This article presents the clinical case of 21 years old female patient reporting history of Arthrogryposis Multiplex Congenita (AMC). The extraoral examination disclosed clinical AMC pathognomonic signs. The intraoral examination revealed slight compression of the maxillary arch, conical upper lateral incisors, absence of 17 and 35, 53 persistence, upper cuspids inclusion and agenesis of third molars. Additionally, there was a severe generalized shortening of the tooth roots, with a general 1:1 root/crown proportion. The extraction of 23 was planned due to its maxillary position. Relatively to the 13, the orthodontical traction with a microimplant was the option. Treatment planning established orthodontics to restore esthetics and function followed by rehabilitation with implants. Finally, the esthetic composite restorations of 12 and 22 were programmed, given the limited prognosis presented by fixed prosthesis in the cases of root/crown low proportions.
Este artigo apresenta um caso clínico de uma paciente de 21 anos, do sexo feminino, que relatou história de Artrogripose Múltipla Congénita (AMC). O exame extraoral revelou sinais clínicos patognomónicos de AMC. O exame intraoral revelou compressão da arcada maxilar, incisivos laterais superiores conoides, ausência do 17 e do 35, persistência do 53, inclusão dos caninos superiores e agenesia dos terceiros molares. Adicionalmente, verificou-se um encurtamento radicular severo generalizado, com a maioria das proporções raís/coroa 1:1. Foi planeada a extracção do 23, dada a sua posição na maxila. Relativamente ao 13, a tração ortodôntica com um microimplante foi a opção eleita. Planeou-se o recurso à ortodontia para restabelecer estética e função, seguida de reabilitação com implantes. Finalmente, planearam-se restaurações estéticas a compósito nos dentes 12 e 22, dado o limitado prognóstico oferecido pela prótese fixa em casos de baixas proporções raíz/coroa.
Arthrogryposis Multiplex Congenita (AMC) is a rare congenital disorder,1 affecting 1 in 30002–4 to 1 in 12,0005 newborns. It involves the presence of multiple non-progressive,1,3 symmetric joint contractures,1,3,4 sometimes associated with muscle weakness and fibrosis.1
This disease can present an isolated form or it can also be associated with other congenital anomalies, as part of a syndrome, with or without central nervous system involvement.6
This condition's etiology is considered multifactorial and may be presented as a monogenic disease (autosomal recessive transmission, autosomal dominant or associated with the X chromosome), as a chromosomal disorder or as a congenital malformation (involving various organs).7 AMC may also be associated with environmental factors such as infections, drugs administration, trauma, chronic diseases, oligohydramnios or abnormal uterus structure (affecting the mother and the developing fetus).7 These factors described in the etiology of AMC are also common to approximately 7% of the congenital abnormalities in general.3
In the recognition of early clinical signs of AMC, in the last months of pregnancy, decreased fetal movement (fetal akinesia) is considered a common denominator to all AMC affected individuals, conditioning a variety of minor fetal deformities. It is important to notice the absence of movement, essential for joints and periarticular tissues development, leads to an increase of connective tissue around the immobilized joint with rippling of the skin covering the joint, muscle atrophy and changes in the joint surface depending on the position of the immobilization.3,8
The involvement of the temporomandibularjoint (TMJ) is a common AMC complication, conditioning the mandibular kinetics.2,9 Other common features include the presence of micrognathia,2,8 slightly shortened limbs, intrauterine growth restriction, pulmonary hypoplasia and short and/or immature bowel.8 Some cases of AMC were also found associated with the presence of upper lateral conoid incisors,10 hypodontia11 and delayed tooth eruption.2
This paper focused on the presentation of a clinical case of AMC, emphasizing oral and craniofacial abnormalities and proposing a treatment approach.
Case reportA female patient, 21 years old, attended a dental appointment to assess orthodontic treatment need, referring the closure of existing dental gaps in the upper anterior arch as a priority. During the anamnesis, the patient reported an AMC history, diagnosed since childhood.
