To assess and compare five diagnostic imaging methods used in the identification of periapical diseases, of different diameters, mechanically simulated.
MethodsThe sample of the present study consisted of 12 dried human mandibles. Digital panoramic radiography, conventional and digital periapical radiography (charged couple device and photo-stimulable phosphor plate), and high-resolution cone beam computed tomography (CBCT) were previously performed to exclude regions presenting periapical lesions or similar conditions, which then formed the control and experimental groups. Then, periapical diseases were progressively produced with drills of different diameters, thus creating lesions of different sizes. The different image diagnosis methods were applied after each lesion produced. The data were assessed using the Kappa test, ROC curve graphs and Cochran's Q test. The significance level was set at 0.05.
ResultsThe images obtained with conventional film and digital panoramic radiography showed the worse results (0.65 and 0.55, respectively), and statistically significant differences compared to the controls (p<0.05) for lesions artificially produced with #6 drill. With regard to high-resolution CBCT, the area values were found to be high for all lesion sizes.
ConclusionConventional periapical radiography and digital panoramic radiography did not provide satisfactory images for the identification of incipient periapical diseases. The high-resolution CBCT showed high accuracy in the diagnosis of periapical diseases in both regions evaluated, and proved to be the most reliable method for the identification of initial periapical diseases (1.8mm).
Avaliar e comparar 5 métodos de diagnóstico por imagem utilizados na identificação de lesões periapicais, de diferentes diâmetros, simuladas mecanicamente.
MétodosA amostra do presente estudo consistiu de 12 mandíbulas humanas secas. Radiografias panorâmicas digitais, radiografias periapicais convencionais e digitais (dispositivo de carga acoplada e placa de fósforo fotoestimulável), e tomografia computadorizada de feixe cónico de alta resolução (TCFC) foram realizadas previamente para excluir regiões com lesões periapicais ou condições semelhantes. Em seguida, lesões periapicais foram produzidas progressivamente por meio de brocas de diferentes diâmetros, criando lesões periapicais de diferentes tamanhos. Os diferentes métodos de diagnóstico por imagem foram executados após a produção de cada lesão. Os dados foram avaliados por meio dos testes Kappa, curva ROC e Q de Cochran, com nível de significância de 0,05.
ResultadosAs imagens de radiografias panorâmica digital eperiapical convencional apresentaram os piores resultados (0,65 e 0,55, respectivamente) e com diferença estatisticamente significante quando comparados ao grupo controle (p<0,05), em lesões artificialmente produzidas com a broca 6. Com relação à TCFC de alta resolução, os valores de área obtidos foram elevados em todas as lesões.
ConclusãoRadiografias panorâmicas digitais e periapicais convencionais não proporcionaram imagens satisfatórias para a identificação de lesões periapicais incipientes. A TCFC de alta resolução demonstrou elevada acurácia no diagnóstico de lesões periapicais em todas as regiões avaliadas, e provou ser o método mais confiável para a identificação de lesões periapicais iniciais (1,8mm).
The interpretation of radiographic images continues to be the primary tool for the diagnosis of bone lesions in the maxilla-mandibular complex. Diagnosis of periapical pathology has always been an issue of interest to doctors. Identification of evidence of periapical pathology in nonvital teeth is central to treatment planning, and the disease is diagnosed when periapical radiolucency is present.1,2 Panoramic radiography (PR) is the image diagnosis method used for tracking oral and maxillofacial diseases such as dental caries, periodontitis, tumorous lesions, degenerative bone changes in temporomandibular joints and inflammatory diseases (e.g., periapical diseases).3 Conventional periapical radiographs (CPR) are the most commonly used method for the evaluation of the periapical region, but superposition of bone structures can impair visualization of periapical radiolucent images, primarily with initial lesions. Anatomical features adjacent to the area of interest may result in poor contrast and therefore increased difficulty in assessing periapical tissues.4
