The non-recurrent inferior laryngeal nerve (NRILN) is a rare anatomic variation associated with subclavian artery abnormalities. In these cases lack of information about this situation increases the risk of iatrogenic damage of the nerve.
This article describes the incidental pre-operative identification of vascular anomaly and therefore the anticipation of the anatomical variant of right RLN in relation to a clinical case.
O nervo laríngeo inferior não-recorrente (NLINR) é uma variação anatómica rara associada a anomalias da artéria subclávia. Nestes casos, o risco cirúrgico de lesão do nervo aumenta.
Neste artigo é descrita a identificação incidental da anomalia vascular pre-operatoria e por isso antecipada a alteração anatómica do NLR direito a propósito de um caso clínico.
The inferior laryngeal nerve (ILN) innervates the intrinsic muscles of the larynx except the cricothyroid. It is also responsible for sensitive supply of the laryngeal region, below the vocal cords. The designation of recurrent is due to its anatomic location, since it is a loop of the vagus nerve, recurring inferiorly to the subclavian artery in the right side and the aortic arch in the left side.1 Being an essential structure to laryngeal functions and given the intimate relation with the thyroid gland, ILN identification and preservation are fundamental steps in thyroid surgery.
The NRILN is an anatomic variation first reported by Stedman in 1823.2 Its intraoperative identification and preservation can be a challenge even for the most experienced endocrine surgeon. Thus, the possibility of a preoperative diagnosis reduces the risk of inadvertent damage of the nerve.
The non-recurrent ILN is consistently related to the absence of brachiocephalic trunk and the presence of the so-called arteria lusoria on the right side. It only appears on the left side if associated with situs inversus. The preoperative identification of this variation if made should serve as a guidance/keynote to the presence of a NRILN.
