The purpose of this study was to evaluate the influence of different exposure times (24h, 7 days and 45 days) of zinc oxide eugenol cement (ZOE) on microtensile bond strength (μTBS) of etch-and-rinse and self-etch adhesives.
MethodsOcclusal enamel of 40 human molars was removed. Zinc oxide eugenol restoration was placed on the dentin surface and left for different times (24h, 7 days or 45 days). After ZOE removal or over fresh dentin (control) were restored using Adper Single Bond 2 (SB2) or Clearfil S3 Bond (CS3). After 24h, each tooth was longitudinally sectioned, to obtain bonded sticks that were tested under tension (0.5mm/min). Two-way ANOVA and Tukey's test (α=0.05) were used to compare μTBS.
ResultsA decrease in μTBS was observed for SB2 after 24h (46.8±3.4MPa) when compared to the control (60.4±5.2MPa, p<0.05). Similarly, a decrease was observed for CS3 after storage for 24h (20.4±2.2MPa) and 7 days (18.1±2.1MPa), when compared with a control group (39.1±4.2MPa, p<0.05). After 45 days, both adhesives SB2 and CS3 show the same μTBS compared to controls. Under all conditions, SB2 showed higher μTBS values than CS3 (p<0.001).
ConclusionThe results suggest that ZOE has negative effects on microtensile bond strength after 24h.
O presente estudo avaliou o efeito do tempo de permanência (24 horas, 7 ou 45 dias) de restaurações de provisórias de óxido de zinco e eugenol (OZE), na resistência de união de adesivos convencional e autocondicionante simplificados.
MétodosQuarenta (40) molares usados neste estudo tiveram o esmalte removido. Os espécimes do grupo controle não entraram em contato com restaurações de OZE. Nos demais grupos do OZE foram colocadas em contato com a dentina e assim permaneceram por diferentes períodos (24h, 7 ou 45 dias). Depois da remoção do OZE, foram usados os adesivos: Adper Single Bond 2 (SB2) ou Clearfil S3 Bond (CS3). Os espécimes foram cortados para obtencão de palitos para o teste de resistência de união. Os dados foram submetidos à ANOVA de 2 fatores e teste de Tukey (α=0,05).
ResultadosUma redução na resistência de união foi observada para o SB2 depois de 24 h (46,8±3,4 MPa) quando comparado com o grupo controle (60,4±5,2MPa, p < 0.05). Igualmente, uma redução nos valores de união foi encontrada para o adesivo CS3 quando OZE foi mantido por 24h (20,4±2,2MPa) ou 7 dias (18,1±2,1MPa) quando comparado com o grupo controle (39,1±4,2MPa, p < 0.05). Depois de 45 dias, os dois adesivos SB2 e CS3 apresentaram valores de união similares aos do grupo controle. Em todas as condições, o SB2 mostrou os maiores valores de união em compração com o CS3 (p < 0.001).
ConclusãoOs resultados sugerem que o OZE têm efeito negativo na resistência de união depois de 24h.
The use of provisional zinc oxide eugenol (ZOE) cement is common in prosthodontics, endodontics and restorative dentistry due to its desirable properties.1 In many cases, lack of time or the type of clinical treatment prevents ending treatment in a single clinical visit. Therefore, application of a temporary material is essential to seal the cavity.
On the other hand, cements containing eugenol may have potential negative effects on polymeric materials. For instance, eugenol may reduce color stability, hardness,2 degree of conversion,3 bond strength to dentin4–6 and adhesion of intraradicular post.7,8 Furthermore, it may inhibit polymerization of resin restorative materials9 as well as promote formation of gaps between dentin and restorative material.10 Lastly, eugenol has been shown to increase microleakage.11
The removal of provisional cement for placement of final restoration may leave remnants of the ZOE material on surface dentin.12–14 Thus, the presence of remnants makes it difficult for an adhesive system to penetrate into a substrate and polymerize.15,16
Contradictory literature reports exist on the influence of ZOE on bond strength of adhesive systems to dentin. While some studies have reported that its use should be avoided due to observed reduction of bond strength,3–5,10,17–19 other studies have observed no alteration with provisional restoration.20–23
A factor that may explain the conflicting results is the adhesive system applied in the various studies: in comparison with earlier generations of milder adhesive systems,20,23 the adhesive systems used currently all comprise a phosphoric acid etching step or a self-etching step.