Conventional radiographs have been replaced by digital systems. The digital radiography have the advantages of immediately generating images, eliminating chemical processing, and allowing images to be manipulated, stored and sent to other practitioners, thus increasing the ability to visualize the images and determine a diagnosis.5 However, the main advantage for the patient is the radiation dose reduction in digital systems. About radiation exposure and based on ALARA principle (the desired amount of information must be obtained with the smallest possible amount of radiation), digital systems showed a dose reduction from 30% to 70% compared to E-Film speed.6
Tachibana and Matsumoto, in 1990, were pioneers in research on the use of computed tomography in endodontics.7 However, this method also has disadvantages, such as high radiation doses and high examination costs.2,8,9 Due to these limitations, cone beam computed tomography (CBCT) was developed for the dentistry market to provide visualization of bone and alveolar structures in three dimensions using lower radiation dose.10 In general, CBCT can be categorized into large, medium, and limited volume units based on the size of their field of view (FOV). The size of the FOV describes the scan volume of the CBCT machine and is dependent on the detector size and shape, beam projection geometry and the ability to collimate the beam. Beam collimation limits the radiation exposure to the region of interest and ensures that an optimal FOV can be selected based on disease presentation. The radiation dose applied in CBCT is lower, mainly when the exam is performed with a reduced field of view.10 However, CBCT still has exposure radiation larger than periapical radiography. Two recommendations are given10: (1) Intraoral radiographs should be considered the imaging modality of choice in the evaluation of the endodontic of the patient, and (2) limited FOV in CBCT should be considered the imaging modality of choice for diagnosis in patients who present with contradictory or nonspecific clinical signs and symptoms associated with untreated or previously endodontically treated teeth. Radiation exposure to patients should be kept as low as reasonably practicable (ALARA principle).10 Nevertheless, the use of CBCT imaging is indicated only in cases which complex anatomy and/or morphology is suspected. It is worth remembering that CBCT imaging still uses ionizing radiation.11,12 To improve the visualization of endodontic diseases, such as periapical diseases, the use of a limited FOV and a small isotropic voxel (high-resolution) is recommended.10
The aims of the present study was to assess and compare digital panoramic radiography, conventional periapical radiography, digital periapical radiography (charged couple device – CCD, and photo-stimulable phosphor plate – PSP) and high-resolution cone beam computed tomography for the identification of periapical diseases, which were simulated in several stages and/or sizes.
Materials and methodsBefore commencement of the study, appropriate ethics approval was obtained from the Pontificial Catholic University of Minas Gerais (PUC-Minas) Human Research Ethics Committee (Ethics Approval Number: CAAE 07790512.9.0000.5137).
The sample of the present study consisted of 12 dried human mandibles belonging to the Dentomaxillofacial Radiology laboratory from School of Dentistry of the Pontifical Catholic University of Minas Gerais. Digital PR, conventional and digital periapical radiography (CCD and PSP), and high-resolution CBCT were previously performed to exclude regions presenting periapical diseases or similar conditions (exclusion criteria), which then formed the control group (10 anterior teeth and 20 posterior teeth). The alveoli of dried human mandibles used in this study were considered the golden standard. Following this stage, the experimental group was formed by 30 roots/alveoli (10 anterior teeth and 20 posterior teeth) selected from dried human mandibles. The mandibles were immersed in a recipient solution containing water and liquid detergent for 90min to facilitate the extraction of teeth.8 The teeth were then removed, and the integrity of the alveolar bone was assessed.
