To evaluate the influence of dental fluorosis and etching time on the shear bond strengths (SBSs) of orthodontic brackets to human enamel.
MethodsA total of 48 human maxillary central incisors, extracted for periodontal reasons were used. The sample was divided into three experimental groups (n=16): group H30 with healthy teeth and group F30 and F60 with fluorosed teeth (Thylstrup and Fejerskov Index scores 3–4). After etching the dental enamel with 35% phosphoric acid for 30s (groups H30 and F30) or for 60s (group F60), metal orthodontic brackets were bonded with Transbond XT adhesive system and light cured (1200mW/cm2 for 10s). The specimens were then thermocycled (5–55°C, 500 cycles), stored in distilled water (37°C/7 days), and tested in shear (Instron, 1KN, 1mm/min). Failure mode was classified, with a stereomicroscope (20× magnification), according to the adhesive remnant index (ARI). SBS data were statistically analyzed with 1‐way ANOVA, followed by Tukey post hoc tests (α=0.05). Kruskal–Wallis and Mann–Whitney nonparametric tests were used to analyze failure data (α=0.05).
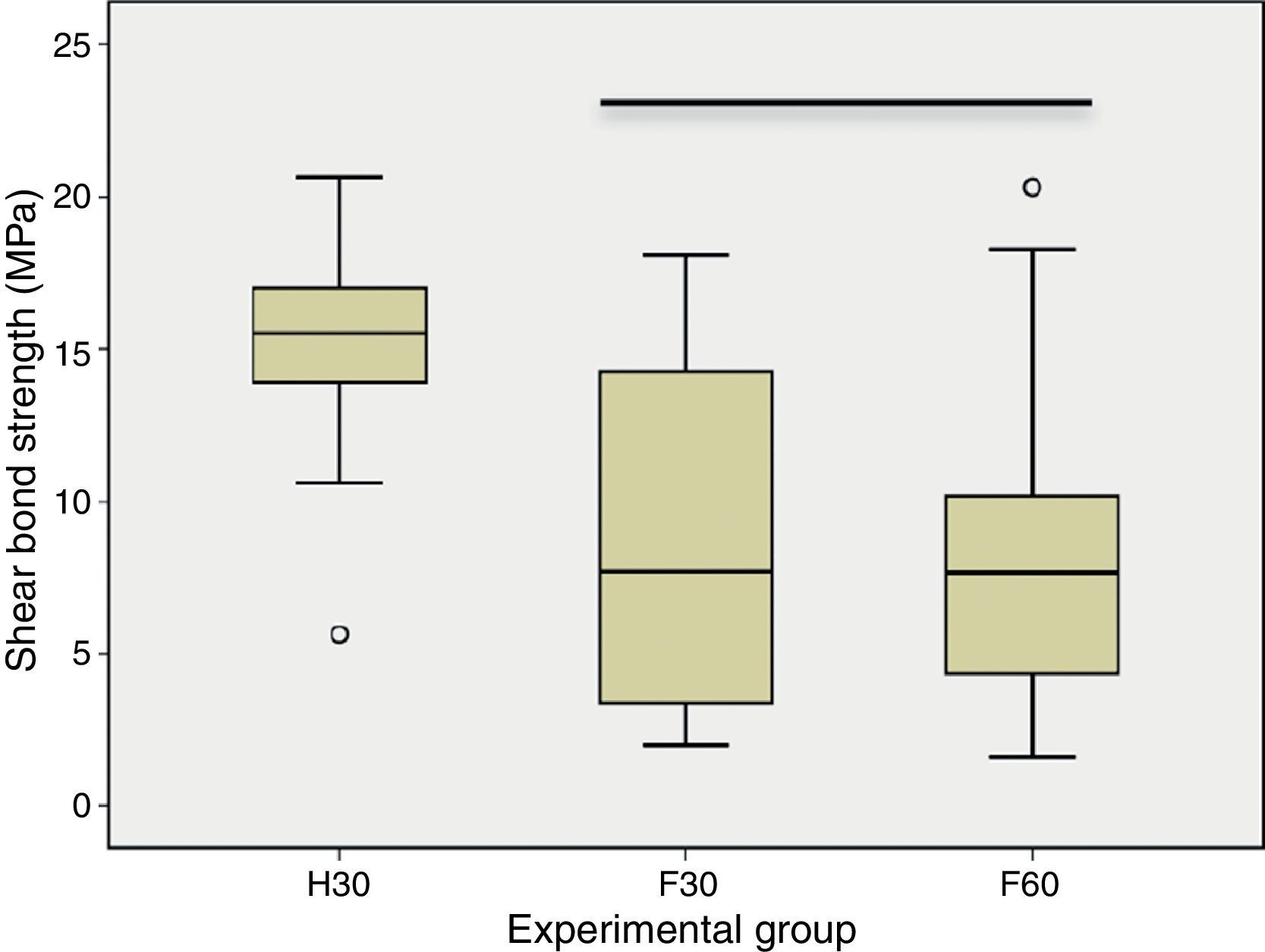
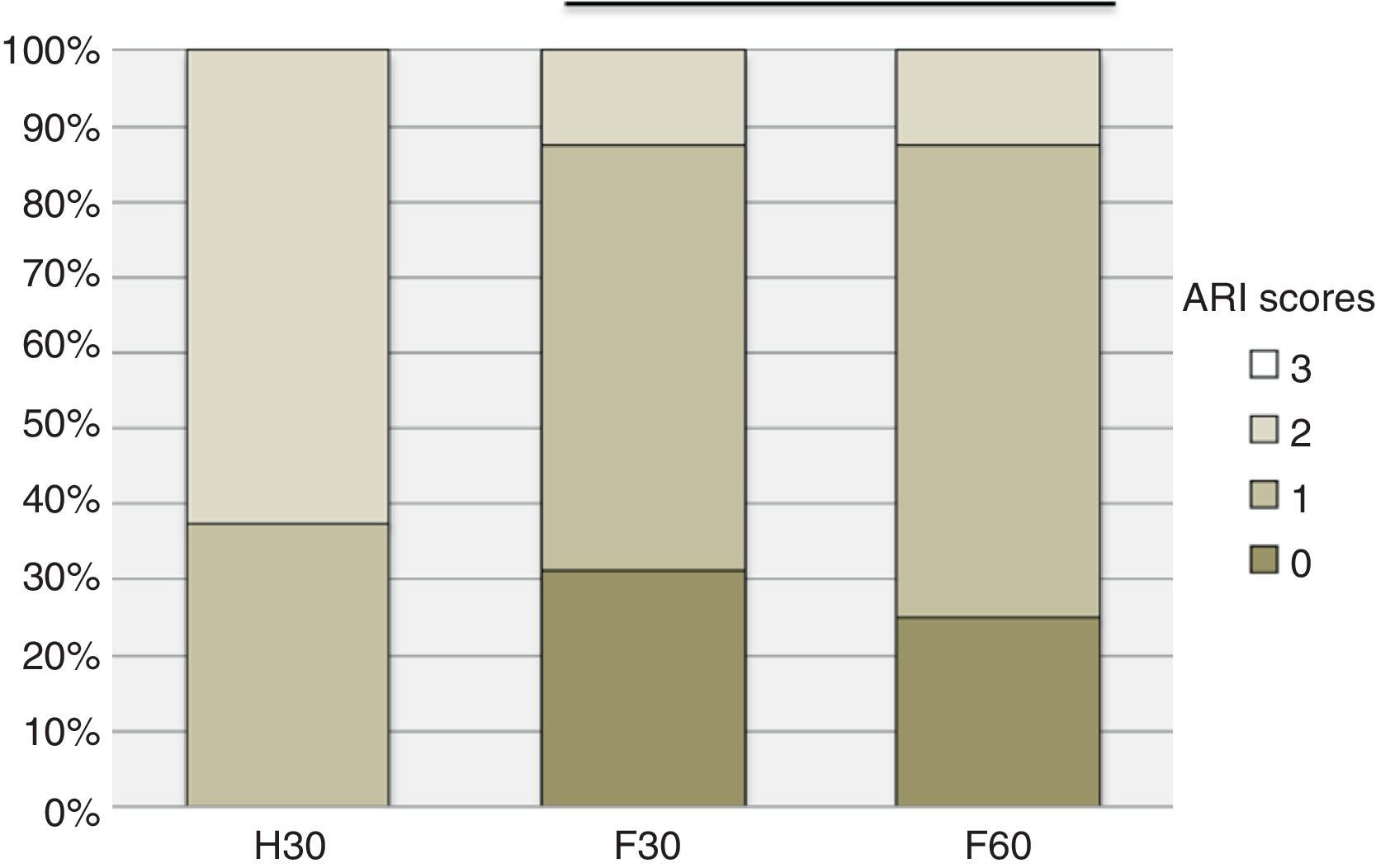
ResultsNo statistically significant (p=0.763) differences were found between F30 and F60, but these groups showed a statistically (p<0.05) lower bond strength values than H30. The non‐fluorosed group showed a significantly (p<0.05) higher ARI score than the other groups.