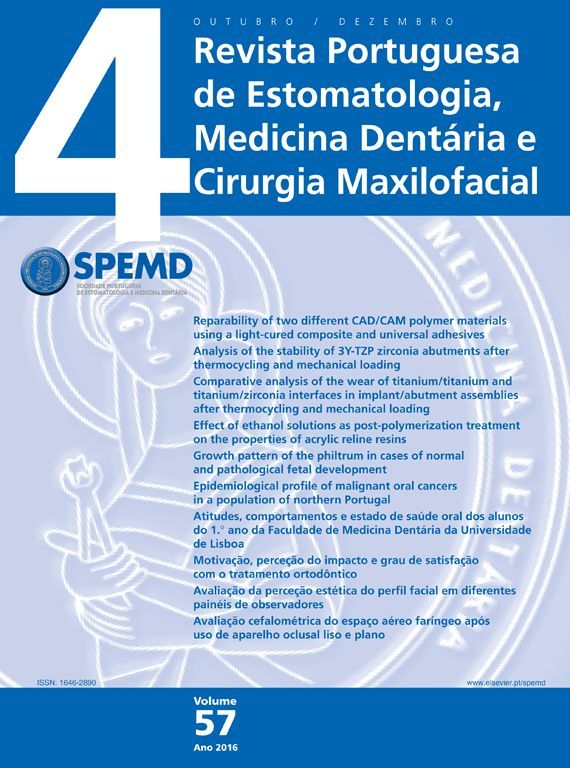
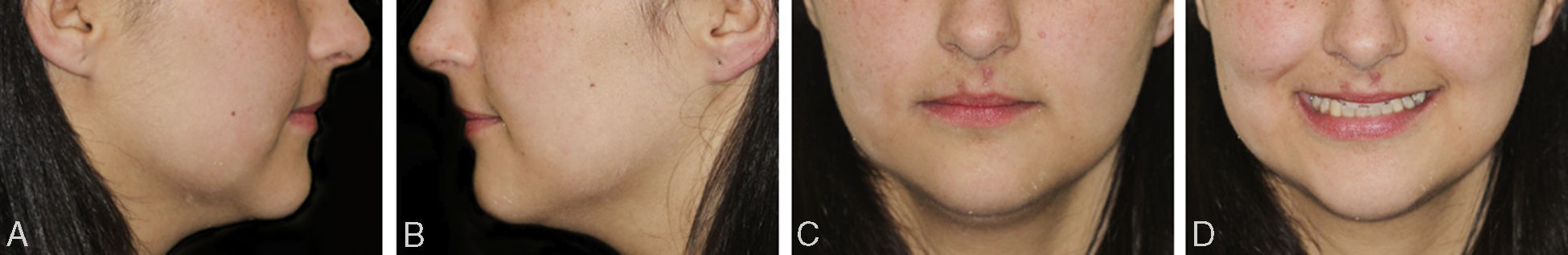
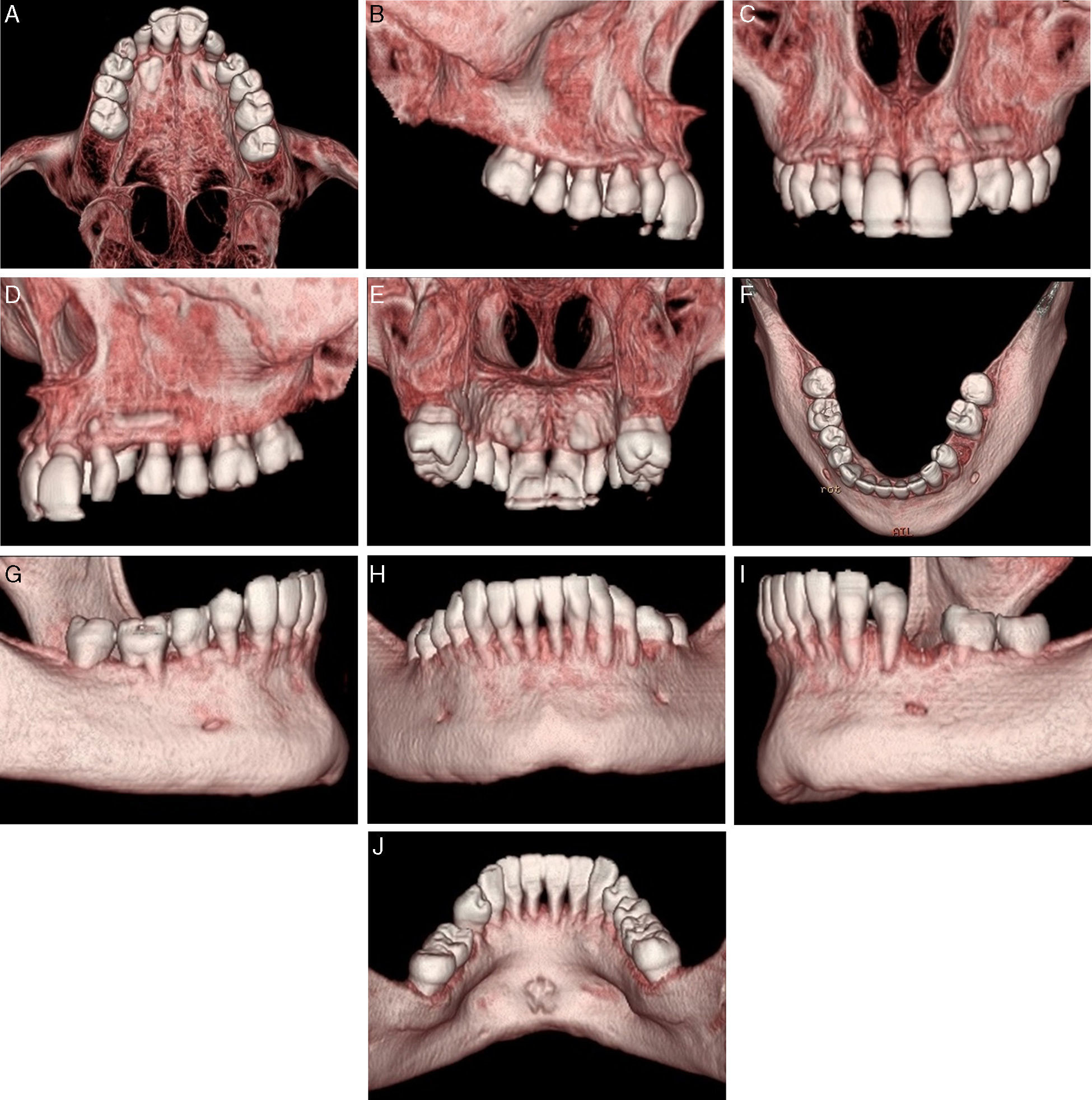
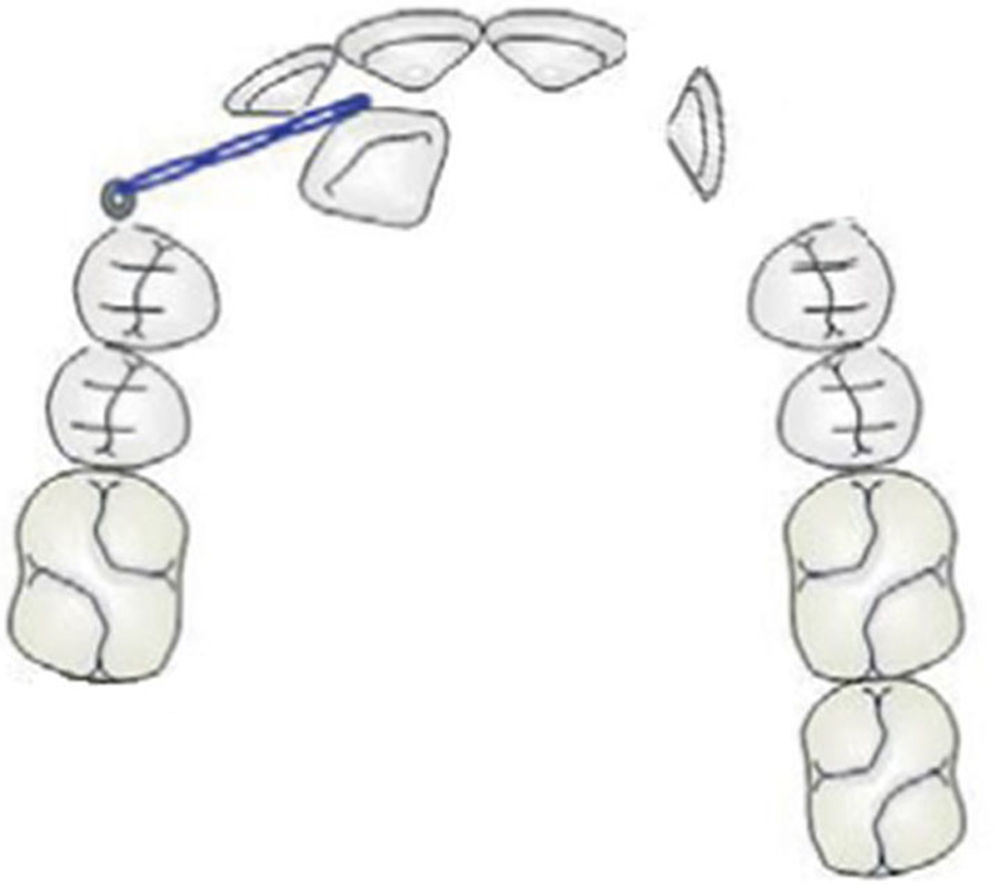
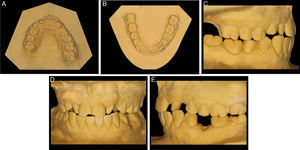
The extraoral clinical examination (Fig. 1) revealed pathognomonic clinical signs of AMC: multiple joint contractures, short stature, low set ears and dysplasia of the fingernails and toenails deployment. The analysis stressed a thin hypertonic upper lip and a low smile line TMJ clinical examination (by palpation, auscultation and mandibular kinetics evaluation) discarded