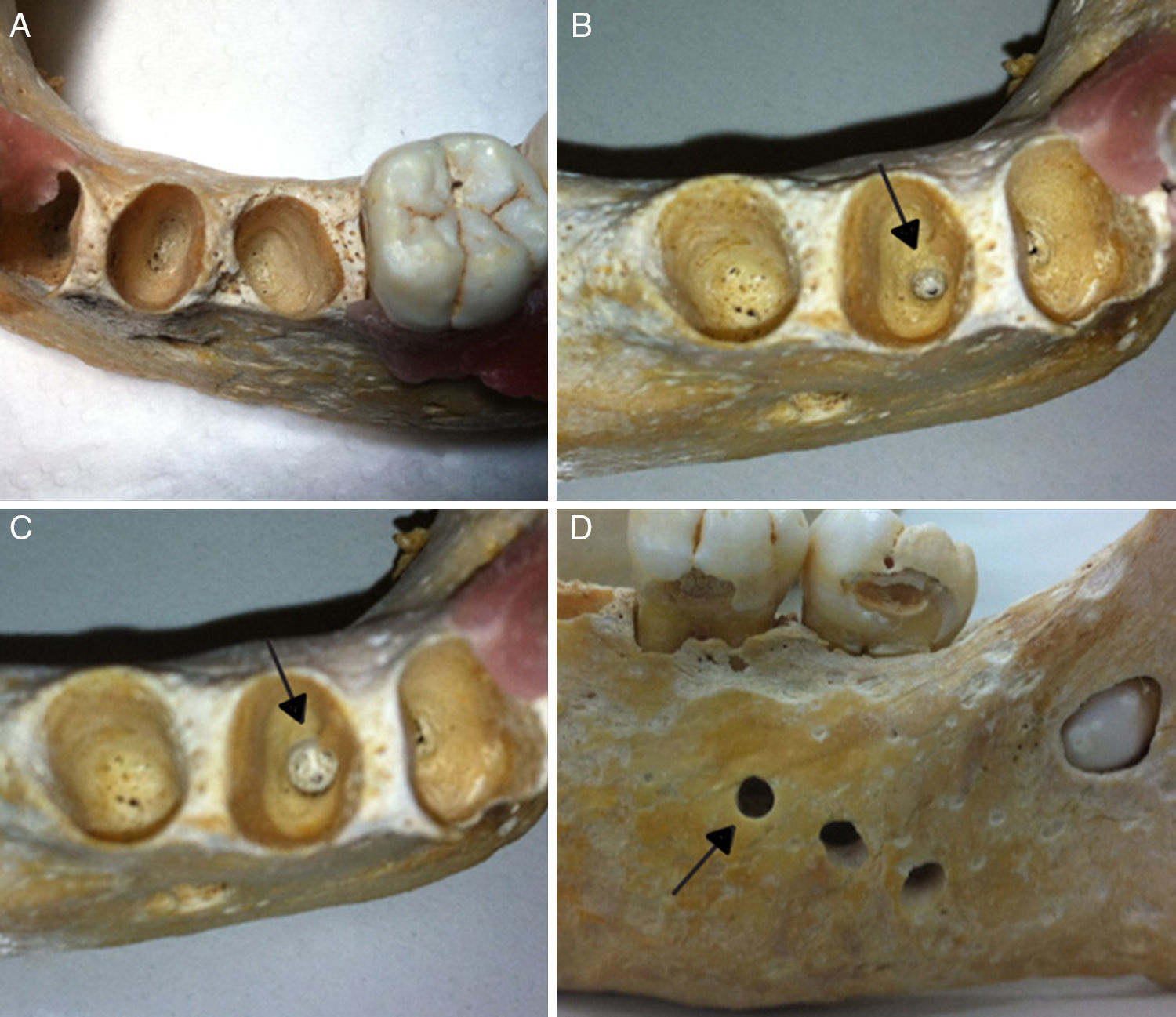
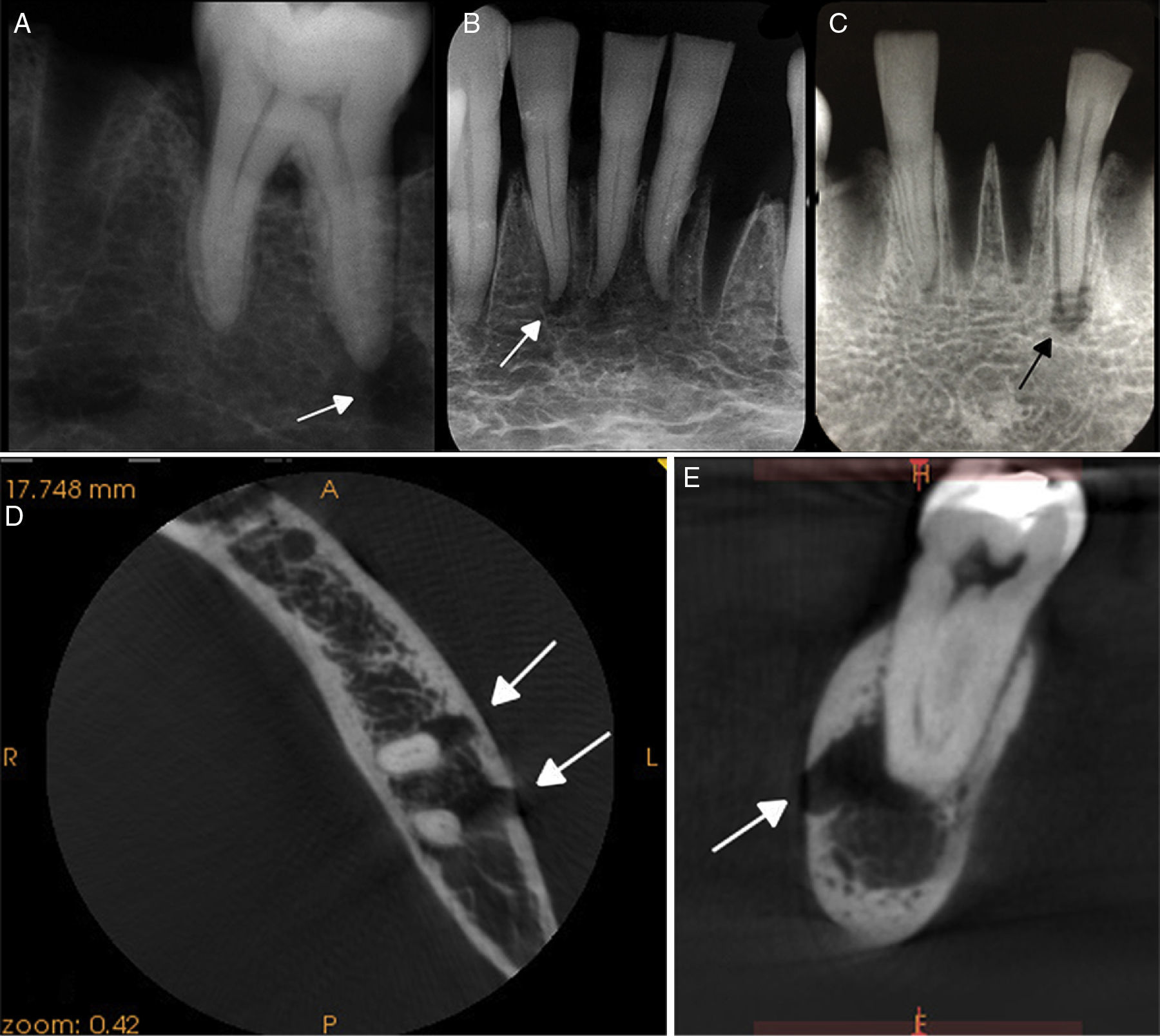
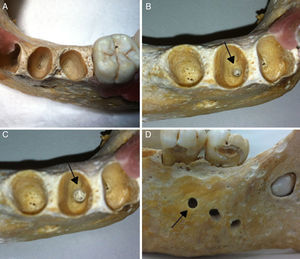
Periapical diseases of different sizes were artificially produced in each alveolus by means of non-water low-speed handpiece INTRAmatic 10 ABN (Kavo do Brasil, Santa Catarina, Brazil) and spherical carbide drills (Dentsply-Maillefer, Inc., Ballaigues, Switzerland) numbers 6 (1.8mm diameter) and 10 (2.7mm diameters). The penetration limit was determined by the diameter of the drill head and the size in millimeters was confirmed by CBCT. Lastly, was produced disruption of the buccal cortical bone, resulting in four different phases (Figure 1). After each preparation, the mandibles were submitted to radiographic and tomographic examinations.
To obtain the periapical radiographs, an intraoral X-ray system (Kodak 2200, Carestream Health, Inc., New York, USA) was used at 60kV and 7mA. According to the conventional method, size #2 radiographic E/F-speed film (Kodak Insight, Carestream Health, Inc.) were used with exposure times of 0.3 and 0.36s in the anterior and posterior teeth, respectively. With regard to the digital method, a CCD sensor (Kodak RVG 5100, Carestream Health, Inc.) and a PSP digital system (ScanX-Duo, Air Techniques, Inc., New York, USA) were used to allow a spatial resolution of 14lp/mm and 22lp/mm, respectively. The exposure times were set at 0.15 and 0.18s for anterior and posterior teeth, respectively. The parallelism technique was performed. The samples were mounted to align with a Rinn plastic ring paralleling device (Rinn Manufacturing Company, Inc., Illinois, USA) affixed to the acrylic block with cyanoacrylate adhesive.5 This acrylic block of 20mm in thickness was used to simulate the soft tissues.13,14 The mandibles were stabilized with the aid of a plastic box supported by a camera tripod, thus allowing a standard distance to be maintained between X-ray source and sample surface.
