Lung cancer is the leading cause of cancer death in both sexes, accounting for nearly a third of all cancer deaths. It causes more deaths than breast, colon, prostate and pancreatic cancer combined. Their overall 5-year survival rate is 15%, however, if caught in early stages it can reach up to 60–70%. Unfortunately, over 70% of lung cancers occur in advanced stages. For early clinical stages of non-small cell tumours, surgical treatment is usually recommended. Recently, the video-assisted thoracic surgery approach has proven to be at least equivalent to open surgery regarding oncologic principles, also showing the advantages of a minimally invasive procedure. In this occasion we present the case of a patient with lung cancer IIB on whom a lobectomy was performed using a minimally invasive approach. The patient was discharged three days after surgery.
El cáncer de pulmón es la principal causa de muerte por cáncer en hombres y mujeres, dando cuenta de casi una tercera parte de todas las muertes por cáncer, causando incluso más muertes que los cánceres de mama, colon, próstata y páncreas juntos. Su sobrevida global a 5 años es de 15%; sin embargo, si se detecta en estadios tempranos puede alcanzar hasta el 60-70%. Lamentablemente más del 70% de los cánceres de pulmón se manifiesta en estadios avanzados. Para estadios clínicos tempranos de tumores de células no pequeñas, el tratamiento indicado es generalmente quirúrgico. Recientemente el abordaje por cirugía torácica videoasistida ha demostrado ser al menos equivalente a la cirugía abierta con respecto a principios oncológicos, mostrando además las ventajas de un procedimiento de mínima invasión. En ésta ocasión presentamos el caso de una paciente con cáncer pulmonar estadio IIB a quien se realizó lobectomía con abordaje de mínima invasión, egresándose del hospital a los tres días de operada.
Lung cancer is the leading cause of cancer death worldwide for both sexes. In 2012 the World Health Organization reported a rate of 1.8 million new cases worldwide.1 With a 5-year survival rate of only 17%, totalling nearly one-third of all cancer deaths in the United States and causing as many deaths as breast, colon, prostate and pancreatic cancer combined. However, if the disease is diagnosed and treated in its early stages, the 5-year survival rate increases to 60–70%.2
In 2006, 1770 cases of lung cancer were reported in Mexico alone, which was 1.67% of the total number of cancers reported3; unfortunately, this is believed to be due to significant underreporting.
Sadly, despite being curable if caught in the early stages, 70% of patients presented in advanced clinical stages.4
A potential risk factor for lung cancer is smoking. Someone who smokes more than 20 cigarettes per day is 20–30 times more likely to develop lung cancer. However, more than half of the patients diagnosed with lung cancer tumour antigen never smoked or smoked several years earlier. Overall, lung cancer is still more common in men than in women, but the rate in men has been on the decline, probably as a result of national campaigns to reduce tobacco use.2
Lung cancer can be separated roughly into 2 groups: “Small Cell” and “Non-Small Cell”. This division is popular because, in general, non-small cell tumours can be treated with surgery when located, unlike small cell tumours that are treated with chemotherapy or radiation. The three most common types of non-small cell tumours are: Adenocarcinoma, Squamous Cell and Large Cell.5
Currently, the NCCN (National Comprehensive Cancer Network) guidelines recommend surgical resection and mediastinal lymph node dissection or sampling for non-small cell lung cancer in clinical stages I to IIIa (smaller than 7cm, without mediastinal adenopathy), without endobronchial extension.6
On this occasion we present the case of a patient with non-small cell lung cancer of the right lower lobe EC IIB T2bN1M0, on whom a lobectomy was performed using minimally invasive surgery, the first of its kind to be carried out in the Hospital General de México, which is one of the tertiary referral public hospitals in Mexico City and also a major teaching hospital.
Case report79-year-old female, with no history of smoking or exposure to biomass. She started a year previously with an intermittent bloody productive cough. Six months ago, her symptoms were exacerbated, and a chest X-ray was initially performed with a finding of a right solitary pulmonary nodule in the lower right lobe.