Another contributing factor is the variable time interval during which ZOE cement remains in contact with the dentin surface prior to resin restoration. In several studies, the exposure time to ZOE has ranged from 24h,1,17,18 6 to 10 days19,20,22,23 or 4 weeks,14 making it difficult to make comparisons among studies and determine the actual real effect of ZOE on bond strength of dental adhesives.
The aim of the current study was to evaluate the influence of exposure time of ZOE on microtensile bond strength (μTBS) of two different simplified adhesive systems (etch-and-rinse and self-etching). So, the null hypothesis to be tested is that exposure time of ZOE does not influence the bond strength value.
Materials and methodsForty freshly extracted human third molars stored in 0.5% chloramine for up to 1 year were used in this study, which was approved by the Institutional Review Board of the local Dental School (23115003552/2010-59). A flat and superficial dentin surface was exposed on each tooth after wet grinding occlusal enamel using #180-grit SiC (silicon carbide) paper and wet polishing using #600-grit SiC paper for 60s to standardize the smear layer.
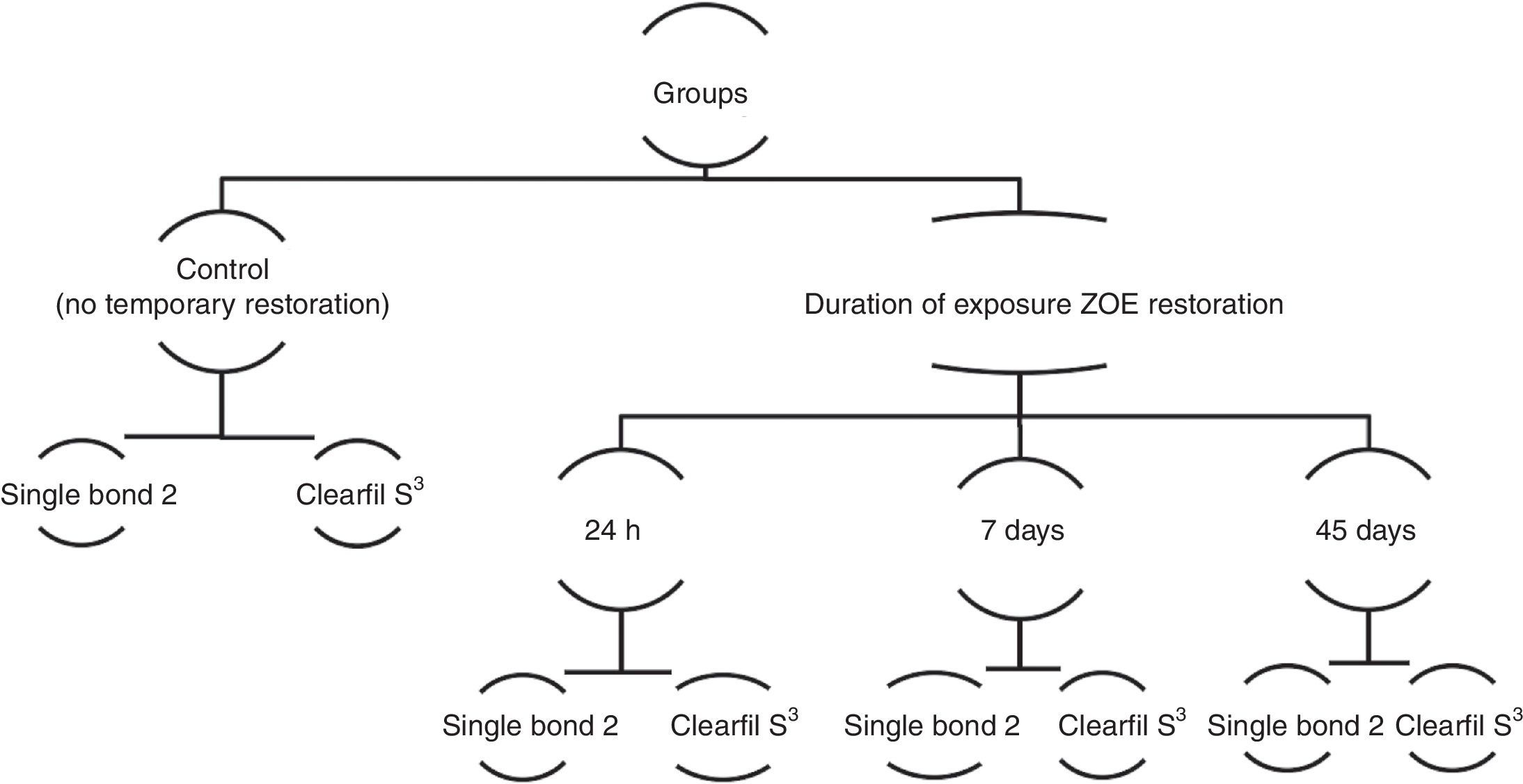
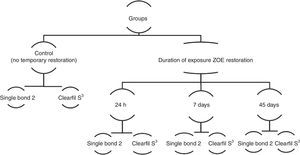
Specimens were divided into eight experimental conditions (n=5 in each group) based on length of contact time to ZOE restoration: Control group (without restoration) and test groups (with cement for 24h, 7 days or 45 days), which were further stratified based on adhesive system: Adper Single Bond 2 (3M/ESPE, St. Paul, MN, USA) or Clearfil S3 Bond (Kuraray Medical, Inc., Tokyo, Japan) (Fig. 1).