Case reportWe herein present a case report of a 64-year-old male patient, without relevant associated pathologies, which was referred to an endocrine surgery evaluation with the diagnosis of a right thyroid lobe nodule that has been growing for 6 months. The patient denied other symptoms including dysphagia or hoarseness.
Physical examination detected a swelling at the base of the neck, on the right side, solid in consistency, movable with swallowing, without thrill, with 3cm diameter and with no palpable adenopathy.
Thyroid ultrasound was performed showing a nodular heterogeneous conglomerate with a cystic component, without microcalcifications or plunging component at the base of the right lobe, measuring 37.6mm×27.0mm×40mm. Left lobe had micronodules.
A fine-needle aspiration cytology ultrasound guided was carried out, and revealed: scarce and disperse colloid; abundant cellularity with isolated thyroid epithelial cells and clusters of variable volume and cohesion. The majority of these cells had cytoplasmic oxyphilic transformation. These aspects were compatible with Hürthle cell tumor.
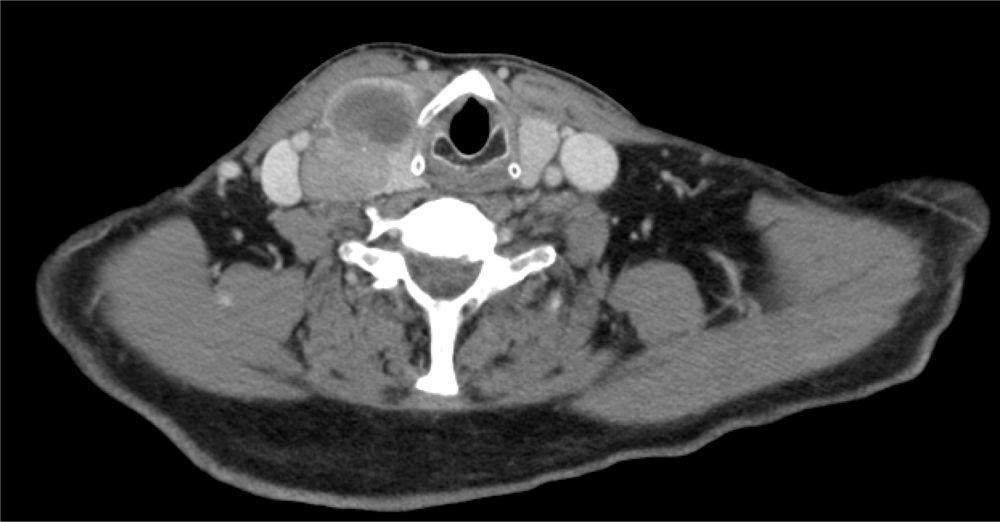
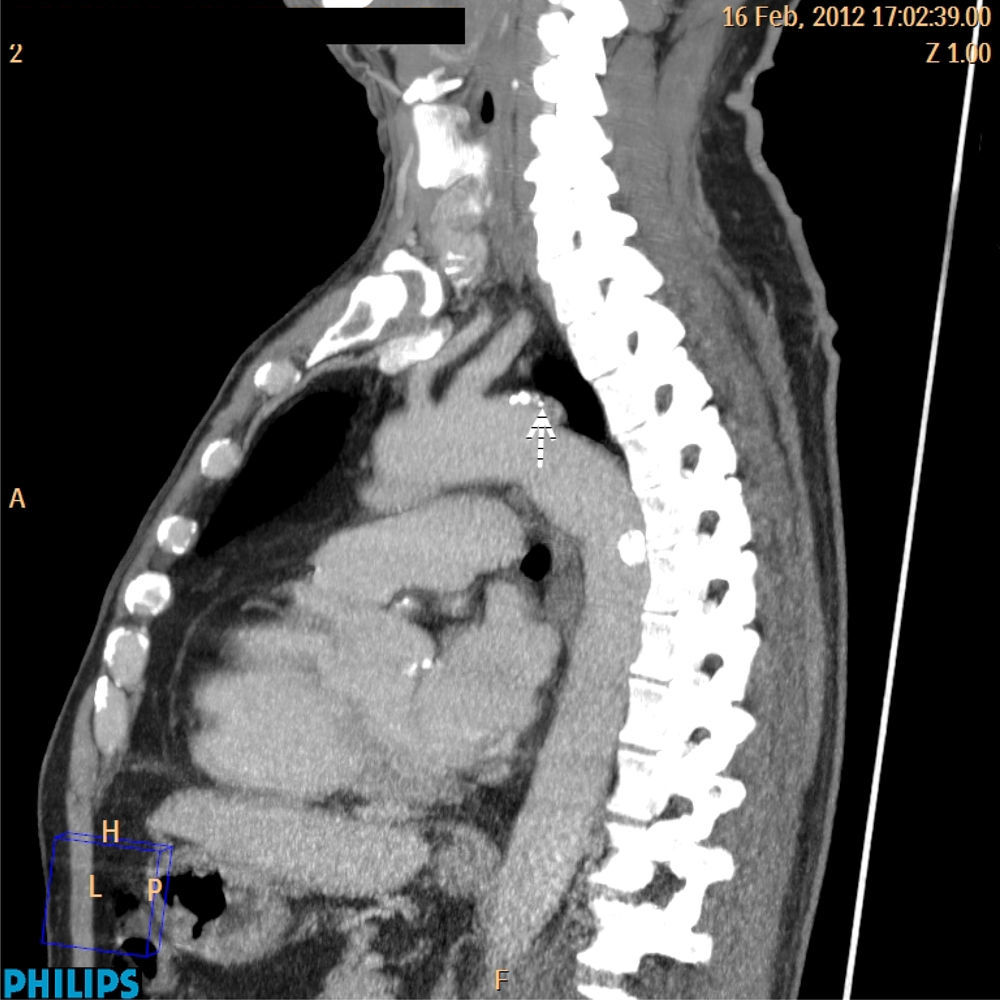
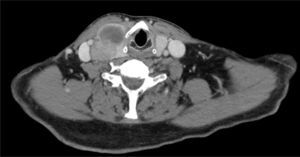
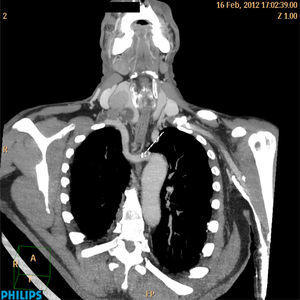
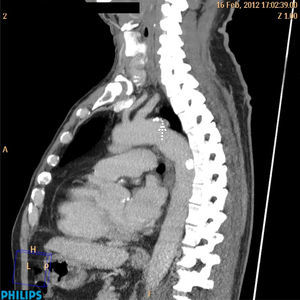
A CT scan of the neck without contrast, performed prior to consultation and requested by the patient's family doctor revealed enlargement of the right thyroid lobe by three expansive solid lesions (Fig. 1). The lesions were measured between 2.7 and 4cm. This volume increase of the right lobe exercised extrinsic compression and lateral displacement of the internal jugular vein, without clear invasive criteria and a slight casting on the tracheal right wall at the level of the thoracic operculum (Fig. 2).
