The clinical features of the skin and mucosa as well as the dermatological pathologies of patients with Down syndrome are sometimes chronic and difficult to treat. Intense xerosis and perioral dermatitis result in a therapeutic challenge for the specialist. Multidisciplinary and proactive management involving the family and the patient who is able to understand and follow routines are fundamental to avoid common complications such as superinfection. New cosmetic formulations that include active agents capable of protecting and restoring barrier function are helpful in avoiding comorbidities and excessive drug use. The authors perform a review of the main pathologies and specific conditions of the skin as well as the measures for its correct management.
Las características clínicas de la piel y mucosa así como las patologías dermatológicas de los pacientes con síndrome de Down son en ocasiones crónicas y de difícil manejo. La xerosis intensa y la dermatitis peribucal resultan en un reto terapéutico para el especialista. El manejo multidisciplinar y proactivo involucrando a la familia y al paciente que es capaz de entender y seguir rutinas resultan fundamentales para evitar complicaciones comunes como la sobreinfección. Las nuevas formulaciones cosméticas que incluyen activos capaces de proteger y restituir la función barrera son de ayuda para evitar las comorbilidades y el uso excesivo de fármacos. Los autores realizan una revisión de las principales patologías y condiciones específicas de la piel así como de las medidas para su correcto manejo.
Down syndrome (DS) results from increased genetic material on all or part of chromosome 21, and causes intellectual disability, morphological and phenotypic characteristics and carries the risk of comorbidities in different organs and systems.1 The syndrome affects approximately 1 in 1000 births and the mean survival age is from 50 to 60 years. In addition to cardiovascular, respiratory, endocrine and metabolic disorders, DS patients present a series of chronic dermatological conditions that affect their skin and mucous membranes.2,3
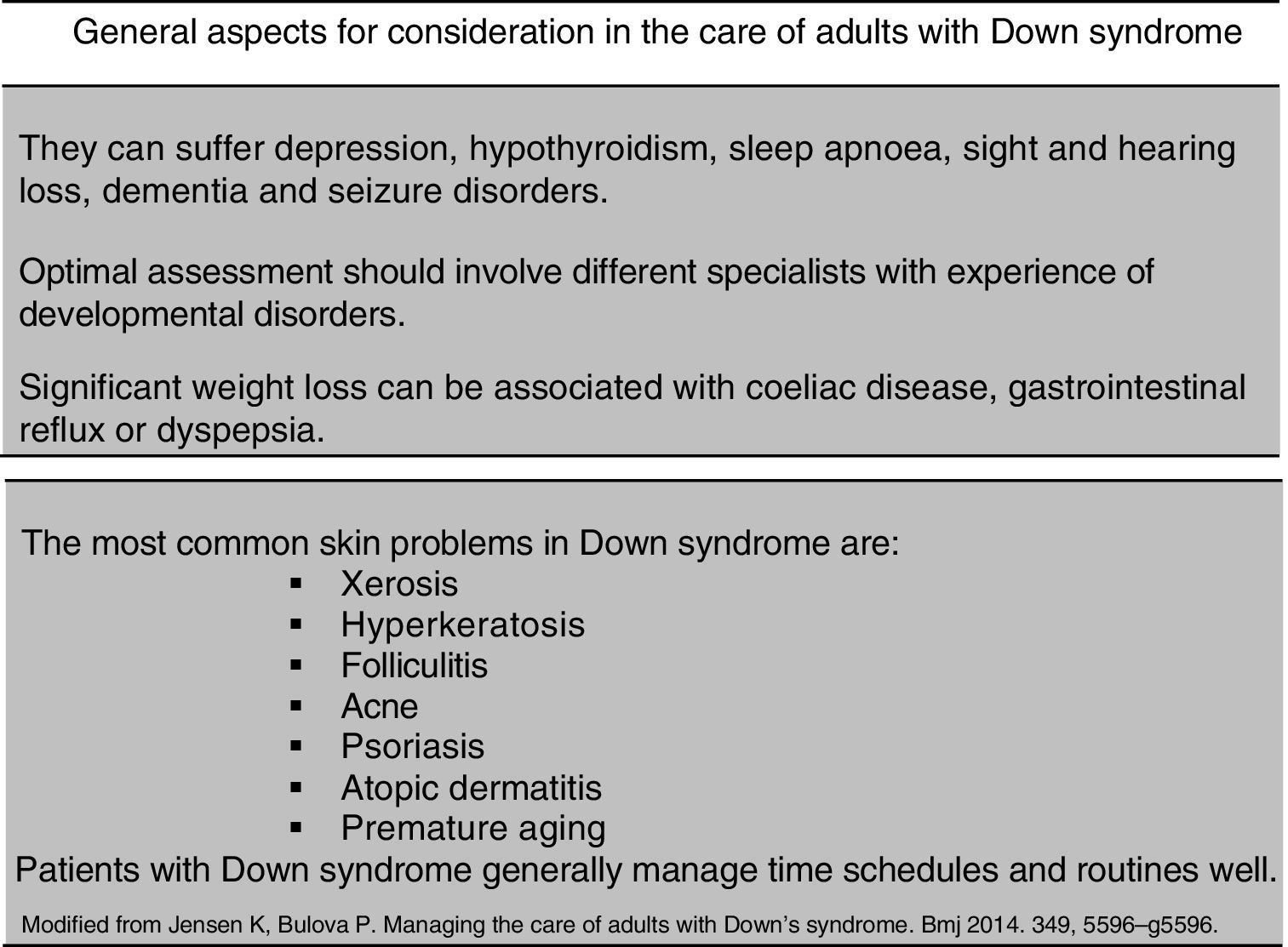
These conditions, even when very prevalent, are often considered less serious than the other comorbidities. However, the various skin disorders can have a considerable impact on the quality of life of these patients (Fig. 1).
