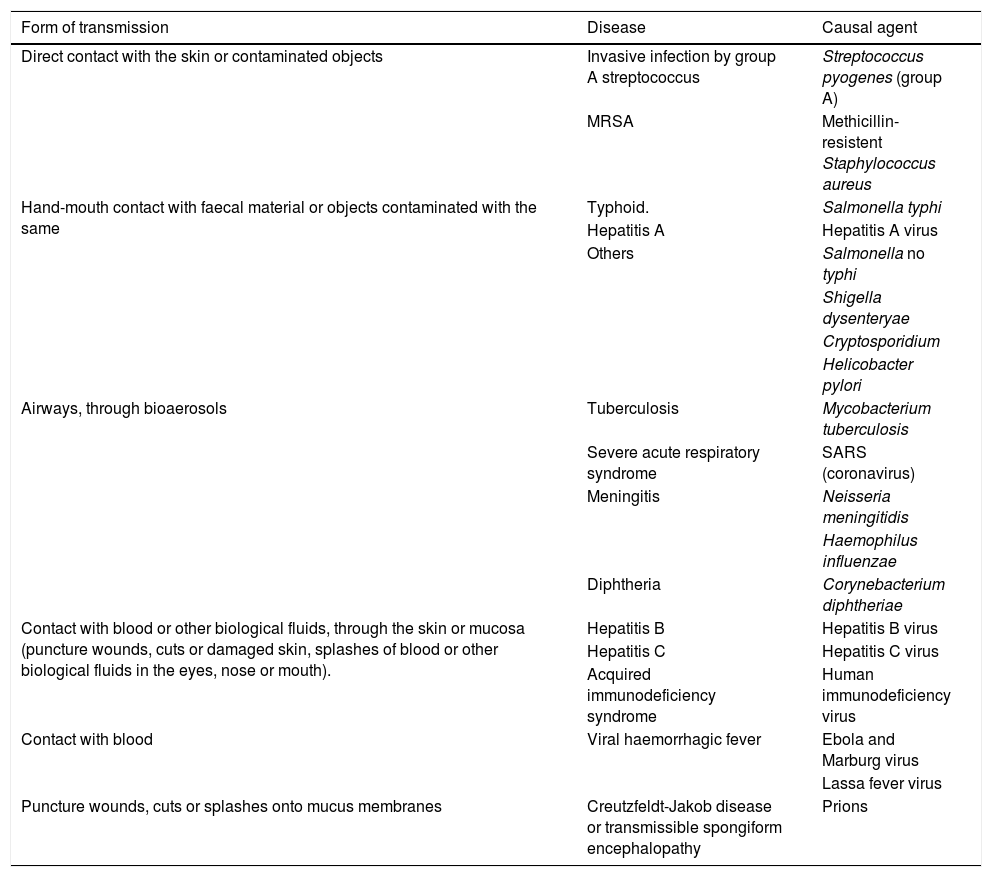
In the event of a major catastrophe, the existence of multiple victims is not a risk factor for the transmission of infectious-contagious diseases. Other circumstances have to be present if handling a dead body is to be considered a risk factor for public or professional health. These include bodies that are hosts to a disease present in endemic areas, or those which are infected by microorganisms that may remain alive after the death of the host, on condition that the environmental conditions necessary for this have been fulfilled. The elimination of any of these factors is decisive in determining a significant reduction in the risk of transmitting infectious-contagious diseases due to contact with a dead body.
When the main cause of death is infection, it has to be documented. Nevertheless, the cause of death is not always known, so that it is possible for professionals to be exposed to biological agents against which preventive or protective measures should be applied.16 Because of this, it is obligatory to adopt a series of standard measures, presupposing that every dead body may be a carrier of infectious agent, regardless of whether or not the cause and circumstances of death are known.