Regarding the panoramic images, was used a digital apparatus (Kodak 9000C 3D, Carestream Health, Inc.) operating at 60kV, 2mA and an exposure time of 14.1s. A plastic box with rods was used for the positioning of the mandibles and image acquisition, which allowed stability of the materials, standardization and the proper positioning within the focal trough. Next, the plastic box was filled with water (750ml) to promote attenuation of X-ray beams and to simulate the presence of soft tissue.15
The high-resolution CBCT (Kodak 9000C 3D, Carestream Health, Inc.) was performed with 60kV, 10mA and an exposure time of 10.8. Scanning was carried out with a FOV volume of 3.75cm×5.0cm and isotropic voxel size of 76μm. The mandibles were positioned using the same plastic box used for the acquisition of panoramic images.
Blinded analyses were performed. Two surgeon dentists, who were specialists in Oral Radiology, analyzed all the images separately and independently. The examiners evaluated each type of image on alternate days so that no comparison could be made between the techniques used. To assess the intra- and inter-rater reliability of the 2 evaluators, all cases were examined for a second time 50 days later.
For the interpretation of the CPR, a cold light negatoscope with a black cardboard mask in the same size of the images was used. The use of a magnifying glass was also allowed. The digital and tomographic images were visualized by means of specific software (Kodak Dental Imaging Software, Carestream Health, Inc.).
The presence of radiolucent images associated with the root apex, with discontinuity of the lamina dura, was diagnosed as periapical diseases (Figure 2).
Arrows indicating radiolucent images simulated with different drill sizes. Lesion associated with the root apex of the lower left first molar, using a CCD sensor (A), and of the lower incisors, using a PSP system (B) and CPR (C). Arrows indicating radiolucent images associated with the root apex and rupture of the buccal cortical bone, in the axial (D), and sagittal view of high-resolution CBCT (E).
Intra- and inter-rater reliabilities were assessed by using the Cohen Kappa test and the results interpreted using following definitions: 0.01, poor; 0.01–0.20, slight; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, substantial; 0.81–1.00, almost perfect.16 The area under the ROC curve was calculated by means of appropriate software (BioEstat 5.0; Belém, PA, Brazil). The values for true negative, true positive, false negative, false positive and accuracy were calculated. Cochran's Q test was performed at a significance level of 5% (α=0.05). A p value of less than 0.05 was considered to indicate statistical significance.