Before the filling was performed, eugenol-containing cement (IRM, Dentsply, Petrópolis, RJ, Brazil) was mixed according to the manufacturer's recommendations with a powder:liquid ratio of 6:1. The cement was placed on the dentin surface, except in the control group, allowing 1h for setting. Afterwards, test specimens were stored in distilled water at 37°C for the above mentioned times. The distilled water was changed every day. After the storage period, the ZOE was easily removed using a stainless steel spatula (to avoid scaling the dentin). All specimens were then cleaned with a pumice-water slurry using a slow speed handpiece for 60s, and rinsed with an air-water stream (60s).
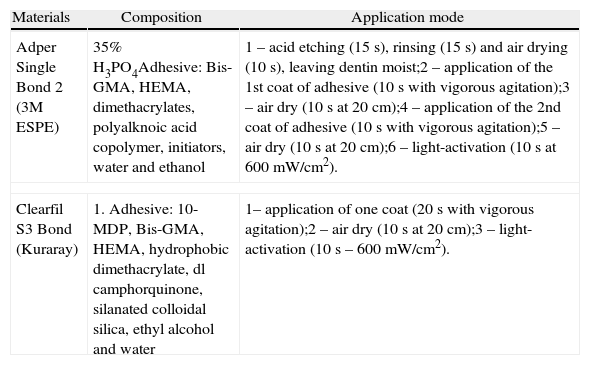
Adper Single Bond 2 bonding system, a two-step etch-and-rinse adhesive (SB2), or a Clearfil S3 Bond system, a one-step self-etch adhesive (CS3), was applied as described in Table 1.
Composition and application mode of adhesive systems.a
| Materials | Composition | Application mode |
| Adper Single Bond 2 (3M ESPE) | 35% H3PO4Adhesive: Bis-GMA, HEMA, dimethacrylates, polyalknoic acid copolymer, initiators, water and ethanol | 1 – acid etching (15s), rinsing (15s) and air drying (10s), leaving dentin moist;2 – application of the 1st coat of adhesive (10s with vigorous agitation);3 – air dry (10s at 20cm);4 – application of the 2nd coat of adhesive (10s with vigorous agitation);5 – air dry (10s at 20cm);6 – light-activation (10s at 600mW/cm2). |
| Clearfil S3 Bond (Kuraray) | 1. Adhesive: 10-MDP, Bis-GMA, HEMA, hydrophobic dimethacrylate, dl camphorquinone, silanated colloidal silica, ethyl alcohol and water | 1– application of one coat (20s with vigorous agitation);2 – air dry (10s at 20cm);3 – light-activation (10s – 600mW/cm2). |
Then, resin composite build-ups (Opallis, FGM, Joinville, SC, Brazil) were placed on the bonded surface (3 increments of 1.5mm each), which were individually activated with a halogen light set at 600mW/cm2 (VIP, Bisco, Schaumburg, IL, USA) for 40s each.
After each contact time interval, all specimens were longitudinally sectioned in both “x” and “y” directions across the bonded interface to obtain bonded sticks with a cross-sectional area of approximately 0.8mm2. Each one was then attached to a modified μTBS testing device, a Geraldelli's device (Odeme, Joaçaba, SC, Brazil), with cyanoacrylate resin (Super-Bonder, Loctite, Henkel Ltda., São Paulo, SP, Brazil) and subjected to a tensile force in a universal testing machine (Emic, São José dos Pinhais, PR, Brazil) at 0.5mm/min. The failure modes were evaluated at 40× magnification (HMV-2, Shimadzu, Tokyo, TY, Japan) and classified as cohesive resin (failure exclusively within composite, CR), cohesive dentin (failure exclusively within dentin, CD), or adhesive/mixed (failure at resin/dentin interface, A/M).
