Nasopalatine duct cyst also known as nasopalatine cyst is a developmental, epithelial, non-neoplastic cyst that is considered to be the most common non-odontogenic cyst in the maxillofacial region. It is unique in that it develops in only a single location – the midline anterior maxilla. Nasopalatine cysts are usually asymptomatic and are often discovered incidentally during routine radiological examination. In this article the authors present a case of a nasopalatine cyst found in a 45-year-old male. The patient was referred, reporting a pressure over the anterior maxilla. There were no other symptoms and no recent history of pain. Clinical examination revealed a palatal expansion on the anterior hard palate. The lesion was surgically removed under general anaesthesia and diagnosis of a nasopalatine cyst was confirmed after histopathologic examination. The patient showed no clinical or radiographic signs of recurrence one year after surgical excision.
O quisto do ducto nasopalatino, também conhecido como quisto nasopalatino, é um quisto epitelial benigno de desenvolvimento, sendo o quisto não odontogénico mais frequente da cavidade oral. A sua localização é única – na linha média da zona anterior da maxila. Normalmente permanece assintomático apresentando-se, muitas vezes, como um achado radiográfico. Neste artigo, os autores apresentam o caso clinico de um quisto nasopalatino detetado num paciente com 45 anos de idade. O paciente foi-nos referenciado apresentando, como queixa principal, uma pressão localizada na zona anterior da maxila. Para além disso, não apresentava outros sintomas nem história recente de dor. Ao exame clínico foi detetado um abaulamento na zona anterior do palato duro. A lesão foi removida sob o efeito de anestesia geral e o diagnóstico de quisto