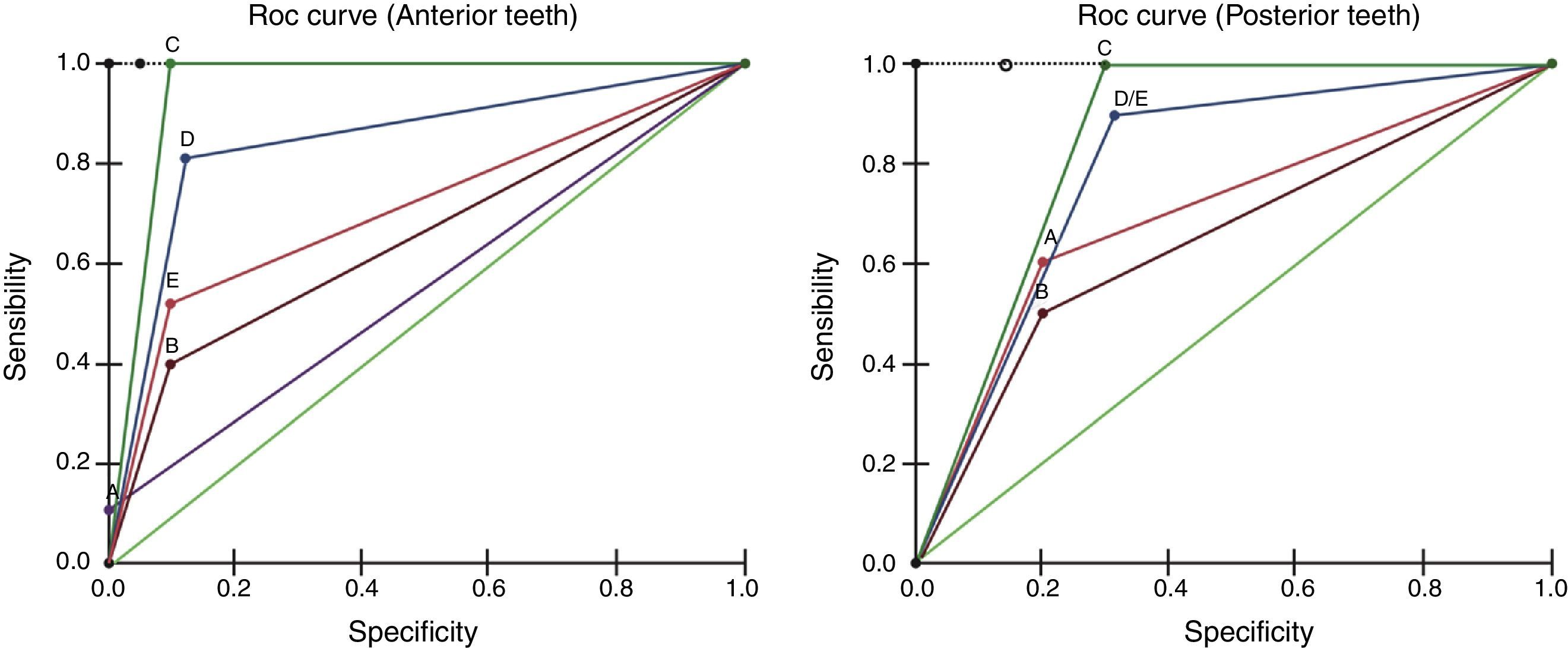
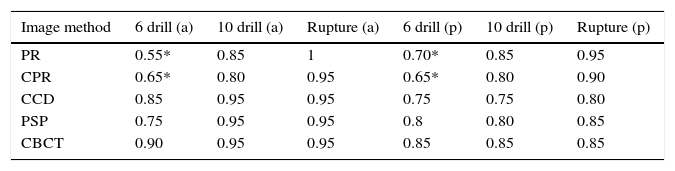
ResultsUsing the ROC analysis, it was observed that the images of anterior teeth obtained from digital PR and CPR presented greater area values (1.0 and 0.95, respectively), for rupture of the buccal cortical bone, and smaller area values (0.55 and 0.65, respectively), for lesions artificially produced with #6 drill. Digital PR yielded 100% true-positive results for rupture lesions, but a small area value of 0.55 was observed for lesions artificially produced with #6 drill, with low sensitivity and high specificity (high false negatives). On digital periapical radiography (CCD and PSP), the area values for lesions artificially produced with #10 drill and rupture of the buccal cortical bone were found to be equal (0.95), that is, with a high rate of true positives. With regard to high-resolution CBCT, the area values were found to be high for all lesion sizes (Table 1), demonstrating high accuracy.
Average area under receiver operating characteristic (ROC) curve for lesion sizes in anterior and posterior teeth according to the different image diagnosis method used.
| Image method | 6 drill (a) | 10 drill (a) | Rupture (a) | 6 drill (p) | 10 drill (p) | Rupture (p) |
|---|---|---|---|---|---|---|
| PR | 0.55* | 0.85 | 1 | 0.70* | 0.85 | 0.95 |
| CPR | 0.65* | 0.80 | 0.95 | 0.65* | 0.80 | 0.90 |
| CCD | 0.85 | 0.95 | 0.95 | 0.75 | 0.75 | 0.80 |
| PSP | 0.75 | 0.95 | 0.95 | 0.8 | 0.80 | 0.85 |
| CBCT | 0.90 | 0.95 | 0.95 | 0.85 | 0.85 | 0.85 |
Anterior teeth (a); posterior teeth (p). Areas followed by (*) show statistically significant differences compared to controls (Cochran's Q at a significance level of 5%).
In the posterior teeth, small area values were observed on digital PR and CPR (0.70 and 0.65, respectively) in those cases of lesions artificially produced with #6 drill. However, it was observed that the value of the area became greater as the size of the lesion increased. High-resolution CBCT had the same value (0.85) for all lesion sizes (Table 1).
With regard to the dental regions studied, the images obtained with CPR and digital PR showed statistically significant differences compared to the controls (p<0.05) for lesions artificially produced with the #6 drill.