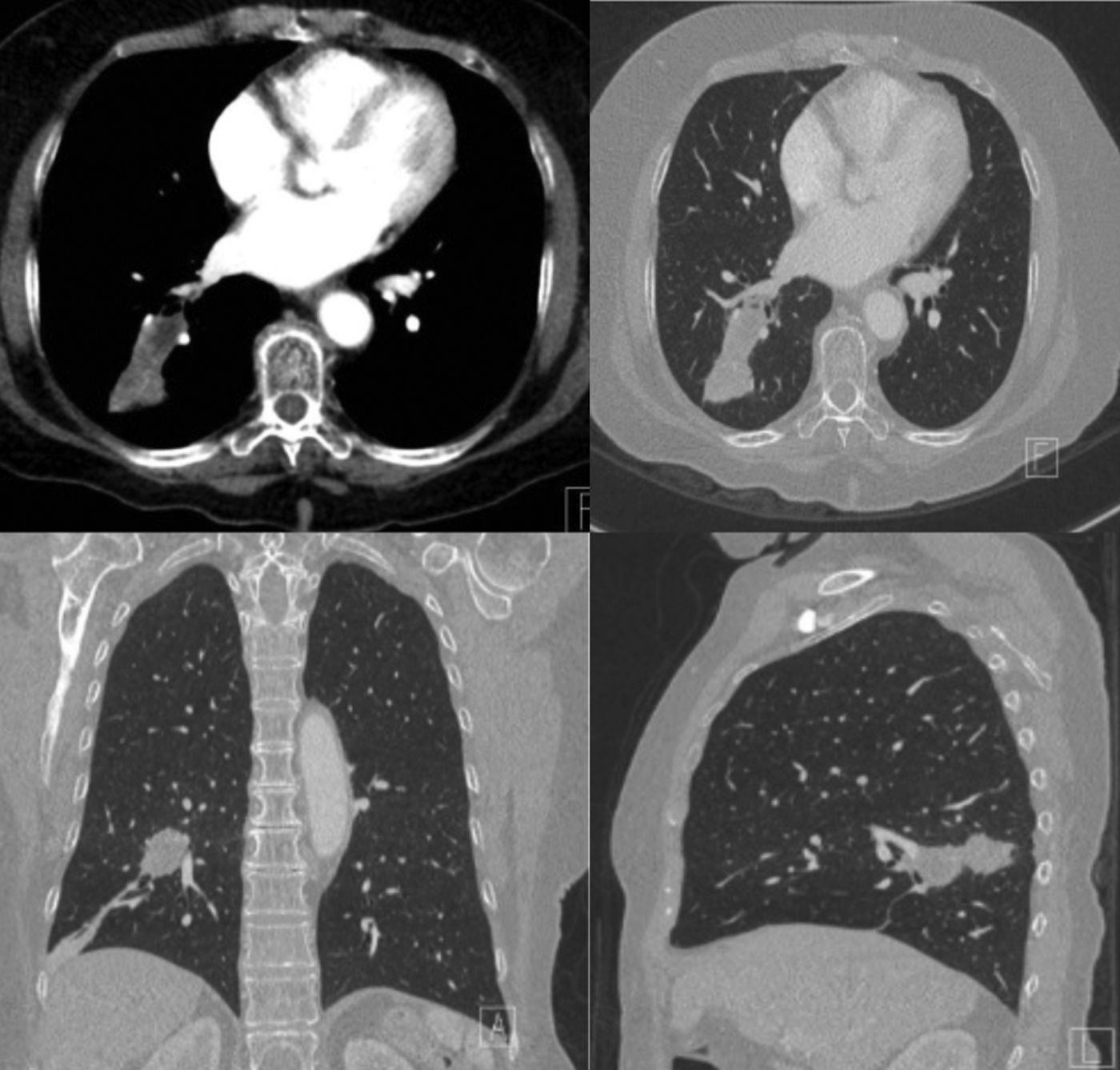
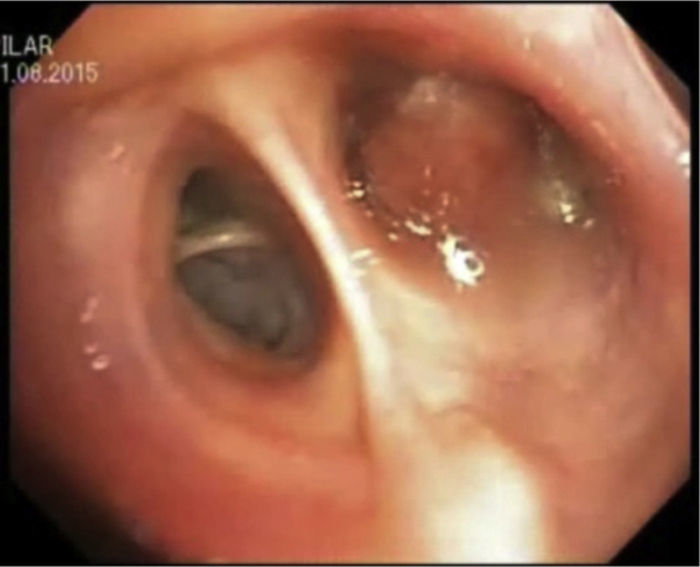
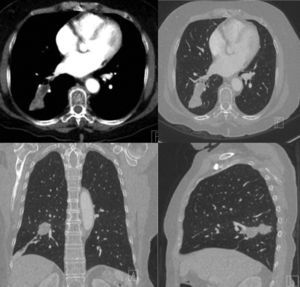
A chest tomography was subsequently taken (Fig. 1), in which the lesion observed in the chest X-ray that was thought to be malignant appears, in the upper segment of the right lower lobe measuring 5cm×7cm with irregular defined edges, and areas of necrosis. The magnetic resonance of the skull was reported without metastatic lesions. A bronchoscopy was performed (Fig. 2) with a biopsy of the lesion being taken that occupied the entire lower right segment 10, with a histopathological result of adenocarcinoma.