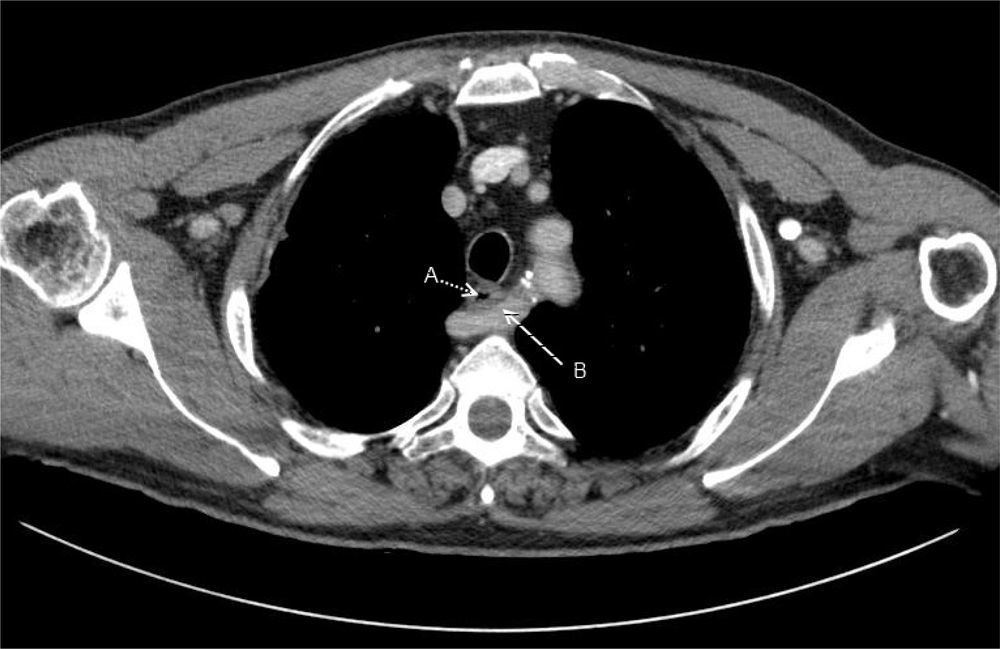
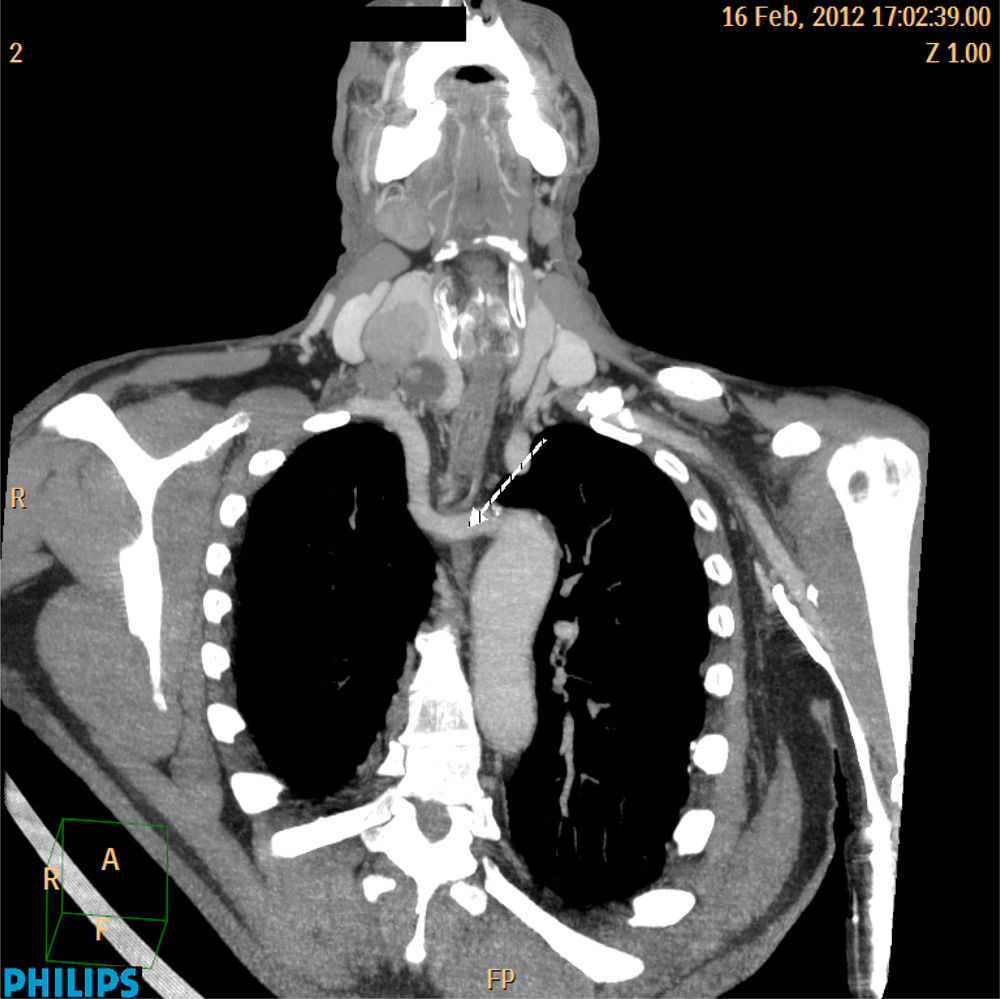
A congenital vascular abnormality with the right subclavian artery passing from left to right behind the esophagus (arteria lusoria) was identified (Figs. 3 and 4).