nasopalatino foi confirmado após exame anatomopatológico. Um ano após a remoção cirúrgica da lesão o paciente não apresenta qualquer sinal de recidiva.
The nasopalatine duct cyst (NPDC) was first described by Meyer in 1914.1,2 NPDC, also named as incisive canal cyst, is a development lesion that arises from embryologic remnants present in the nasolapatine duct. It is one of the most common non-odontogenic cysts of the oral cavity, occurring in about 1% of the population.3–5 The majority of the cases occur between 4th and 6th decades of life. Men are affected more often than women – ratio 3:1.2,4–6 Although cysts may arise at any point along the nasopalatine duct, most origin in the lower part and some arise entirely within the soft tissue of the incisive papilla. These are often designated as cysts of the palatine papilla.7 It may be asymptomatic and discovered on routine radiographic examination, or may present as a slowly enlarging swelling in the anterior region of the midline of the palate. Pain may occur if the cyst becomes secondarily infected.8,9 Radiographically, NPDC usually present as a well-defined radiolucent area. They are usually symmetrical but some are displaced to one side. The cyst may be distinguished from a normal but widened canal and from periapical granuloma or radicular cyst associated to the roots of anterior teeth. A correct diagnosis can only be made after proper clinical, radiographic, and histopathologic examination.10 Malignant transformation is rare, and there are only a few reports in the literature.11 Enucleation is the preferred treatment with low recurrence rates.12
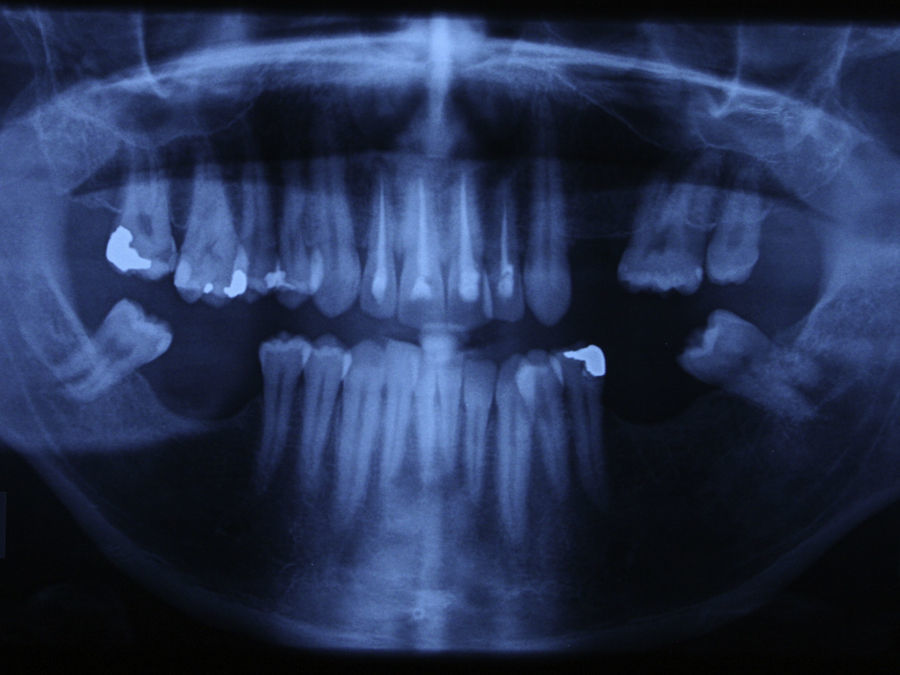
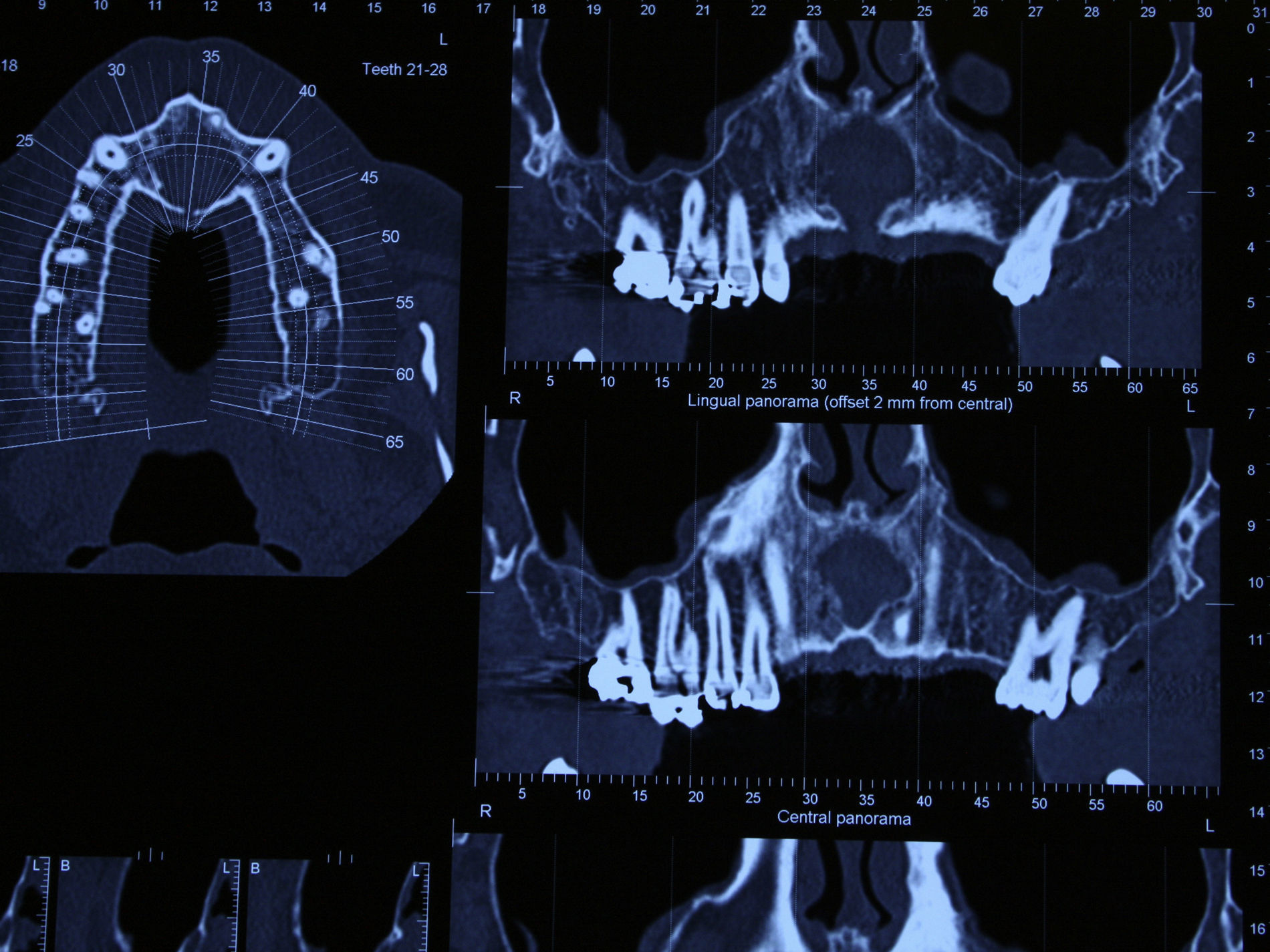
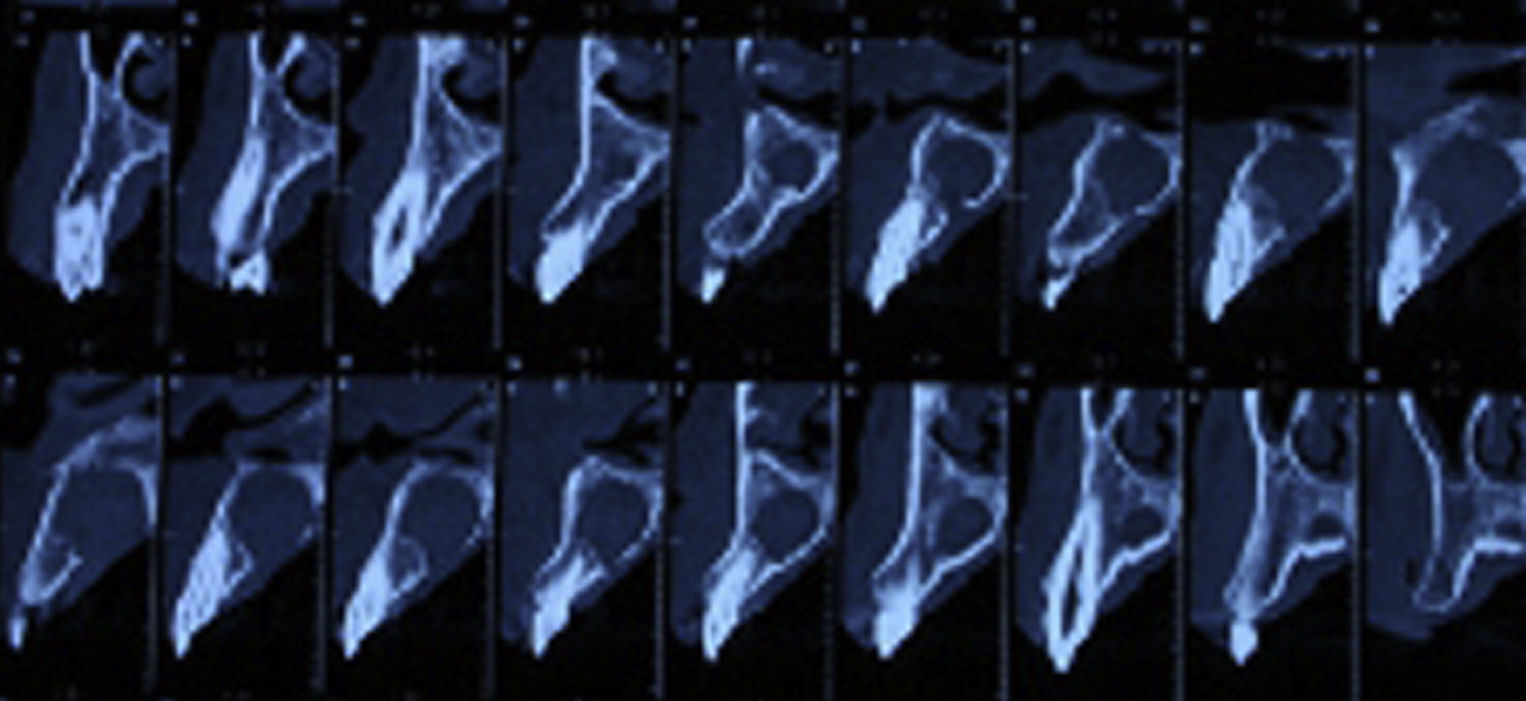
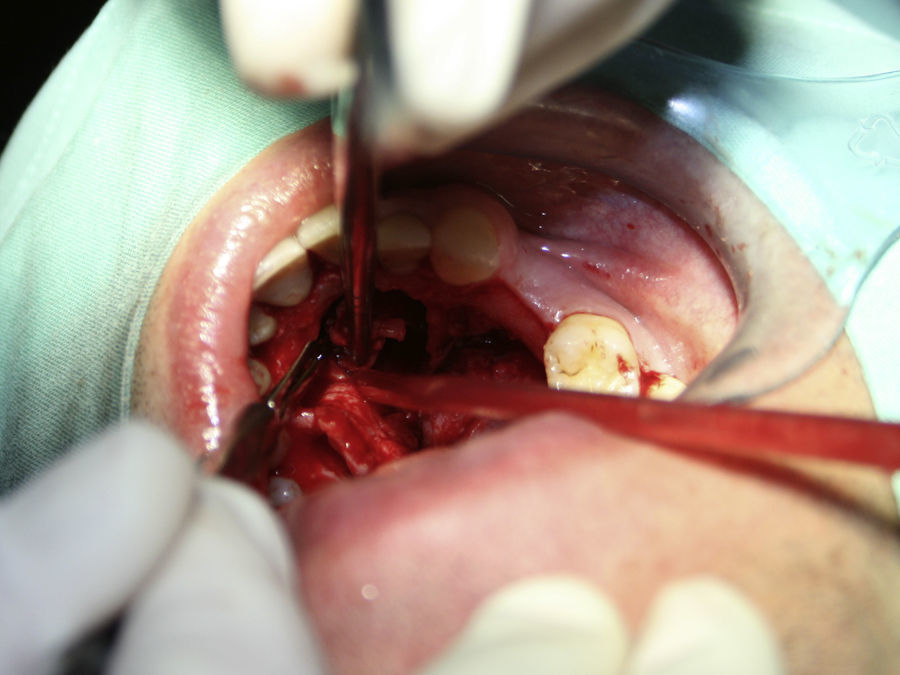