Medical decisions due to the pandemic and the state of emergency in connection with dead bodiesThe severe medical crisis caused by the COVID-19 epidemic made it necessary to draw up medical recommendations on the procedures for handling corpses and carrying out autopsies, including judicial ones. It was also necessary to issue specific regulations for Post-Mortem Medical Practice, especially after the declaration of the state of emergency on 14 March.17
The most relevant medical document is the Procedimiento para el manejo de cadáveres en casos de COVID-19,18 (Procedure for the Management of Dead Bodies in cases of COVID-19) published by the Ministry of Health and drawn up by the Sociedad Española de Anatomía Patológica (the Spanish Society of Anatomical Pathology), which by the end of this review had been published in 6 versions. It includes the bodies of those who have died due to COVID-19 in group 2 of the 1974 RPSM and in group 3 of the Consensus Medical Guide (dead bodies with no medical risk), although it states that “given that the corpse may constitute a biological risk, additional measures are proposed for handling it based on existing information and the applicable international recommendations”. Internationally, WHO Directive (2014) on the Prevention and control of acute respiratory infections with an epidemic and pandemic tendency during medical care19 stands out, as does the document published on 20 February 2020 by the European Centre for Disease Control (ECDC).20 The latter states that “there is no evidence for the transmission of SARS-CoV-2 through handling the corpses of individuals who died due to COVID-19, with a low potential risk of transmission, which is linked to direct contact with a corpse or its fluids, as well as with contaminated fomites, although, notwithstanding this, according to what has been observed with other respiratory viruses and applying the principle of precaution, it is considered that these corpses may give rise to the risk of infection for persons who make direct contact with them”.
The document covers the precautions to be taken with a dead body from its transport to the autopsy room, the performance of the clinical autopsy, which is applicable by analogy to medical-forensic autopsies, and subsequent actions, in which the risks deriving from handling the lungs and other organs are considered to be especially relevant, as they may contain live virus, and the washing of the intestines, so it is recommended not to perform an autopsy in cases of COVID-19 (+). In cases of death with or without respiratory symptoms, but with a justified clinical suspicion, it is recommended to perform the PCR test to rule out infection by SARS-CoV-2, and if the PCR test is negative, it is recommended to reach a decision by agreement with the hospital management. If an autopsy is considered necessary, it must be ensured that it takes place in a safe environment, complying with recommendations respecting PPE and the minimisation of aerosol production, recommending the performance of a partial autopsy by taking biopsies from the main organs. The number of individuals taking part in the autopsy must be reduced to the minimum, drawing up a list of all of the staff, who must themselves monitor their evolution and report the appearance of suspicious symptoms before proceeding to isolate themselves and undergoing diagnostic analysis.
This document classifies the residues produced as class iii, describes the characteristics of the PPE and the precautions applicable when putting it on and taking it off, to prevent the production of aerosols, while whenever possible restricting the use of electric saws, and if it is absolutely necessary to use one, then a vacuum suction system must be used. It also describes the precautions to be taken in cleaning the autopsy room and gives instructions to undertakers: information on the risk of COVID-19, the need to use protective measures similar to those recommended for medical personnel who treat COVID-19 patients, and the prohibition of carrying out thanatoaesthetic practices, thanatopraxis and interventions due to religious reasons that involve invasive procedures in the corpse.
Within the field of Forensic Medicine, on 20 March 2020 a meeting of the Technical Scientific Committee of the Forensic Medicine Board approved the “Recommendations due to the COVID-19 Pandemic”.21 This covered the whole field of expertise and more specifically medical-legal autopsies, with the instruction to “reduce the handling and transport of corpses subject to judicial investigation to the absolute minimum that is necessary, using to this end the precautions contained in art. 778.4 of the Law of Criminal Justice and art. 88 of the current Law of Civil Registration”.