clinical signs of temporomandibular disorder. The intraoral clinical examination (Fig. 2) showed a slight compression of the maxillary arch with anterior cross bite on teeth 12 and 22, Class II molar, decreased vertical overbite, upper lateral conoid incisors, absence of 18, 17, 13, 23, 28, 38, 35 and 48 and persistence of 53. In order to assess dental arch discrepancy, Bolton analysis12 revealed a discrepancy with excess on lower anterior arch (Fig. 3).
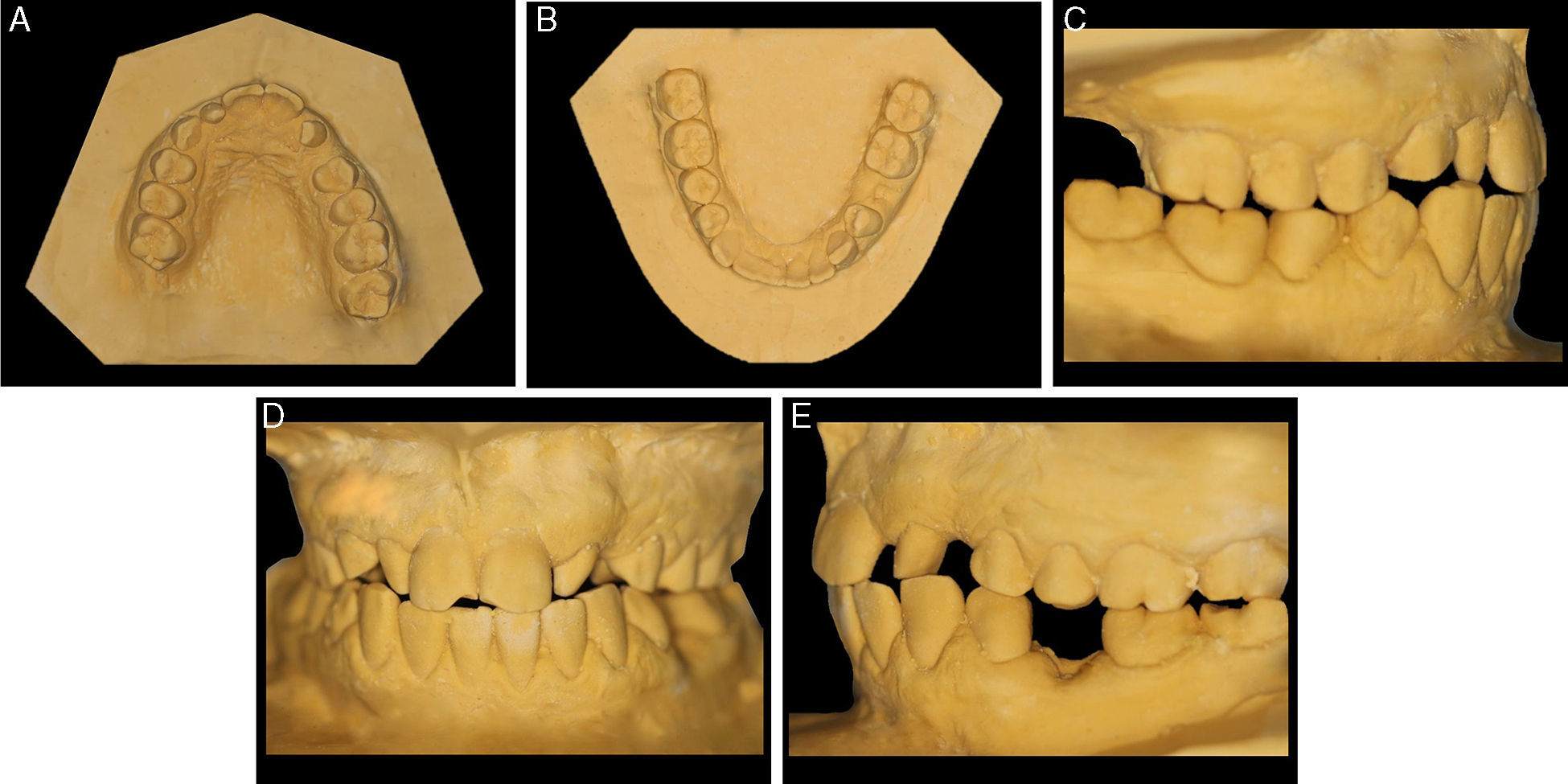
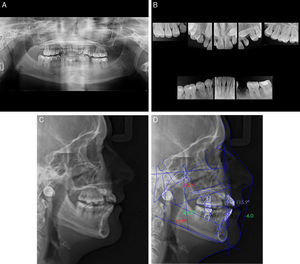