Because the ROC curve graphs regarding the different lesion sizes showed the worst and significant results for lesions artificially produced with #6 drill, the different image diagnosis methods were compared to each other only for these cases (Figure 3). ROC analysis of high-resolution CBCT showed a greater number of true-positive results in both anterior and posterior teeth. By comparing the images from CPR and digital (CCD and PSP) intra-oral radiographs, it was found that digital systems presented greater areas during evaluation. It was also observed that evaluation of digital PR yielded a curve that skewed excessively toward the left, but with low values (high false negatives); the curve was similar to that for CPR.
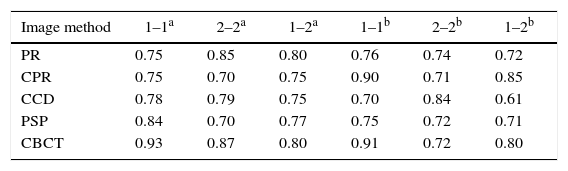
The Cohen Kappa was used to assess intra- and inter-rate reliabilities for lesions artificially produced with a #6 drill. The intra-rater reliability was found to be substantial (0.61–0.80) with the majority of image methods. The almost perfect reliability (0.81–1.00) was also found with digital PR, PSP, and high-resolution CBCT for anterior teeth, as well as with CPR, CCD, and high-resolution CBCT for posterior teeth. Inter-rater reliability was found to be substantial (0.61–0.80) with the majority of the imaging methods, except for the CPR of posterior teeth, which presented almost perfect reliability (Table 2).
Intra- (1–1) and (2–2) and inter-rater (1–2) reliabilities (weighted Kappa coefficient) of each image diagnosis method for lesions artificially produced with #6 drill in anterior and posterior teeth.
In the present study, CBCT always produced high values for accuracy. The greatest difference compared to the other methods was with regard to the lesions artificially produced with #6 drill (1.8mm), a finding similar to that reported by other authors.13,17,18
There are some studies on the diagnosis of periapical diseases using different diagnostic imaging methods, but few authors emphasize the accuracy of limited-volume and high-resolution CBCT in the identification of incipient periapical diseases when compared to other methods.19
The use of a device with a reduced FOV and small voxel size (high-resolution) provides better image resolution for the visualization of changes in the periodontal ligament space, which measures approximately 200μm, compared to other systems with larger voxel sizes and FOVs.10 A reduction in image matrix size is desirable to increase spatial resolution and therefore provide greater image detail. It has been claimed that large-volume CBCT produces grainier images compared with small-volume CBCT.20 In fact, an isotropic voxel size of 76μm provides spatial resolution of 6.5lp/mm, which is inferior to that of conventional film (approximately 20lp/mm) and digital systems (8–20lp/mm). However, the ability of this technology to demonstrate geometrically precise 3D images and to eliminate the superposition of anatomical structures enables accurate evaluation of important characteristics in endodontic diagnosis.10,21,22 One should also consider the lowest radiation dose produced when the FOV is reduced, because beam collimation limits the radiation to the region of interest.10,23,24 Smaller FOVs resulted in lower effective doses, suggesting that limited-volume CBCT should be used for dental images and that a larger field of view should be restricted to cases in which a wider view is required.25 Endodontic cases should be judged individually, and patients should always be exposed to the least amount of radiation possible to gain the most useful information for a proper diagnosis.11
Some authors compared changes in the sizes of periapical diseases after root canal treatment as revealed by periapical radiography and CBCT. Such authors concluded that the absence of a lesion or reduction in the size of a lesion after root canal treatment determined with CBCT and periapical radiography data were different. Assessment of the outcome of root canal treatments determined with periapical radiography could be inaccurate.26 As in our study, this finding demonstrates the importance of the ability of high-resolution CBCT to eliminate the superposition of anatomical structures, especially for visualization of small lesions. Bender and Seltzer4 demonstrated that periapical diseases could be radiographically viewed only when the lesions reached the buccal cortical bone, the lingual cortical bone or both. In the present study, the lower sensitivity (0.2) was verified on conventional periapical images of lesions produced with #6 drill in the posterior teeth, the same region studied by Bender and Seltzer. This finding can be explained by the buccal cortical bone in this region being thicker. However, the conventional periapical images of the lesions produced with #10 drill (2.7mm) do not show statistically significant differences compared to the controls and are capable of being diagnosed, contradicting the report of Bender and Seltzer. Though, in the present study the radiographic images were obtained with lower kV and mA, thereby providing higher contrast and lower density of the radiographic image, allowing great detail in periapical image. However, Bender and Seltzer do not describe details of the radiographic films (e.g., spatial resolution) that were used in their study in 1961. So, after the evolution of radiographic films in these 45 years, probably the films that were used in the present study have higher spatial resolution. Regardless of the region, the conventional intra-oral techniques were found to be more accurate for the diagnosis of greater lesion sizes compared to smaller sizes, primarily when cortical bone was involved.5,21,27,28