ConclusionOrthodontic brackets adhesion to enamel is negatively influenced by dental fluorosis. Doubling the etching time in fluorosed teeth was not enough to produce similar results to those observed in the healthy ones.
Avaliar a influência da fluorose e do tempo de condicionamento ácido sobre a resistência adesiva ao corte de brackets ortodônticos colados ao esmalte.
Métodos48 incisivos centrais maxilares humanos, extraídos por razões periodontais, e divididos em três grupos experimentais (n=16): grupo H30 com dentes sem fluorose e grupos F30 e F60 com dentes com fluorose (Índice de Thylstrup e Fejerskov, classificação 3–4). Após o condicionamento do esmalte com ácido fosfórico a 35% durante 30 segundos (H30 e F30) ou durante 60 segundos (F60), foram cimentados brackets metálicos com o sistema adesivo Transbond XT e fotopolimerizados (1200mW/cm2 durante 10 segundos). Os espécimes foram termociclados (5–55°C, 500 ciclos), armazenados em água destilada (37°C/7 dias), e testados ao corte (Instron, 1KN, 1mm/min). A falha foi classificada, com um estereomicroscópio (ampliação 20x), de acordo com o Índice de Adesivo Remanescente (ARI). Os dados de resistência adesiva foram analisados com ANOVA e comparações múltiplas segundo Tukey (α=0,05). Os testes de Kruskal‐Wallis e Mann‐Whitney foram utilizados para analisar os dados da falha (α=0,05).
ResultadosNão foram encontradas diferenças estatisticamente significativas (p=0,763) entre F30 e F60, mas estes grupos apresentaram valores de resistência adesiva estatisticamente (p<0,05) mais baixos que os obtidos em H30. O grupo H30 apresentou uma classificação ARI estatisticamente (p<0,05) superior aos grupos F30 e F60.
ConclusõesA adesão de brackets ortodônticos ao esmalte é negativamente influenciada pela fluorose dentária. A duplicação do tempo de condicionamento ácido nos dentes com fluorose não foi suficiente para promover resultados similares aos observados nos dentes sem fluorose.
Due to the fluoride ion anticariogenic properties, a decrease in dental caries prevalence occurred, in the last decades.1–3 When enamel remineralization cycles happen in the presence of fluoride ions, the hydroxyl groups of the hydroxyapatite are replaced by fluoride leading to a stronger and less soluble structure, the fluoroapatite.4 However, as a result of its widespread use, there was also an exponential increase in fluorosis prevalence.3,5–10
Dental fluorosis is a developmental tooth enamel lesion resulting from a fluoride overdose and chronic ingestion during early childhood.8,11 This condition leads to metabolic changes in ameloblasts, resulting in a poor matrix formation and tooth calcification.11,12 The fluorosed enamel is characterized by a hypermineralized outer layer and a hipomineralized and porous sublayer.13–16
Etching the enamel surface with acids such as phosphoric acid is an important step to promote adhesion to dental enamel. The acid etching technique, introduced by Buonocore17 in 1955, causes a selective decalcification of enamel, creating a rough surface and increasing the contact area and surface energy which provides the substrate for infiltration of the bonding agent making possible the micromechanical union between the adhesive/restorative materials and the enamel surface.4 However, the adhesion to enamel of fluorosed teeth may be compromised, due to the etching procedure that has been proven to be less effective in these hypermineralized surfaces.18–20 Some authors advocate the increase of etching time in order to overcome such limitation.20–22
Orthodontic treatment with fixed appliances requires an adequate bond between brackets and tooth enamel, and may be a clinical challenge in endemic fluorosis regions. If bond strength values are too low, earlier debonding of brackets may occur as a result of normal clinical stress, forcing a delay and increasing treatment costs.23
The available studies that assess the adhesion of orthodontic brackets to teeth with fluorosis are scarce and show different results.20,22,24–27
The aim of this study is to evaluate the influence of dental fluorosis and the etching time on the shear bond strength of metal orthodontic brackets to human enamel. The null hypotheses tested were that fluorosis does not decrease the bond strength and doubling the etching time does not increase the adhesion of orthodontic brackets to fluorosed enamel.
Materials and methodsThe sample size (n=16) was estimated with a power analysis to provide statistical significance alpha=0.05 at an 80% power.