The CT evaluation led to the preoperative suspicion of NRILN diagnosis in the right and total thyroidectomy was proposed. CT of the neck is not routinely performed as part of the preoperational evaluation in patients with thyroid disease unless a thoracic component is suspected.
Preoperative vocal cord mobility was not assessed in this patient.
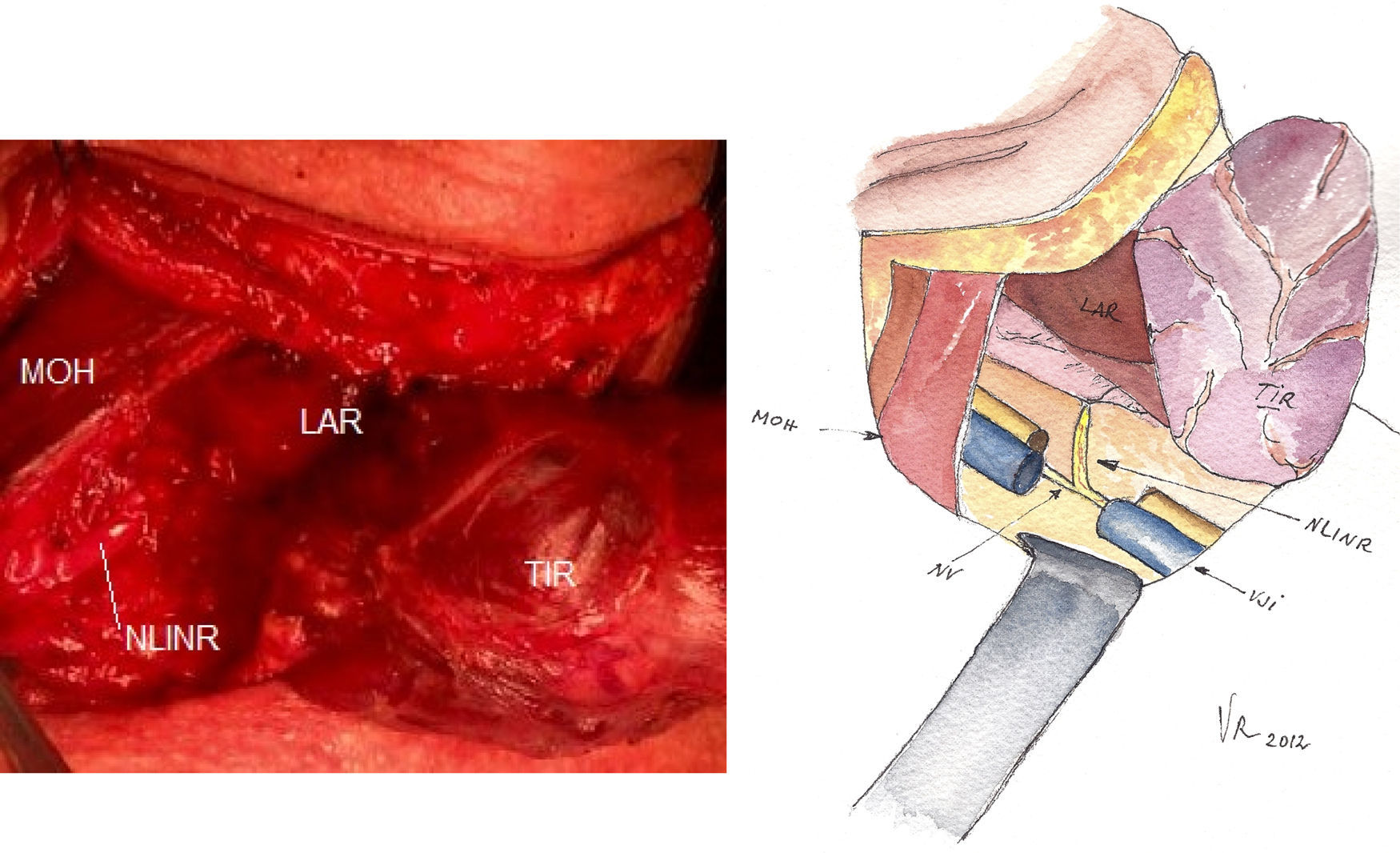
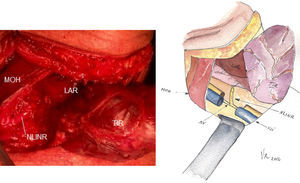
During surgery the anatomic vascular variant reported in CT was identified and the prediction taken from previous data was confirmed: the right ILN was not recurrent. It had its origin from the right vagus nerve in an almost straight angle toward the larynx (Fig. 5), not exhibiting the usual recurrent pattern in the tracheoesophageal groove. The left ILN featured a normal position.
Right side view of a patient with NLINR after total thyroidectomy. NLINR has its origin in the vagus and follows a transverse path parallel over the inferior thyroid artery. MOH, omohyoid muscle; LAR, larynx; TIR, thyroid; NLINR, non-recurrent inferior laryngeal nerve; NV, vagus nerve; VJI, Internal jugular vein.