The experimental unit in this study was the specimen (tooth). The mean microtensile bond strength (μTBS) of all sticks from the same specimen was averaged for statistical purposes. The μTBS (MPa) means for every test group was expressed as the mean of the five specimen used per group.
Before subjecting the data to the appropriate statistical analysis, a Kolmogorov-Smirnov test was performed to assess whether the data followed a normal distribution. Barlett's test for equality of variances was performed to determine if the assumption of equal variances was valid. Afterwards, data were subjected to two-way analysis of variance (Adhesive vs. Time of contact), and a post hoc test (Tukey's test at α=0.05) was used for pair-wise comparisons.
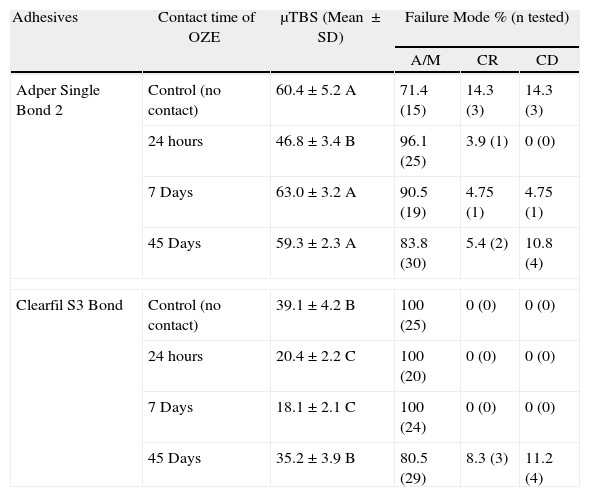
ResultsA summary of μTBS values is shown in Table 2. The cross-product Adhesive vs. Time of contact was statistically significant. For SB2, the 24h contact period showed a lower μTBS to dentin than the control (p=0.001). After 7 and 45 days, the results were similar to the control (p>0.05). For CS3, the 24h and 7 day contact periods showed lower BS to dentin than the control (p=0.001). After 45 days, the results were similar to the control (p>0.05). Under all conditions, SB2 showed higher BS values than CS3 (p<0.001). The distribution (%) of fracture patterns for each experimental condition is shown in Table 2. The failure mode showed a majority of adhesive/mixed fractures.
Mean and standard deviation (SD) of microtensile bond strength values (MPa) obtained for the different experimental groups and percentage distribution of failure mode (%) after microtensile bond strength testing (tested stick).
| Adhesives | Contact time of OZE | μTBS (Mean ±SD) | Failure Mode % (n tested) | ||
| A/M | CR | CD | |||
| Adper Single Bond 2 | Control (no contact) | 60.4±5.2 A | 71.4 (15) | 14.3 (3) | 14.3 (3) |
| 24 hours | 46.8±3.4 B | 96.1 (25) | 3.9 (1) | 0 (0) | |
| 7 Days | 63.0±3.2 A | 90.5 (19) | 4.75 (1) | 4.75 (1) | |
| 45 Days | 59.3±2.3 A | 83.8 (30) | 5.4 (2) | 10.8 (4) | |
| Clearfil S3 Bond | Control (no contact) | 39.1±4.2 B | 100 (25) | 0 (0) | 0 (0) |
| 24 hours | 20.4±2.2 C | 100 (20) | 0 (0) | 0 (0) | |
| 7 Days | 18.1±2.1 C | 100 (24) | 0 (0) | 0 (0) | |
| 45 Days | 35.2±3.9 B | 80.5 (29) | 8.3 (3) | 11.2 (4) | |
Groups with the same letter are not significantly different (Tukey's test, p>0.05).
Cohesive resin (failure exclusively within composite, CR), cohesive dentin (failure exclusively within dentin, CD), adhesive/mixed (failure at resin/dentin interface, A/M).
The microtensile bond strength results of the present study confirmed that the negative influence on bonding to dentin caused by ZOE restoration is dependent on the time of permanence and the null hypothesis was rejected.