The sample consisted of 48 human upper central incisors extracted for periodontal reasons, and the study was approved by the Institutional Research Ethics Committee. Teeth were collected after receiving verbal consent and stored in 0.5% chloramine solution at 4°C for a week followed by immersion in distilled water at 4°C until bonding procedures. The criteria for study inclusion were absence of previous chemical treatment, caries and buccal surface cracks and restorations. Healthy teeth composed group H30. Mild to moderated fluorosed teeth were selected by consensus between two observers according to the Thylstrup and Fejerskov Index (ITF) scores 3–4, and randomly allocated to groups F30 and F60.28
Before bonding, buccal surfaces were cleaned with a mixture of water and non‐fluoride pumice, thoroughly rinsed with water spray and air‐dried.
The enamel of buccal surface specimens was etched with 37% phosphoric acid gel (Transbond™ XT Etching Gel, 3M Unitek, Monrovia, EUA), for 30s for group H30 and F30, and 60s for group F60. All teeth were rinsed with water spray for 15s and dried with oil‐free compressed air for 5s, until characteristic frosty white enamel etched appearance was present.
Metal brackets (Victory Series™ Standart edgewise Bracket Univ U Central, 3M Unitek, Monrovia, USA) were bonded with Transbond XT (3M Unitek, Monrovia, USA) according to the manufacturer's instructions. A thin uniform layer of adhesive primer was applied with a microbrush on the etched buccal enamel surface. The light cured orthodontic adhesive was applied on the base of the bracket and this was immediately positioned onto the tooth surface and pressed firmly in the desired position. Excessive resin was gently removed with a dental probe and thereafter cured (LED CV‐218, Technoflux, Barcelona, Spain) with an output of 1200mW/cm2 for 10s (5s at each of the mesial and distal bracket edge).
The specimens were set in self‐cured acrylic block, thermocycled (5–55°C, 500 cycles), and stored in distilled water at 37°C for 7 days, before tested in shear.
Bond strengths were measured on a universal testing machine (Instron model 4502, Instron Ltd., Bucks, England), using a wire loop applied under the gingival wings of the bracket, in order to induce gingival‐oclusal shear stress at the adhesive interface. Shear bond strength (SBS) tests were performed at a crosshead speed of 1mm/min and load cell of 1kN, until failure occurred. Failure load values (N) were recorded and converted into megapascals (MPa), dividing the failure load by the surface area of the bracket base.
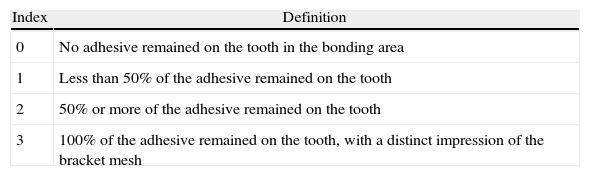
After debonding, teeth and brackets were examined with a stereomicroscope (Meiji Techno, model EMZ‐8TR, Meiji Techno Co. Lda, Saitama, Japan) at magnification of 20×, to assess the amount of adhesive remaining on the teeth and the failure mode was scored according to the adhesive remnant index (ARI) (Table 1).29,30
Adhesive remnant index (ARI).
| Index | Definition |
| 0 | No adhesive remained on the tooth in the bonding area |
| 1 | Less than 50% of the adhesive remained on the tooth |
| 2 | 50% or more of the adhesive remained on the tooth |
| 3 | 100% of the adhesive remained on the tooth, with a distinct impression of the bracket mesh |
Data were statistically analyzed using IBM SPSS Statistics 20 software (SPSS Inc., Chicago, IL, USA). After assessing normality and homoscedasticity with Kolmogorov–Smirnov and Levene's tests, SBS data were submitted to one‐way ANOVA, followed by Tukey post hoc tests. Kruskal–Wallis followed by Mann–Whitney with Bonferroni correction nonparametric tests were used to analyze failure mode data. Statistical significance was identified at alpha=0.05.
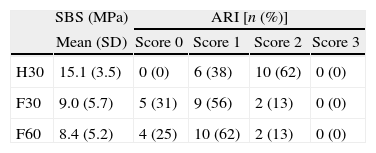
ResultsThe mean SBS ranged from 8.4MPa for the fluorosed teeth etched for 60s (F60), to 15.1MPa for H30 with healthy specimens (Table 2). According to 1‐way ANOVA and Tukey post hoc tests, mean SBS yielded in both groups with fluorosed teeth (F30 and F60) were significantly (p<0.05) lower than that with non‐fluorosed teeth (H30). No significant (p=0.978) difference was found between F30 and F60, the two groups with fluorosed teeth (Fig. 1).