There are diverse and comprehensive reviews in the literature on the different skin conditions that DS patients present, such as: alopecia areata, vitiligo, nail bed conditions, calcinosis cutis and syringomas.3–8 We only mention cutaneous xerosis and perioral dermatitis in this review, since these are two common manifestations that are little reported in the literature. Knowledge of these disorders will enable better understanding of their possible aetiology and management, and help to prevent complications.
XerosisXerosis or skin dryness is a common disorder in DS patients. Although its aetiology is still not fully known, accelerated skin ageing and the high prevalence of atopic dermatitis in these patients appear to be the principal predisposing factors.
Patients with DS suffer premature skin ageing, reflected in their greater predisposition to lentiginosis and skin wrinkles, as well as the onset of xerosis with secondary eczematisation. It is estimated that around 70% of patients with DS have moderate to mild generalised xerosis, predominating on the ankles, knees and legs. Xerosis causes patients to scratch, which in turn causes lichenification lesions and occasionally excoriation and superinfection. Localised areas of lichenification appear in 30% of patients under the age of 10 and 80% of those aged over 20 years. These simple chronic lichen lesions are more common on the arms, wrists, anterior thighs behind the ears and nape of the neck.
The high prevalence of atopic dermatitis in DS patients is very much associated with xerosis, and is found in up to 50% of cases according to the series. The most frequently found signs included keratosis pilaris4 and palmoplantar hyperkeratosis with an incidence of around 75% from the age of five years.3
The presence of these disorders in the skin barrier (xerosis and atopic dermatitis), often associated with poor hygiene, puts the DS patient at greater risk of bacterial, fungal and parasitic skin infections.8
Impetigo is one of the principal bacterial infections. This is mainly present in children and affects the extremities as well as the facial region, which occurs in healthy children.5 The mycotic infections include folliculitis due to Pityrosporum ovale and dermatophyte infections (tinea). Folliculitis due to Pityrosporum ovale generally occurs in males between the ages of 20 and 40 years as a follicular skin rash in the interscapular and presternal area.4 It is occasionally also associated with seborrhoeic dermatitis, and affects the usual places such as the face, scalp and presternal area.3–6
Dermatophyte infections include tinea pedis and onychomycosis. These infections are usually chronic and are found in more than 50% of patients. They generally occur after puberty, especially in institutionalised patients.
In terms of parasitic infections, children with DS are more prone to severe forms of scabies such as crusty or Norwegian scabies. Although the reason for this predisposition is unknown it is believed that it might be due to specific immunosuppression to the parasite. With this condition, thickened or hyperkeratotic plaques appear on the buttocks and flexural areas.7
Perioral dermatitisPerioral dermatitis is common and very characteristic of patients with DS. It manifests as papules and inflammatory plaques around the mouth and chin. It can extend from transitory redness, exudation, flaking, the formation of crusts and itching to serious tumefaction spreading to other areas. With persistent scratching, it can become lichenified.
These lesions are encouraged by some of these patients’ anatomical and functional conditions.