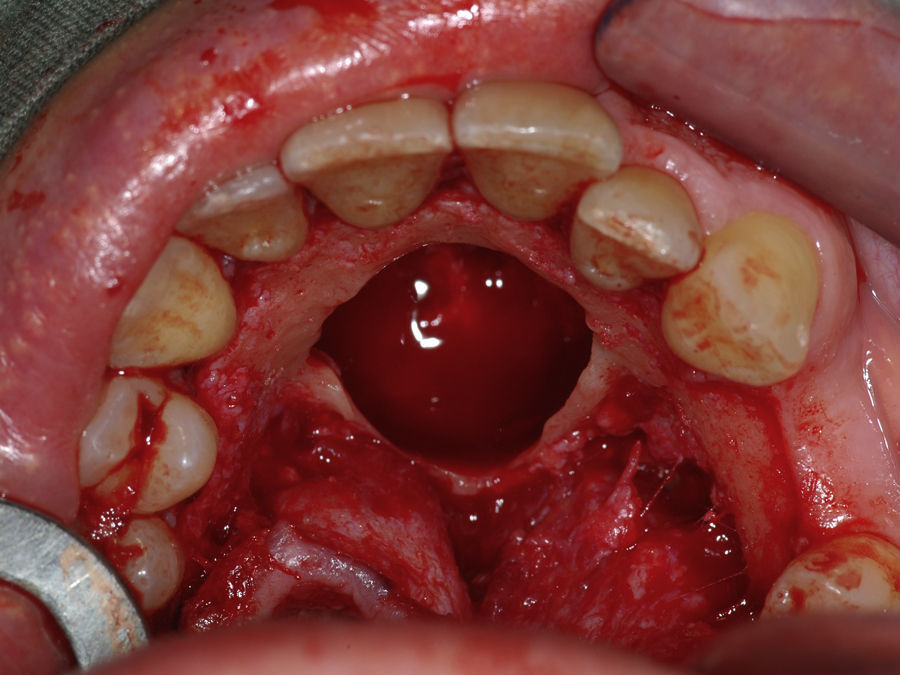
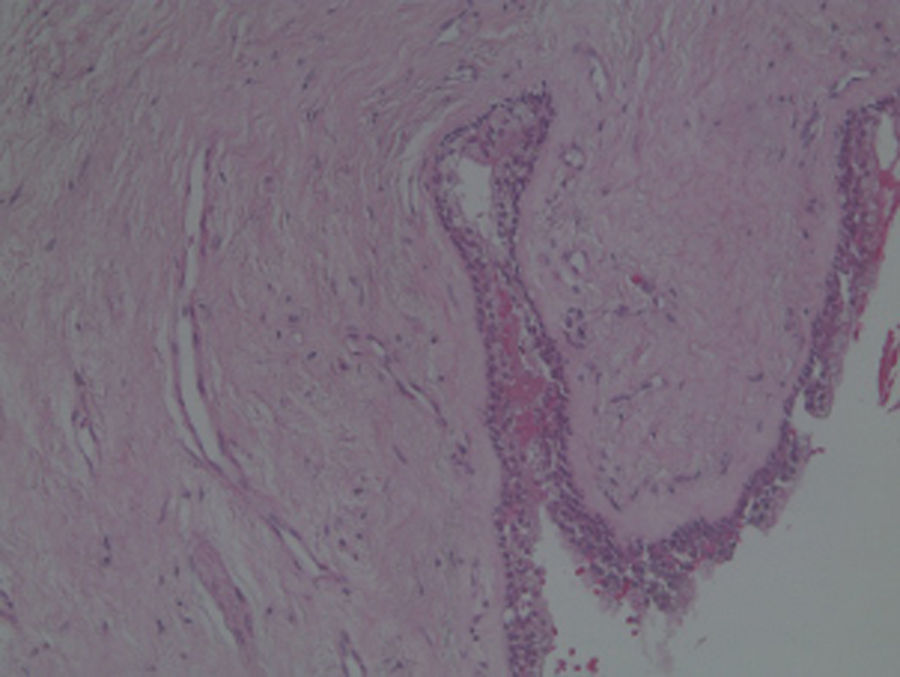
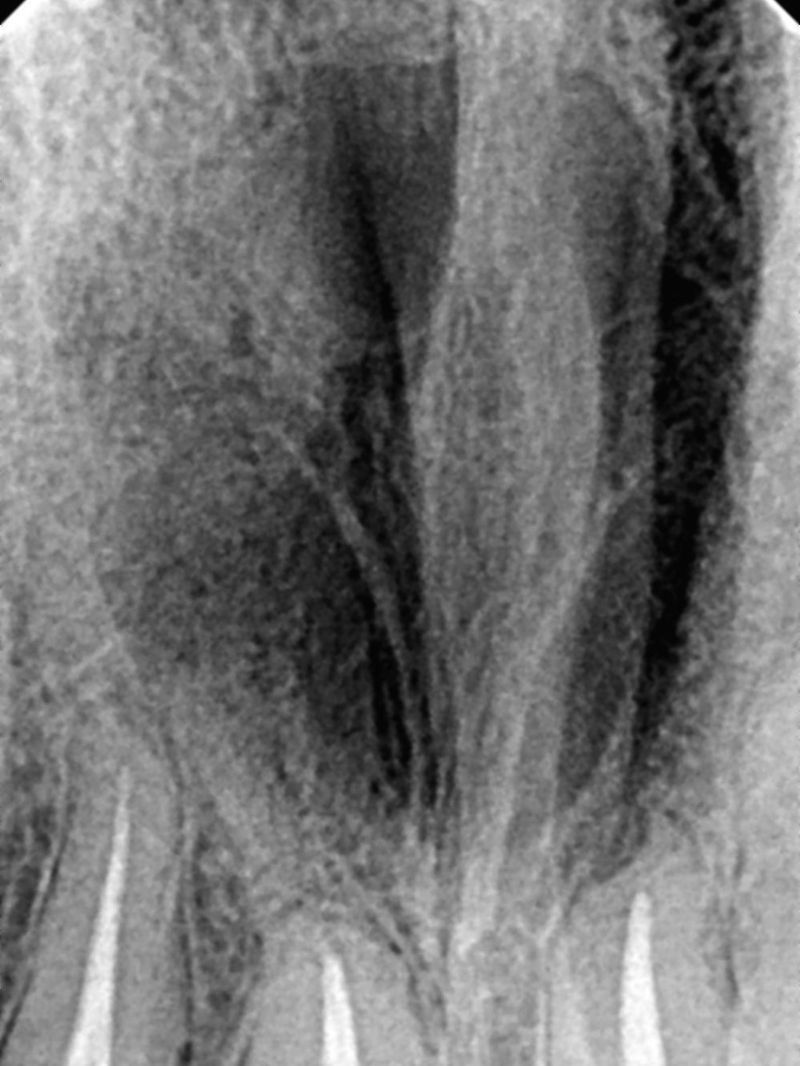
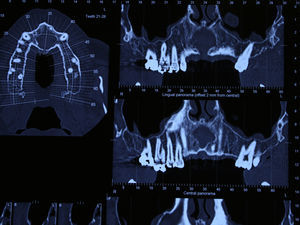
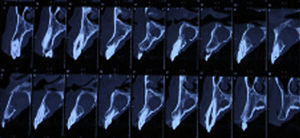
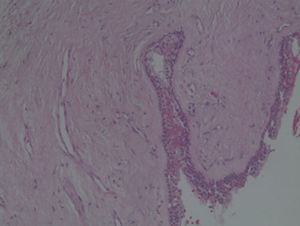
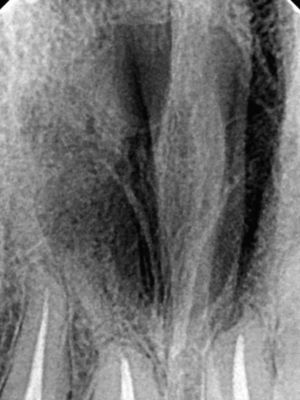
Case reportA case of a nasopalatine duct cyst in a 45-year-old male is presented (Fig. 1). The patient was referred, reporting a pressure over the anterior maxilla. There were no other symptoms and no recent history of pain. Clinical examination revealed a palatal expansion on the anterior hard palate (Fig. 2). There was no previous history of trauma. The patient was asked to take a computerized axial tomography which showed a well-defined radiolucency in the anterior maxilla in the region of incisive canal (Fig. 3). Loss of cortical bone was seen along the palatal aspect of the lesion in the sagittal sections (Fig. 4). Also resorption of nasal cavity floor bone could be seen in those sections. The cyst was enucleated under general anaesthesia. A palatal mucoperiosteal flap was raised and following bone removal, the friable, haemorrhagic cyst lining was curetted and sent for histological examination fixed in 10% neutral formalin (Figs. 5 and 6). After cyst removal it could be seen in the depth of surgical loca a small communication with the nasal cavity. Gross examination revealed a whitish, soft consistency fragment measuring 2.2cm×1.5cm×0.4cm (Fig. 7). Microscopic examination revealed fibrous wall lined by thin stratified squamous epithelium without inflammatory infiltrate and with some clear cells of ciliated appearance, which confirms the diagnosis of nasopalatine duct cyst (Fig. 8). The patient showed no clinical or radiographic signs of recurrence one year after surgical excision (Fig. 9).