Surgery and postoperative period did not have intercurrences or complications.
The surgical specimen anatomical pathology identified follicular variant of papillary carcinoma without extra thyroidal extension or vascular invasion: pT3NXMX. Remaining parenchyma had nodular hyperplasia. The patient did I 131 therapeutic in postoperative period.
DiscussionThe existence of anatomic variants in the path of the ILN is an additional reason to enhance their preoperative identification. One of these variants is the NRILN whose incidence ranges from 0.3% to 1.6% for the right and it is approximately 0.04% for the left.3
Its presence on the right is a consequence of a right subclavian artery variant that arises directly from the aortic arch behind the esophagus. Therefore, the absence of recurrence of the inferior laryngeal nerve results from an embryological variant.
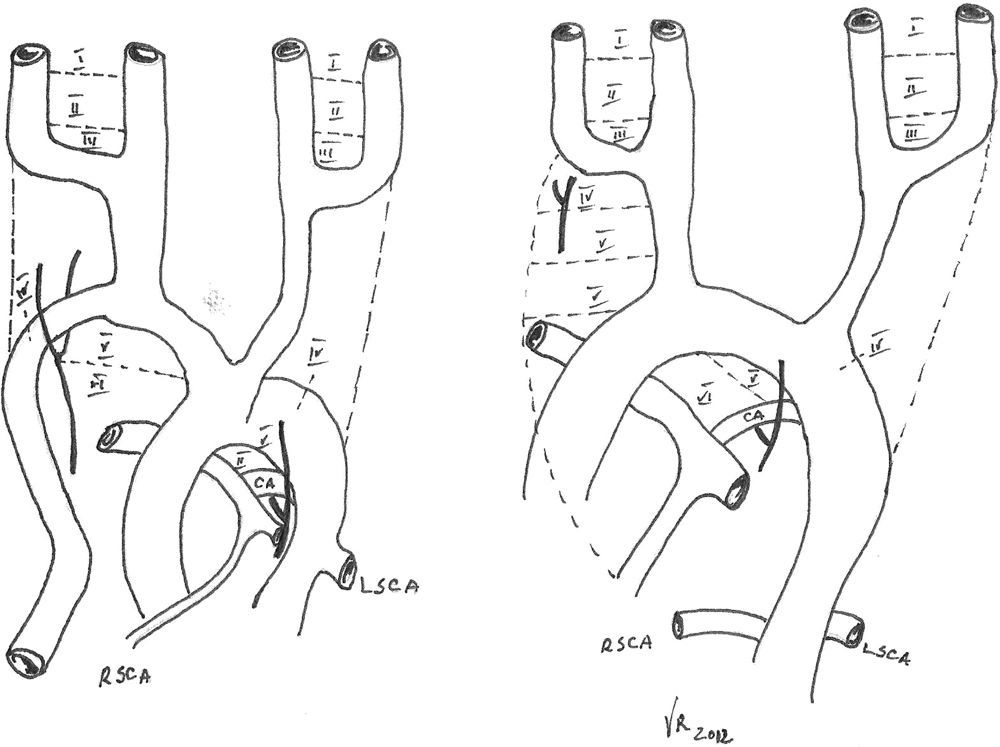
During embryological development, ILN originates from VI brachial arch, with vagus nerve under the same VI aortic arch and in a horizontal course.