Regarding the regulations on post-mortem medicine at national level, the following stand out:
- -
Order SND/272/2020 of 21 March, which regulates the “exceptional measures to expedite the burial licence and final destination of dead bodies in the situation of medical crisis caused by Covid-19”7;
- -
Order SND 296/2020 of 27 March, on “exceptional measures for the transport of dead bodies in the situation of medical crisis caused by Covid-19”,22 and
- -
Order SND/298/2020 of 29 March, on “exceptional measures and funeral ceremonies to limit the propagation and contagion of COVID-19”.23
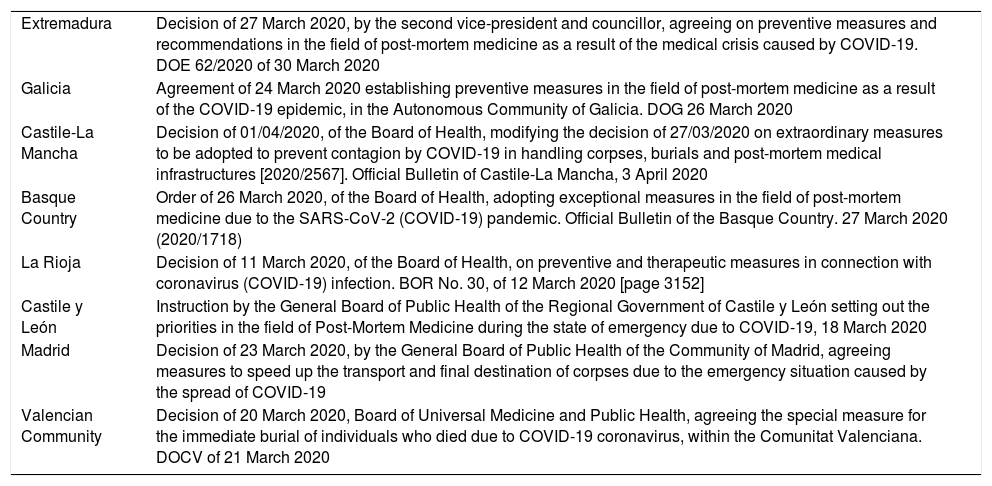
The regulations of the autonomous communities, published by practically all of them, develop state regulations for their own territory with few variations. The Canary Island regulations stand out,24 as they include dead bodies due to COVID-19 within group 1 of the Consensus Guide on Post-mortem Medicine. Table 4 shows the regulations issued by the different A.C. in connection with the pandemic.
Autonomous Community Regulations in connection with the COVID-19 pandemic.
| Extremadura | Decision of 27 March 2020, by the second vice-president and councillor, agreeing on preventive measures and recommendations in the field of post-mortem medicine as a result of the medical crisis caused by COVID-19. DOE 62/2020 of 30 March 2020 |
| Galicia | Agreement of 24 March 2020 establishing preventive measures in the field of post-mortem medicine as a result of the COVID-19 epidemic, in the Autonomous Community of Galicia. DOG 26 March 2020 |
| Castile-La Mancha | Decision of 01/04/2020, of the Board of Health, modifying the decision of 27/03/2020 on extraordinary measures to be adopted to prevent contagion by COVID-19 in handling corpses, burials and post-mortem medical infrastructures [2020/2567]. Official Bulletin of Castile-La Mancha, 3 April 2020 |
| Basque Country | Order of 26 March 2020, of the Board of Health, adopting exceptional measures in the field of post-mortem medicine due to the SARS-CoV-2 (COVID-19) pandemic. Official Bulletin of the Basque Country. 27 March 2020 (2020/1718) |
| La Rioja | Decision of 11 March 2020, of the Board of Health, on preventive and therapeutic measures in connection with coronavirus (COVID-19) infection. BOR No. 30, of 12 March 2020 [page 3152] |
| Castile y León | Instruction by the General Board of Public Health of the Regional Government of Castile y León setting out the priorities in the field of Post-Mortem Medicine during the state of emergency due to COVID-19, 18 March 2020 |
| Madrid | Decision of 23 March 2020, by the General Board of Public Health of the Community of Madrid, agreeing measures to speed up the transport and final destination of corpses due to the emergency situation caused by the spread of COVID-19 |
| Valencian Community | Decision of 20 March 2020, Board of Universal Medicine and Public Health, agreeing the special measure for the immediate burial of individuals who died due to COVID-19 coronavirus, within the Comunitat Valenciana. DOCV of 21 March 2020 |
RD 32/2009 passed the National Protocol for medical-forensic and scientific police action in MVE. It centres on forensic medical activity in the identification of bodies and the determination of the causes and circumstances of death.10 The current situation is different, as there are a high number of deaths every day and a risk of infection for the individuals who handle corpses or perform necroscopic examinations in confirmed and probable cases, those under investigation or even undiagnosed and asymptomatic cases.25–27 Due to this, it is necessary to establish protocols and recommendations to ensure the suitable management of dead bodies and minimise the propagation of the virus, and that all procedures take place as smoothly as possible.