DiscussionNPDC is the most common non-odontogenic cyst developing from the proliferation of embryological epithelial remnants of nasopalatine duct.4,5,13 Most studies show a higher incidence of NPDC among males than females4,5,12–15 which is in accordance with our case. A case of NPDC in a female patient was reported,16 but most cases reported in literature are in males.2,8,9,17–24 It may occur at any age but they are most common seen in the fourth to six decades of life.25,26 Our patient's age was in accordance with this. In a large study of 334 NPDCs, the overall mean age was 42 years and 6 months, with a male-to-female distribution of 1.2:1.5 A similar mean age result was found in a retrospective study.12 In another study of 31 patients the authors found a mean age at diagnosis of 37 years and 5 months, and a higher frequency in males than in females with a ratio of 3.4:1.14 Racial predilection is not clear due to lack of representative studies.4 However it has been suggested that there is a predisposition in young African Caribbeans, where NPDC appears to be more clinically aggressive with larger and symptomatic lesions than in other ethnic groups.27 In spite of being a developmental cyst, it is rarely seen in the first decade of life3. Very few cases have been reported to occur in children.2,19,23,27,28
Nasopalatine cysts are believed to develop from epithelial remnants of paired embryonic nasopalatine ducts within the incisive canal.26 The stimulus for cyst formation from the epithelial remnants of the nasopalatine canal is uncertain, although trauma and bacterial infection are thought to play a role.6,13,25
Most of these cysts are asymptomatic or cause such minor symptoms being tolerated for very long periods. Nearly 40% of the cases are totally asymptomatic and found only during routine clinical examination.15,17 In another study the authors reported that 87% of the cases were asymptomatic.14 Our patient referred few symptoms despite the size of the lesion. If this lesion was left untreated for a long time it could have an abnormal growth.9,11,18,21,29–31 The cyst may produce bulging of the floor of the nose or even a communication with the nasal cavity, as happened in our case. Usually patients complain of a small asymptomatic swelling just posterior to palatine papilla.16 In rare cases, the swelling is associated with a burning sensation.31 Pain is not a frequent complaint but it can be due to pressure on the nasopalatine nerves or if the cyst becomes secondarily infected.7 Various combinations of swelling, drainage and pain may occur. Drainage occurs in 25% of the cases5 and may be mucoid, in which case the patients describe a salty taste, or it may be purulent and the patients may complain of a foul taste.
In occlusal radiographs, they are seen as well defined round or oval radiolucencies in the midline, although some lesions can appear heart-shaped, because the nasal spine is superimposed on the radiolucent area.10,26
As the incisive canal and foramen may normally vary greatly in size, the clinician may have some difficulty in distinguishing between a large incisive foramen and a small asymptomatic incisive canal cyst on the basis of radiographic evidence alone. Some clinicians follow the thumb rule which says that radiolucencies of the incisive canal measuring less than 0.6cm in diameter should not be considered cystic in the absence of other symptoms.7,10 A radicular cyst or a granuloma associated with the central incisor should also be considered in differential diagnosis as these entities may be similar in appearance to an asymmetric NPDC. The presence or absence of the lamina dura and enlargement of the periodontal ligament space around the apex of the central incisor indicates an inflammatory lesion. NPDC and radicular cysts can also be differentiated by vitality tests once vitality of nearby teeth of a NPDC should not be affected. However, it is not uncommon to see evidence of endodontic therapy because the nasopalatine duct cyst was previously clinically misdiagnosed as a periapical cyst or granuloma.6,12 This is probably the reason why, in our case, the four maxillary incisive had yet root channel therapy when patient was referred to us. A residual cyst, a keratocyst and even central bone tumours can be confused with NPDC.18
NPDC may be delined by a variety of different types of epithelium that ranges from stratified squamous to pseudostratified columnar, or a combination of these.4,7,10 In this case we found both respiratory and squamous type of epithelial cells. Respiratory epithelium is seen only in 9.8% of the cases.14 The connective tissue wall contains small arteries and nerves, representing the nasopalatine neurovascular bundle. Collections of mucous glands and scattered chronic inflammatory cell infiltrate are frequently present.6,7,10
The treatment of choice is enucleation. Excision must be total to avoid relapse and postoperative long term follow-up is essential. Marsupialization may be recommended for a large cyst without bony architecture, which has the risk of developing a postsurgical permanent fistula.6,11,21,29,30,32,33 Recurrence rate is low5,33 and ranges from 0% to 11% depending on the authors.4,5,15,34 Paresthesia of anterior palate may occur in fewer than 10% of the cases, which can happen when branches of nasopalatine nerve are removed during surgery.12,27,33 Only after histological examination the definitive diagnosis can be established.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.