Subsequently, the V and the distal portion of the VI aortic arches regress bilaterally and the two laryngeal nerves remain anchored to the structures that develop from the IV arch (subclavian artery on the right and aortic arch on the left). During their descent into the thorax, these arteries take with them the nerves that assume, therefore, a recurrent course. As reported by Devèze et al.,4 on the right side, the ILN moves up beneath the IV arch, which forms the initial portion of subclavian artery. When this portion of the IV aortic arch is absent, the arterial segment under which the ILN makes its loop is missing. The right ILN is now free to migrate upwards arising directly from the vagus nerve, at cervical level, reaching the right thyroid lobe transversely (Fig. 6). Right subclavian artery arises distally to the left subclavian artery, directly from the aortic arch. Subclavian artery crosses the mediastinum behind the esophagus to reach the right axillary area – arteria lusoria. Even though this vascular change is usually asymptomatic, about 5% of these patients report dysphagia (dysphagia lusoria). This vascular variant is exceptional on the left side and always associated with a situs inversus.3
Normal embryological evolution (left) and in case of non-recurrent inferior laryngeal nerve (right). [7].
Two types of non-recurrent ILN were defined: type 1: arises directly from vagus and runs together with superior thyroid vessels; type 2A: parallel transverse path, over the trunk of inferior thyroid artery; and type 2B, parallel transverse path, under the trunk or between the inferior thyroid artery branches.3,5
In this case the nonrecurrent inferior laryngeal nerve was classified type 2A.
CT diagnosis of arteria lusoria is based on the identification of an aberrant vessel that passes behind the esophagus.6
It is possible to predict the presence of a nonrecurrent inferior laryngeal nerve by identifying the presence of an arteria lusoria and the absence of the brachiocephalic artery on a preoperative CT scan.
It is also possible to predict the presence of a nonrecurrent inferior laryngeal nerve by identifying the arterial anomalies constantly associated with nonrecurrent inferior laryngeal nerve by preoperative ultrasonography. Ultrasonography is a very reliable and simple method to be used in preoperative assessment to identify vascular anomaly associated with NRILN to make optimal surgical decisions against nerve damage in patients undergoing thyroidectomy. But again, adequate surgical technique maintains great importance.7,8
Intraoperative neuro-monitoring (IONM) in thyroid surgery has recently been introduced, and its use has expanded quickly, allowing the surgeon to recognize and differentiate “true” branches of the inferior laryngeal nerve (ILN) from sympathetic anastomoses, as well as NRLN during surgery.9
There is some evidence that IONM may provide additional benefits beyond those afforded by visual nerve identification alone. But with visual identification remaining the basis for nerve protection, it is up to every surgeon whether to use IONM as a routine adjunct. We believe that especially in experienced hands, the recurrent laryngeal nerve palsy rates are so low that prohibitively large numbers of patients would be needed to achieve adequate statistical power.10
ConclusionNonrecurrent inferior laryngeal nerve incidence is very rare, but when present, increases the risk of damage during thyroidectomy.
Preoperative imagiologic diagnosis of arteria lusoria and dysphagia lusoria may suggest its presence. The present case report described a patient without dysphagia and NRILN was an accidental discovery through CT scan.
We decided to present this case because it highlights this anatomical variant. There are auxiliary methods that allow intra-operatory identification, as Intraoperative neuro-monitoring (IONM).
The knowledge of its presence and a correct surgical technique minimize morbidity.
Conflicts of interestThe authors declare no conflicts of interest.



![Normal embryological evolution (left) and in case of non-recurrent inferior laryngeal nerve (right). [7]. Normal embryological evolution (left) and in case of non-recurrent inferior laryngeal nerve (right). [7].](https://static.elsevier.es/multimedia/16463439/0000000900000001/v1_201407280026/S1646343914000133/v1_201407280026/en/main.assets/thumbnail/gr6.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