Panoramic X-ray (Fig. 4A) complemented by a retroalveolar X-rays status (Fig. 4B) revealed the inclusion of upper cuspid, agenesis of third molars (upper and lower), absence of 17 and 45 and a generalized severe dental root shortening.
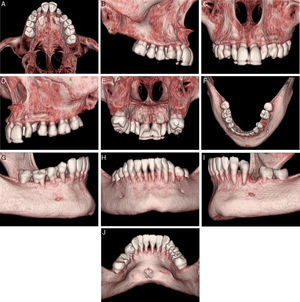
Ricketts cephalometric analysis (Fig. 4C and D) revealed a skeletal Class II, with a retro and micrognatic mandible, an orthopositioned maxilla, a mesocephalic facial type, proclined and orthopositioned upper and lower incisors, a decreased interincisal angle and a lip retraction. Functional analysis according to Multifunction System (MFS) classification13 showed type 1 nasal collapse (narrow nostrils without collapse), type 2 adenoids (slightly convex), type 2 tonsils (appear slightly), normal swallowing, nasal breathing, type 1 tongue mobility level (tongue touches the palate). In order to improve the perception of cuspid location, a computed tomography (CT) was requested (Fig. 5).
Discussion and conclusionsRoot shortening is a rare finding occurring in about 1.3% of general population, more frequent in females and involves mostly premolars and maxillary incisors14 with no reports of its association with AMC.