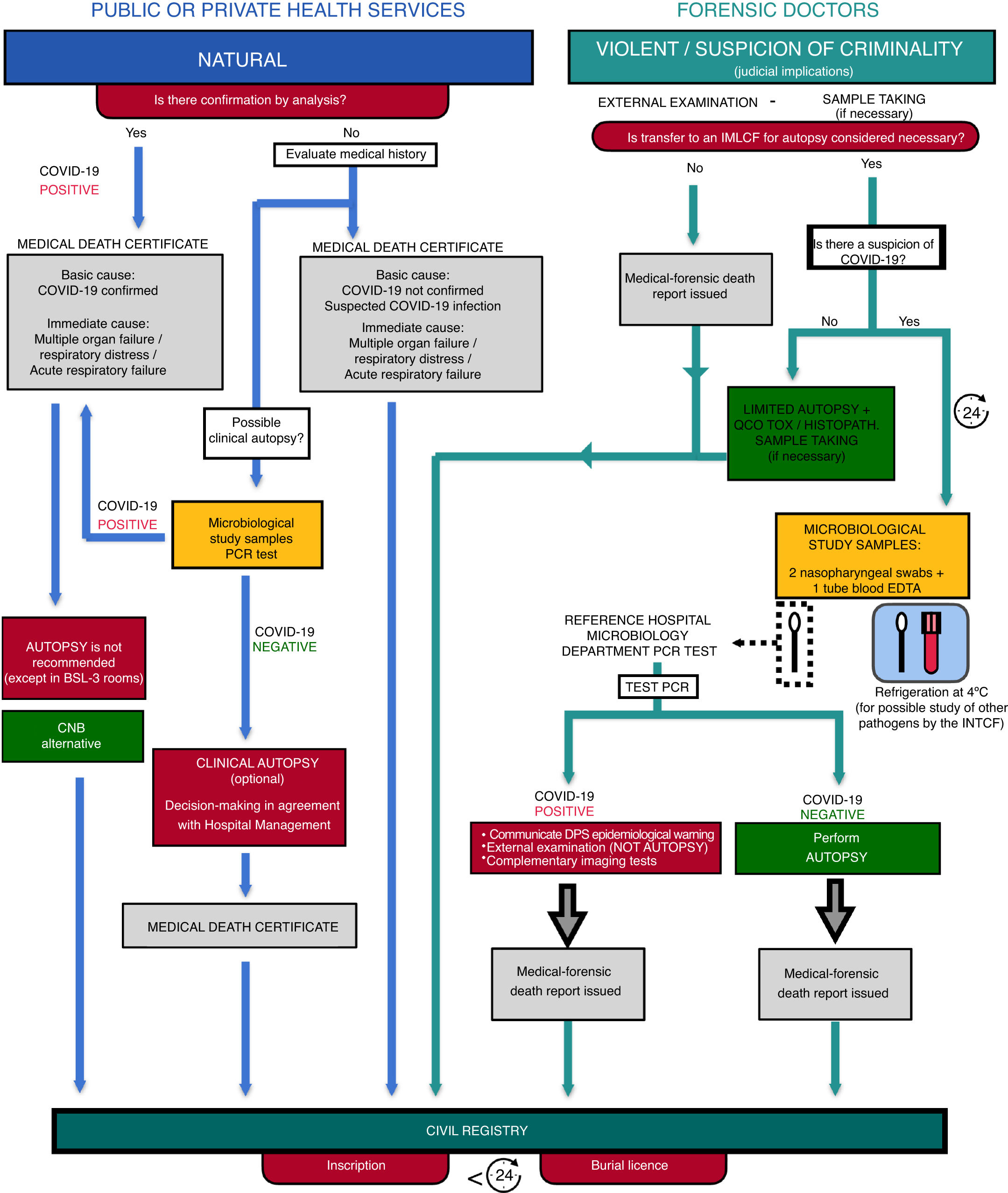
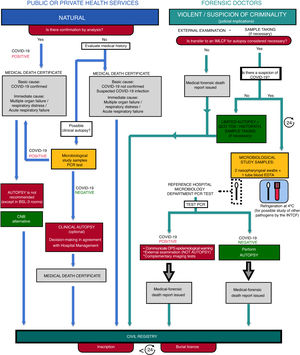
Coordination with medical authorities is necessary to ensure proper management of death certificates and judicial actions, favouring the rapidity and flexibility of the necessary processes. The Ministry of Health therefore published the above-mentioned technical document which regulates the procedure for processing the dead bodies of COVID-19 cases.18 This document is continuously revised, and together with the recommendations of the General Board of Official Medical Associations,28 the Forensic Medicine Council21 and the Spanish Society of Forensic Pathology,29 they make it possible to establish an initial protocol to govern the actions of the public and private health services, as well as those by forensic doctors in cases of death during the COVID-19 pandemic (Fig. 1).
Cases of natural death correspond to doctors who work in healthcare, and they issue the corresponding death certificate in the case of previous analytic confirmation or if medical history leads to the suspicion of infection by COVID-19.28 Although it is not recommended to perform autopsies in positive COVID-19 cases, the Autopsy Work Group of the Spanish Society of Anatomical Pathology accepts the possibility of practising a core needle biopsy in principle in these situations, instead of a standard autopsy.30 Once the initial phase of the medical crisis had passed, it then accepted the performance of clinical biopsies solely within autopsy rooms that meet the BSL-3 biosafety standards.
The work of forensic doctors should preferentially centre on cases of violent death, ones in which there is a clear suspicion of criminality or in certain special circumstances, such as death while in custody.31 In these situations forensic doctors collect all of the information relating to a case. They examine the scene where events took place externally and assess the need for transfer to the IMLCF (Legal Medicine and Forensic Sciences Institute) based on existing judicial consequences, and it may be agreed that no autopsy will be performed, by applying article 778.4 of the Law of Criminal Trial.
In the case of transfer to the IMLCF without the suspicion of COVID-19, then a restricted autopsy will be considered sufficient, respecting the recommendations made above; additionally, only samples that are necessary for histopathological studies will be taken.29 Even minimally invasive autopsies have been proven to be useful in cases of systemic viral and bacteria infections.32,33
In the case of transfer to the IMLCF with suspicion of infection by COVID-19, waiting for 24 h. after death is recommended before performing the autopsy, taking samples beforehand to analytically confirm a positive result for COVID-19, with the recommendation to only perform an external examination and complementary imaging tests (radiography or post mortem computed tomography) that help to find sufficient signs that explain the cause and circumstances of death,33,34 or a negative result that makes it possible to perform a complete autopsy.