A large number of studies have evaluated the interaction of eugenol and residues of eugenol-containing cement with adhesive systems.17–23 In the current study, the inhibition of polymerization caused by eugenol was evident when a reduction in bond strength of the two adhesives was observed after 24h. The high release of eugenol, which occurs in the first hours of contact with moisture may be responsible for the reduction μTBS.
The presence of water from both the oral medium and dentinal tubules may favor a reversible reaction capable of releasing eugenol from the zinc eugenolate matrix, which is incorporated into the subjacent dentin.16 These characteristics favor the accumulation of free non-reacted eugenol in the smear layer and dentinal tubules, compromising the bond strength of adhesive systems.15 Results of the current study are similar to those of Carvalho et al.,18 in which, irrespective of the type of adhesive (etch-and-rise or self-etch), bond strength was significantly affected after 24h of contact with ZOE.
After maintaining ZOE restoration for 7 days, the microtensile bonding strength values for the SB2 adhesive system were re-established. This was probably due to the effect of phosphoric acid etching used in this system. The SB2 adhesive requires dentin pre-treatment with acid, which removes the smear layer, exposing the collagen that will be infiltrated by the resin monomers to form the hybrid layer.
Koch et al.24 show that H3PO4 reduced the quantity of eugenol in dentin by a factor of 10 compared with no conditioning and that eugenol that remains on dentin surface can be subsequently washed off with water.
In self-etch systems, etching occurs simultaneously with resin monomer infiltration and, therefore, the dentin smear layer is not removed. Instead, it is incorporated into the hybrid layer.25 Since the demineralization depth of phosphoric acid etching may reach up to 9–10μm, it may potentially eliminate the smear layer as well as the contaminated subjacent dentin. This has been confirmed by various studies demonstrating that ZOE does not affect bond strength of etch-and-rise adhesives if tests are performed within 7 days after initial application of ZOE.6,20
In the current study, microtensile bond strength for CS3 adhesive remained low after the period of 24h and 7 days, and the ZOE restoration has an influence on the μTBS, when compared to the control group. However, several studies have not observed any effect of eugenol on bond strength of self-etch adhesives after one week.17,23 These studies used methods for ZOE removal, such as scalers or sandblasting, that may have contributed to the removal of a larger layer of contaminated dentin.17
Findings from the current study are consistent with previous studies reporting that self-etch systems do not remove the smear layer,25 but incorporate for the formation of a bond interface. For this reason, self-etch adhesive efficacy of bonding to the smear layer may be affected by the presence of contaminants, even 7 days after the presence of the ZOE restoration.
The presence of ZOE residue on the dentin surface reduces bond strength, as well as decreases surface energy of dentin, which may reduce the wetting capability of the adhesive system on dental surface.12,26 Despite removal of ZOE by mechanical cleaning and a visually clean macroscopic appearance, remnants can still be found on the surface. ZOE may act as a barrier, inhibiting interactions between acidic functional monomers and inorganic components of dentin.26 Analysis by atomic force microscopy (AFM) showed that a larger amount of granular particles were present when samples were treated with a self-etching primer compared to phosphoric acid.19 Even the presence of low concentrations of eugenol into smear layer may inhibit the polymerization reaction of resin materials.10 All of these conditions are potentially responsible for the lower bonding strength observed from the CS3 adhesive when ZOE remained on the dentin between 24h and 7 days. However, after 45 days, both the CS3 and SB2 adhesive showed no statistically significant differences compared to the control group.
The sensitivity of adhesive systems in the groups that were restored with temporary cement is evident when observing the fracture mode, where it is possible to observe that the SB2 shows large incidence of fracture adhesive/mixed (Table 2). However, CS3 did not show the same pattern.
The diffusion rate of eugenol is highest within the first 24h, but decreases rapidly afterwards.15 As previously mentioned, this may be due to the reduction in free eugenol being released after 45 days. Clinically, 7 days is a reasonable period for the replacement of temporary restorations when using etch-and-rise adhesives and 45 days for self-etch adhesives.
ConclusionsPretreatment of dentin with ZOE affects resin-dentin bond strength of the two adhesive systems evaluated, particularly that of the self-etch approach. When ZOE was applied, it was necessary to wait 7 days before performing restorations with an etch-and-rinse adhesive, and 45 days for restorations with a self-etch adhesive.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe author has no conflicts of interest to declare.
This study was supported by FAPEMA (01164/09 and 228/2011) and CNPq (237066/2012-2 and 310874/09-2).