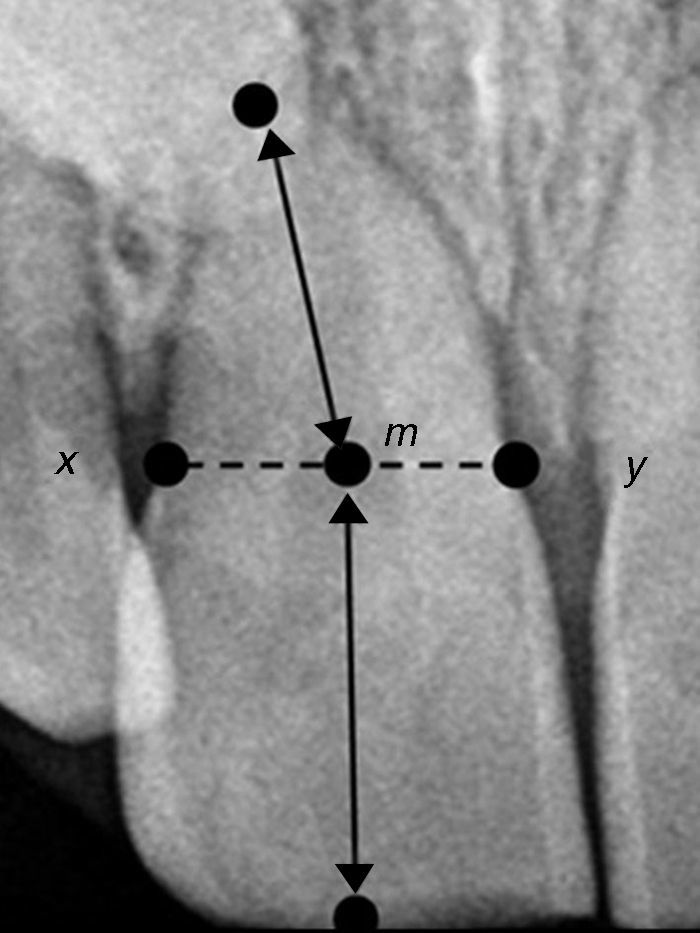
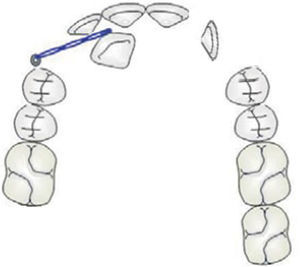
There are several radiographic measurement techniques of root/crown ratio (R/C) described in literature. In the present study the Lind method15 was the one selected for the assessment. According to it, the interproximal concavities between root and crown correspond to x and y points, being m the midpoint of x-y segment. The relative root length is calculated from the apex to m point and the relative coronal length is the distance between m point and the midpoint of the incisal edge. The performed evaluation revealed that most of the patient's teeth had a R/C ratio ≤1.0 (Fig. 6). According to Jakobsson et al.,16 roots are considered short when R/C ≤1.1.
In AMC cases, despite the limitations caused by dental morphology, orthodontic treatment can be considered in order to enable opening spaces for rehabilitation with dental implants in an attempt to restore the appearance and function. Partial fixed appliances may be used to avoid compromising periodontal structures of adjacent teeth while opening spaces for rehabilitation. However, partial appliances do not fix all dental positions and may pledge reaching goals related to the establishment of an ideal functional occlusion. Relative position and possibility of orthodontic traction of impacted teeth should be carefully considered prior to treatment. Bringing the impacted canine into a normal position is important in achieving a functional occlusion and final esthetics of orthodontic treatment, but factors such as height of the impacted canine, angulation of the long axis to the upper midline, canine mesiodistal position of the tip relative to the midline, adjacent incisors and the anteroposterior position of the canine root apex should also be considered.
In this particular case, the left canine presented a horizontal position and was in proximity with the roots of adjacent teeth. Therefore, extraction seems to be the most suitable option. As for the right canine, a more conservative approach would be adequate and it seems that the use of a mini-screw as a traction auxiliary device would be indicated (to be possible to traction using a mini-screw) (Fig. 7).
This may avoid loss of anchorage and outline periodontal limitations. Patients should be informed about the limitations of these procedures, such as, tooth ankylosis, possible compromise of adjacent teeth during root repositioning and the anatomy and position of the remaining teeth. The decision of tooth traction or extraction should be decided with the patient.
Rehabilitation phase can be done based on implant supported rehabilitation or using a removable partial acrylic denture. Dental-supported prosthesis has a limited prognosis in cases of low R/C ratio. As skeletal prosthesis require too much support on the abutment teeth, this option should be discarded.
In order to improve dental esthetics of conoid teeth, when present, esthetic restorations with composite resin may be held due to the already mentioned limited prognosis offered by fixed prosthesis.
In conclusion, a multidisciplinary approach is essential to solve this type of cases, covering areas such as genetics, oral surgery, orthodontics, implantology and esthetic dentistry. Comprehensive treatment must be individualized and adjusted to patient needs and, when required, subjected to adjustments in face of individual clinical response. R/C ratio may represent an important determinant and may affect the dental prognosis and complicate the orthodontic treatment and rehabilitation planning, if considering factors such as anchorage and functional and mechanical principles. Especially in orthodontic patients, this problem is emphasized and gets critical dimension, due to the high rate of root resorption in patients with previous root shortenings.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.