The Ministry of Health technical document also considers social distancing measures to prevent the spread of the virus, making it advisable to suspend wakes and funeral ceremonies.18
Respecting the final destination of the corpse, burial or cremation, Order SND/272/2020, of 21 March, which established exceptional measures to expedite burial licences and the final destination of dead bodies in medical crisis caused by COVID-19, speeds up the process of inscription in the Civil Registry and the issue of the burial licence, so that less than 24 h. may pass before it takes place. To gain speed and flexibility in these processes, this acceleration is applicable to all dead bodies regardless of the cause of death.7
For transport, corpses must be placed in a specific impermeable body bag or in 2 open impermeable shrouds sprayed with disinfectant or a solution of sodium hypochlorite. A normal coffin may be used without requiring any special precautions, and it should be taken as soon as possible to the mortuary prepared for this purpose, the morgue, or directly to the crematorium or for burial. All of the personnel who work in this transport must always use protective measures in the form of PPE.18
Due to the high number of deaths every day, it is necessary to prepare the special centres described above, to prevent or delay putrefaction until final transport.35
If international transport is necessary, this must take place according to the law now in force.36 Cremation is the most favourable situation, given that handling ash is completely risk-free and its transport is not subject to any medical regulations. If cremation is not performed, it will be necessary to use transitory preservation techniques that do not involve handling the corpse, and embalming corpses with confirmed or suspected COVID-19 is not recommended.37
Forensic autopsy in situations of riskAlthough in general the main form of transmission of SARS-CoV-2 is through particles resulting from coughing or aerosols, or due to contaminated hands, any surface may carry the pathogenic agent. They are known as passive vectors, such as skin cells, hair, clothing, sheets or personal belongings.25
Unless aerosols are created by using an electric saw, during autopsy the basic risk arises from contact with infectious materials and especially fluids. Nevertheless, if an individual dies because of COVID-19, their lungs and other organs may contain the virus.38
Due to this, forensic autopsies of possible cases and most especially of confirmed cases, especially those with no signs of violence, must be reduced to the minimum and only be performed when absolutely necessary. Even so, and given that our law permits this, internal examination of the corpse must be avoided.39
The installations for autopsies of this type have to be specific and they must be equipped with far stricter biosafety measures than the usual facilities.40
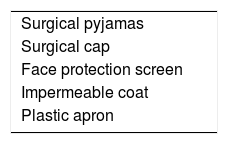
Nevertheless, the risk may be drastically reduced if autopsies are performed under conditions with a certain degree of safety and suitable personal protective equipment41 (Table 5).
Minimum recommended personal protective equipment.
| Surgical pyjamas |
| Surgical cap |
| Face protection screen |
| Impermeable coat |
| Plastic apron |
To reduce risk to the maximum in autopsies or examinations only one forensic doctor and an assistant will intervene, always keeping a safe distance from each other. When due to legal questions 2 experts have to be present, and one of them will act as an observer.
As is usual in forensic practice, before commencing post-mortem study the greatest amount of data possible has to be gathered on the clinical history of the dead individual to facilitate the medical-legal study of their death. However, if the corpse is suspected of infection by COVID-19, as well as examining their medical and personal history we should check for previous symptoms that are compatible with coronavirus infection (fever, coughing and respiratory problems) as well as possible recent contacts that they may have had with sick people.
If there is the slightest suspicion, some professionals recommend covering the mouth and nasal orifices of the corpse with a mask or compress to prevent emanations while the corpse is moved, so that it arrives at the autopsy table in this condition.
It is well-known that studying clothing in forensic medicine may sometimes offer valuable information. However, given the risk of possible contagion, and most especially in cases of deaths that were apparently natural, a short description and photographic report may be sufficient, as it seems that SARS-CoV-2 virus may remain on the surface of clothing for 1 or 2 days.42 The personal effects that the dead individual may carry, such as documents, a watch or jewellery, etc., must like clothing be considered to be contaminated and they should not be collected, unless due to specific circumstances it is possible to guarantee their sterilisation.
To conclude, in forensic practice 2 basic situations may arise:
- -
In the case of natural deaths, without prejudice to the decisions of the corresponding judicial authority, and following the recommendations for managing COVID-19 corpses described above, it is recommended that no autopsy be performed. After gathering data and examining the corpse externally, if necessary minimally invasive sample-taking may be performed for toxicological study.
- -
In the case of violent deaths or those with a suspicion of criminality a more exhaustive external examination is to take place, with the corresponding photographic report. If internal examination is indispensible, this will be targeted to specific anatomical zones or organs. It is not recommendable to extract organs, especially the lungs. The cranial cavity, as was pointed out above, must only be examined in exceptional cases due to the risk of the formation of aerosols while it is opened.
The authors have no conflict of interests to declare.
Please cite this article as: González-Fernández J, Ibáñez-Bernáldez M, Martínez-Tejedor JA, Alama-Carrizo S, Sánchez-Ugena F, Montero-Juanes JM. Gestión de los cadáveres durante la pandemia por COVID-19 en España. Rev Esp Med Legal. 2020;46:109–118.