Anatomically, patients with DS have an unusually large tongue, known as macroglossia. This can also be associated with a fissured or geographic tongue. The lips tend to be thin and fissured, and these patients often have sialorrhoea or hypersalivation. All these factors, often associated with a small oral cavity, favour the development of cheilitis and perioral dermatitis and even early, severe periodontal disease.9–12
With regard to the functional disorders that explain the greater prevalence of perioral dermatitis, experimental studies have shown that the saliva of patients with DS is not the same as that of people without a genetic disorder. Analysis of the parotid gland secretions of DS patients show considerably higher pH and sodium, calcium, uric acid and bicarbonate content, with reduced secretion speed. It is believed that this might be an important factor in the particular susceptibility of these people to periodontal disease and dental caries.11
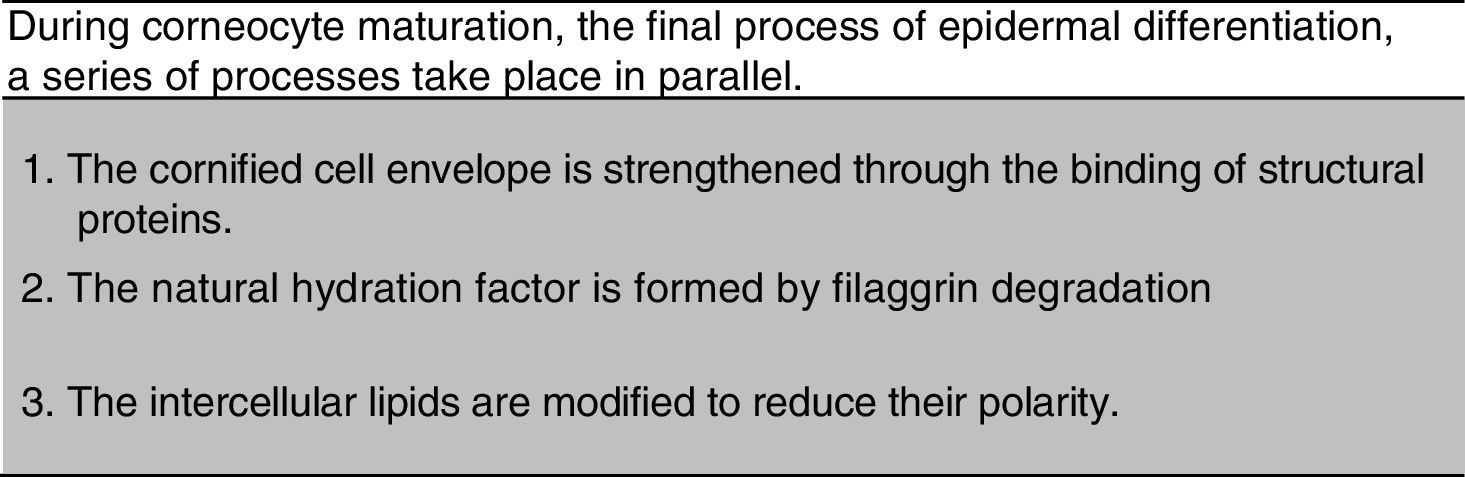
Increased skin pH and calcium in saliva, associated with permanent humidity in the perioral area (anatomical area of the facial region comprising the nasogenian fold and furrows) are the principal factors that cause deterioration of the barrier function and a loss of lipid cohesion in this area.12 If the skin is irritated its pH changes, altering the normal function of the skin enzymes responsible for lipid synthesis. The enzyme activity of the stratum corneum is intimately related to its pH gradient. In relation to humidity, it is known that the lipid bilayer of the stratum corneum in humans is not constitutionally prepared to permanently support an aqueous medium, although it does have a temporary barrier effect to prolonged exposure to water. The degree of functionality of the skin barrier is proportional to the total lipid content. A loss of barrier function in the corneal layer is often associated with a disorganised keratinisation process (Fig. 2). The cementing substance of the corneocytes has a liquid crystalline structure that requires a minimal presence of water, which is found in sheets in the polar areas of the lipids organised into lamellar bodies. Prolonged exposure of the skin to water causes changes in the skin's morphology and results in constant tension and cumulative damage to the stratum corneum, and even loss of barrier function, which then becomes a loss of lipid cohesion.13,14
It has been observed recently that calcium plays an essential role in the development of perioral dermatitis in these patients. For skin barrier formation, the lipids that are secreted in the first instance such as the glucosylceramides, cholesterol and phospholipids need to be metabolised and subsequently transformed into ceramides, cholesterol and fatty acids. This process requires an acid medium (physiological acidity of the corneal stratum) and the presence of calcium ions that enable the activation of certain enzymes. This has been demonstrated in vitro from liposomes constructed with corneal lipids.13 The glucosylceramides via the enzymatic route, without doubt modulated by the calcium gradient and acid pH, become released from glucose residue to become ceramides. The enzyme responsible for this transformation is called glucocerebrosidase. The lack of enzymatic activity by the beta-glucocerebrosidases, results in an abnormality in the barrier which appears to be attributable to the accumulation of glucosylceramides, and not to the depletion of ceramides. This biochemical change is accompanied by the persistence of immature membrane structures through the interstices of the stratum corneum, which, although unsuitable for supplying atmospheric lifetime, seem to be insufficient for the mucous epithelium. The enzyme beta-glucocerebrosidase is reduced in the oral mucosa, which indicates that the presence of ceramides in these tissues is not so necessary (this also indicates less demand on the requirements of barrier function). Without any doubt, the mechanisms that regulate this lipid conversion are calcium dependent. Variations of extracellular calcium levels induce changes in the surface proteins and the mechanisms of cell–cell and cell–lipid surface adhesion.14
The calcium ion is involved in the maintenance of intercellular adhesion and regulation of the enzymatic systems, playing a determining role in keratinocyte differentiation. There is an optimal concentration of calcium that is able to regulate cellular differentiation in vitro, including the expression of granular cells in terms of the production of filaggrin and keratin precursor. An increase in calcium will inhibit this differentiation.