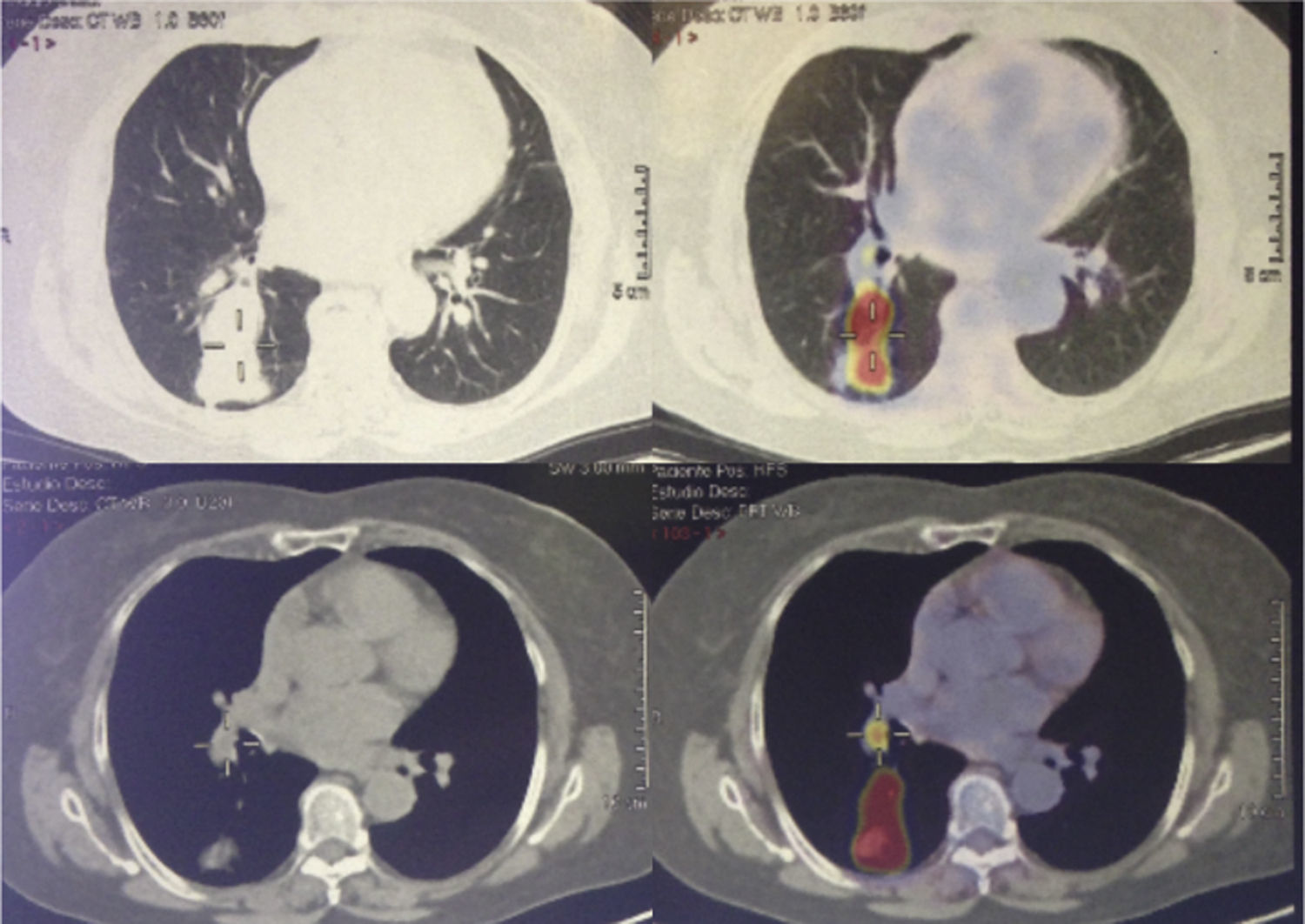
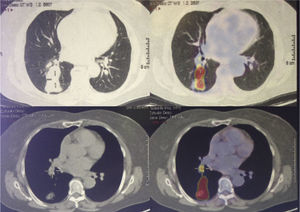
The PET-CT (Fig. 3) shows a tumour of the right lung with increased metabolic activity (SUVmax 10.67) and right interlobar adenopathy of 7mm with SUVmax of 3.79.