The distribution of failure ARI score by experimental groups is presented in Table 2 and Fig. 2. No cohesive failures (score 3) were observed. Failure mode was predominantly mixed (scores 1 and 2) but the ARI score of H30 non‐fluorosed teeth was significantly (p<0.05) higher than those achieved in fluorosed teeth (F30 and F60). Adhesive failures were found only for F30 and F60.
DiscussionBonding orthodontic brackets to fluorosed teeth remains a difficult task due to the lower acidic solubility of fluoroapatite, present at high concentration in the external enamel layer.18–20 The reduction of enamel solubility is related to the presence of larger apatite crystals, better crystallinity, and the buffering action of fluoride released by enamel crystals during initial stages of etching.31
The present study was designed to evaluate the effects of fluorosis and etching time on shear bond strengths of orthodontic brackets.
Thermal cycling was performed, according to the ISO 11405 specifications for testing adhesion to tooth structure. This procedure could be controversial but all specimens were treated in the same way, although it has been stated that 500 cycles do not stand for a sufficient amount of aging.32,33
Significantly lower bracket bond strength values were found in the fluorosed enamel than those achieved in non‐fluorosed teeth. Consequently, the first null hypothesis tested was rejected. These results are in agreement with previous studies18,20,24; nevertheless some others showed no effect of fluorosis on bond strength.22,26 This inconsistency and conflicting results may be explained by the differences observed between the fluorosis severity of the teeth used in the different studies. It was shown that the increase of fluorosis severity leads to a lower bond strength.20,34 For this study, mild to moderate fluorosed teeth (TFI=3–4) were collected in the Azores Islands (São Miguel), a fluorosis endemic area, where fluoride contents in drinking water reaches concentrations higher than 1ppm.35
In order to overcome the lower enamel solubility in teeth with fluorosis, some authors advocate the extension of etching time.20–22 It has been recommended to etch healthy teeth for 15–30s, enamel with mild and moderate fluorosis for 30s, and etching enamel with severe fluorosis at least for 60–90s.13,36,37
In the present investigation, the second null hypothesis tested could not be rejected. An increase in etching time, from 30 to 60s, on mild to moderate fluorosed teeth was not enough to achieve bond strengths as high as the ones yielded with non‐fluorosed teeth. A previous study, also found no increase in bracket bond strength to teeth with moderate and severe fluorosis, by extending the etching time from 15s to 150s.20
However, obtaining higher bond strengths may not be a critical issue. The adhesion achieved should be enough to withstand the stress produced in clinical situations, but extremely high bond values may induce enamel fractures during bracket debonding and increase the difficulty of the adhesive remnants removal, at the end of the treatment.20 It has been suggested that obtaining bracket bond strength values ranging from 6 to 8MPa will be sufficient to ensure a good clinical performance.38 Regardless of the lower bond strength observed with fluorosed teeth when compared with non‐fluorosed teeth, the mean bracket bond values achieved in all experimental groups were higher than those mentioned above. Nonetheless, it is known that several factors may influence the bond values, such as the mechanical test configurations used.39–41 The lack of uniformity in the methodology of previous publications limits the comparability of the bond values between studies and their extrapolation to clinical behavior.
The failure mode observed was in accordance with the SBS values. The 25–30% of adhesive failures found in fluorosed groups may suggest that in these groups the union between the enamel and the orthodontic adhesive is not so strong as in healthy teeth. This result was also consistent with previous studies where higher ARI scores are observed with increased bond strength values.20,24,27
Further studies should be performed to evaluate the influence of different types of fluorosis, etching time and orthodontic adhesives on bracket bond strength, and to evaluate long‐term durability of the bond. Clinical studies are also desirable.
ConclusionOrthodontic brackets adhesion to tooth enamel is negatively influenced by dental fluorosis. Doubling the etching time does not increase the adhesion of orthodontic brackets to fluorosed enamel.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank 3M Unitek for providing the materials for this study. This work was performed at UICOB, R&D unit no. 4062 of FCT.


![Box‐plot of shear bond strengths (MPa) [horizontal line indicates statistical similar groups (p≥0.05)]. Box‐plot of shear bond strengths (MPa) [horizontal line indicates statistical similar groups (p≥0.05)].](https://static.elsevier.es/multimedia/16462890/0000005500000002/v1_201407220031/S1646289013001805/v1_201407220031/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![Adhesive remnant index (ARI) scores distribution by experimental groups [horizontal line indicates statistical similar groups (p≥0.05)]. Adhesive remnant index (ARI) scores distribution by experimental groups [horizontal line indicates statistical similar groups (p≥0.05)].](https://static.elsevier.es/multimedia/16462890/0000005500000002/v1_201407220031/S1646289013001805/v1_201407220031/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