A previous study found substantial disagreement between CPR and CBCT assessments of the number of canals and the number and size of lesions amongst molar teeth. For all molars evaluated, the mean number of lesions found with periapical films was 0.95 versus 1.55 with CBCT. The value represents a 63% increase in the amount of periapical diseases detected using CBCT. Those authors demonstrated that CBCT is more sensitive at detecting periapical diseases than intraoral radiographs.29 The results of the current study indicated similar sensitivity. CBCT allows to clinician several views, reconstructed slices of data without the overlying cortical plate, which may otherwise hide what is actually occurring within the cancellous bone. With CBCT, the examiner usually specifies the orientation of the reconstructed slices resulting in views that are parallel and perpendicular to the long axis of the root under investigation showing high accuracy in the diagnosis of periapical diseases compared bidimensional images.
In the present study, only lesions produced with #6 drill resulted in images significantly different from the controls (p<0.05). Such lesions were not detected by means CPR and digital PR in anterior and posterior regions. Other authors followed up the evolution of periapical diseases, induced by pulp exposure in dog teeth, using CPR and histological analysis, and they concluded that radiographic examinations were not capable of diagnosing initial-stage lesions.27 Unlike the present study and according to some authors, the PSP system produced images with significantly greater quality compared to those from CCD sensors.30 However, their study involved patients, and there was difficulty in proper positioning of the CCD sensors, which might have contributed to the worse results.
The digital systems used were of high resolution, with the CCD sensor having 14lp/mm and the PSP system having 22lp/mm, thus enabling them to distinguish details accurately but without eliminating the superposition of bone structures. Some authors have found better results with the CPR relative to the PSP system regarding the diagnosis of small periapical diseases, although the digital systems had spatial resolution of 6lp/mm. This resolution provides less detailed images than the digital system used in the present study, and in addition, their examiners had no previous experience with digital radiographs,1,31 thus differing from our work, in which the examiners had knowledge of several digital image manipulation tools. One should also consider the shorter exposure time with the digital systems than conventional periapical technique, that is, less radiation is emitted to the patient.
In the present study, digital PR had the smallest area (0.55) and consequently yielded the least accurate diagnosis of lesions produced with #6 drill in anterior teeth, even with the availability of manipulation image tools. Another study also found the same negative result for incisors, but this study involved patients instead of dried mandibles.32 Therefore, in the present research, the poor sharpness of the images of anterior teeth might have occurred due to inclination of the osseous tables within the focal trough, rather than to superposition with the cervical spine. In contrast, lesions produced in posterior teeth using #6 drill showed a greater area value (0.7) compared to anterior teeth, likely due to the better framing of the posterior region within the focal trough.33 Nevertheless, digital PR also showed statistically significant differences in the region of the posterior teeth compared to the controls. Panoramic radiographs of lesions produced with #10 drill and with rupture of the buccal cortical bone were shown to be reliable in the diagnosis of periapical diseases.
The majority of the results obtained from Cohen Kappa demonstrated substantial intra- and inter-rater reliabilities, thus demonstrating that all the image diagnosis methods are reproducible.
ConclusionsBased on the data obtained, the present study concluded that high-resolution CBCT showed high accuracy in the diagnosis of periapical diseases in both regions evaluated, and proved to be the most reliable method for the identification of initial periapical diseases (1.8mm). Digital periapical radiography systems (CCD and PSP) demonstrated lower accuracy for smaller lesions (1.8mm) compared with high-resolution CBCT. However, both periapical digital methods were capable to diagnose periapical diseases. The CPR and digital PR did not provide satisfactory images for the identification of incipient periapical diseases (1.8mm).
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank Kyria Spyrides, Alexandre Marques, German Villoria and Julia Travassos for fruitful discussions in the preparation of this study.