The important of skin hygiene and hydrationMaintenance therapy for xerosis is essential to enhance the quality of life of these patients. Improved skin hydration against the environment is necessary and factors that cause dryness must be avoided, such as aggressive detergents and soaps.
The use of emollients should be adapted to the skin that requires treatment. Personalised xerosis treatment, and the use of specific emollients that have been prescribed by the specialist are beneficial to these patients.15
There are several aspects of xerosis in DS that require correction. It is affected by external factors such as the weather, dry heat, wind, cold, UV radiation and chemical aggression from medicines and detergents, as well as endogenous factors of the genetic condition itself that result in accelerated ageing, oxidative stress and immune system abnormalities, as we have already mentioned.
Xerosis can be improved by promoting correct epidermal differentiation. In fact, an altered process of differentiation carries with it other lipid and protein dysfunctions. The immune status of the skin of patients with Down syndrome suppresses the expression of the keratinocyte differentiation markers, and correct lipid synthesis. This situation has a direct effect on the skin barrier.16–19
It is essential to normalise this process to improve the barrier function and thus limit water loss while protecting and repairing the skin against external aggression.
The ideal emollient, therefore, should include ingredients that are able to improve corneocyte maturation and epidermal differentiation, provide physiological mimetic lipids, and general and film-forming emollients for protection. This will limit water loss; it is important to ensure the skin's water content.
The stratum corneum of the epidermis contains 15–20% water. If this percentage drops to 10%, the skin will lose its biomechanical properties and appear dry.
The inclusion of hygroscopic, hydrocaptor and moisturising agents in formulations ensures hydration, and the inclusion of antioxidants protects against ageing.
Often dry skin is accompanied by irritation and an itching sensation which can be managed by soothing ingredients such as glycine or allontoin.
Hyperkeratosic areas can be associated with the xerotic condition. In this case, an emollient is necessary that can eliminate this skin thickening by degrading the keratine with a keratolytic such as 20% urea, and complete its action with agents to normalise desquamation, such as intrinsic hydrolytic enzyme activating ingredients.
External aqueous phase creams or lotions are preferable, since they are better accepted by patients, but we must ensure that the product contains film-forming ingredients to protect against the environment.
Products that contain alcohol must be avoided, since these can dry the skin further. The hydrating-emollient emulsion should preferably be applied after bathing.
Bath produces should not include soap and be based on very gentle surfactants, and if possible include lipid-replenishing ingredients. Hygiene products must be compatible with the skin and prevent the following: change in pH, excessive elimination of skin lipids and protein denaturation.
Because the immune system of Down syndrome patients can make them more susceptible to infections, it might be advisable to include an agent that can control the growth of the principle opportunistic micro-organisms such as Staphylococcus aureus.
Including prebiotics in some emollient formulations used to treat atopic dermatitis has been demonstrated to be useful in bacterial control without using broad spectrum bactericides that endanger the skin's natural microbiome.
Although repeated bacterial infections are common, folliculitis is even more so and is usually resolved by pharmacological intervention.
Final considerationsThe correct use of hygiene guidelines and specific skin care for Down syndrome patients is very important, not only in maintaining the health of the body's largest organ but also as a means through which they can receive the affection of their caregivers and learn to take care of their own health.
It is very useful to use products that protect skin exposed to saliva, since the permanent action of saliva on the skin damages its barrier function. Protective and regenerative treatment helps to keep the perioral and chin area in good condition and to protect the skin against other irritants such as food and pollution. The appropriate product for this purpose must have emollient, protective, astringent, soothing, non-occlusive film-forming properties and, if possible, ion-sequestering capacity.
The xerotic skin of patients with Trismomy 21 merits special and specific care to prevent the onset of comorbidities such as folliculitis and eczema.
It is important to understand the dermatological features of Down syndrome patients to ensure their correct management and care.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Piquero Casals J, Serra Baldrich N, Rozas E, de Montserrat R. Fisiopatología y manejo de la xerosis y alteraciones orales en pacientes con trisomía 21. Rev Med Int Sindr Down. 2017;21:46–50.