The patient was catalogues with a right lung cancer, adenocarcinoma EC IIb T2bN1M0, and a candidate for surgery because the tumour was considered as resectable in imaging studies and the patient had no contraindication for surgery.
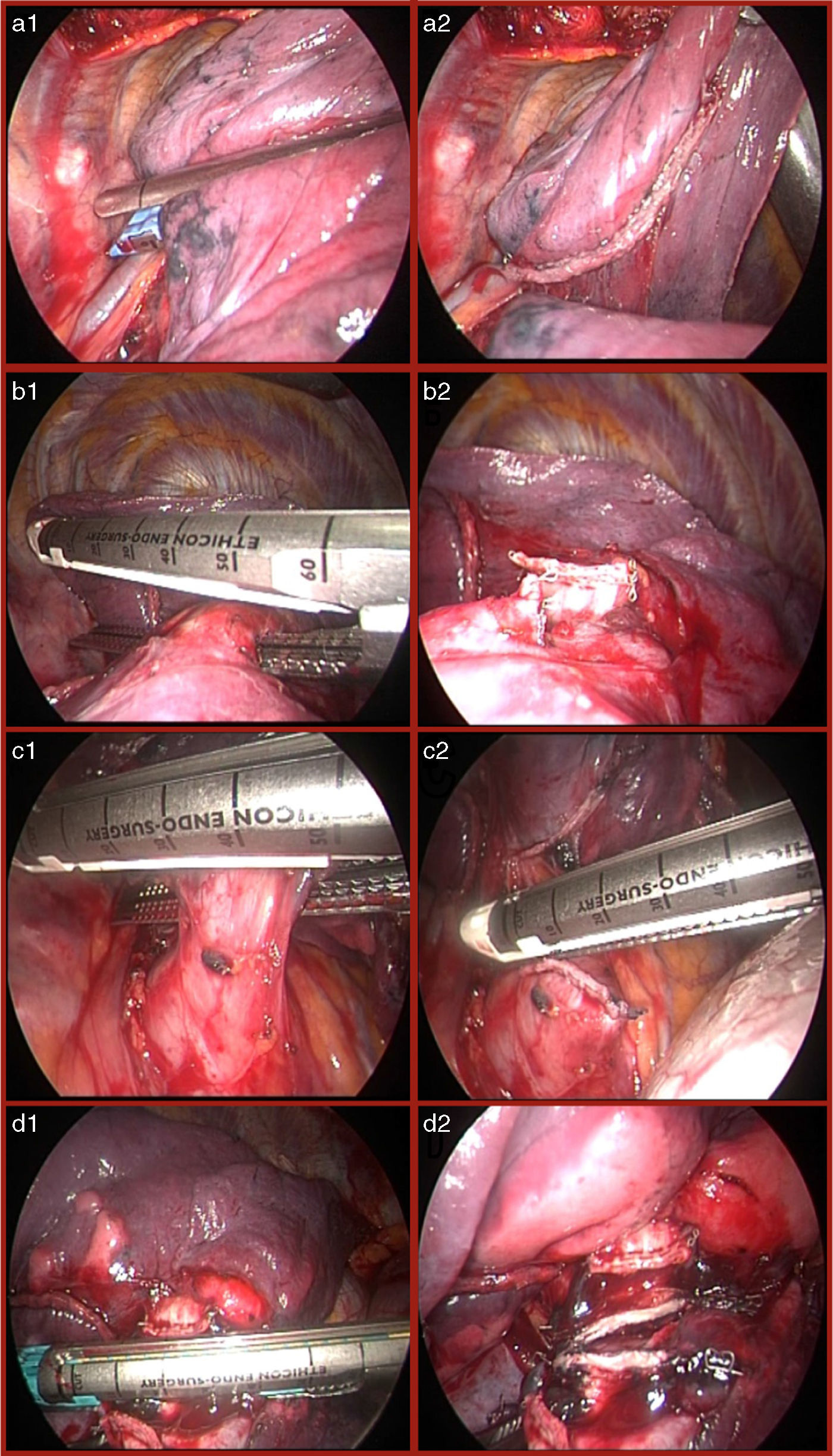
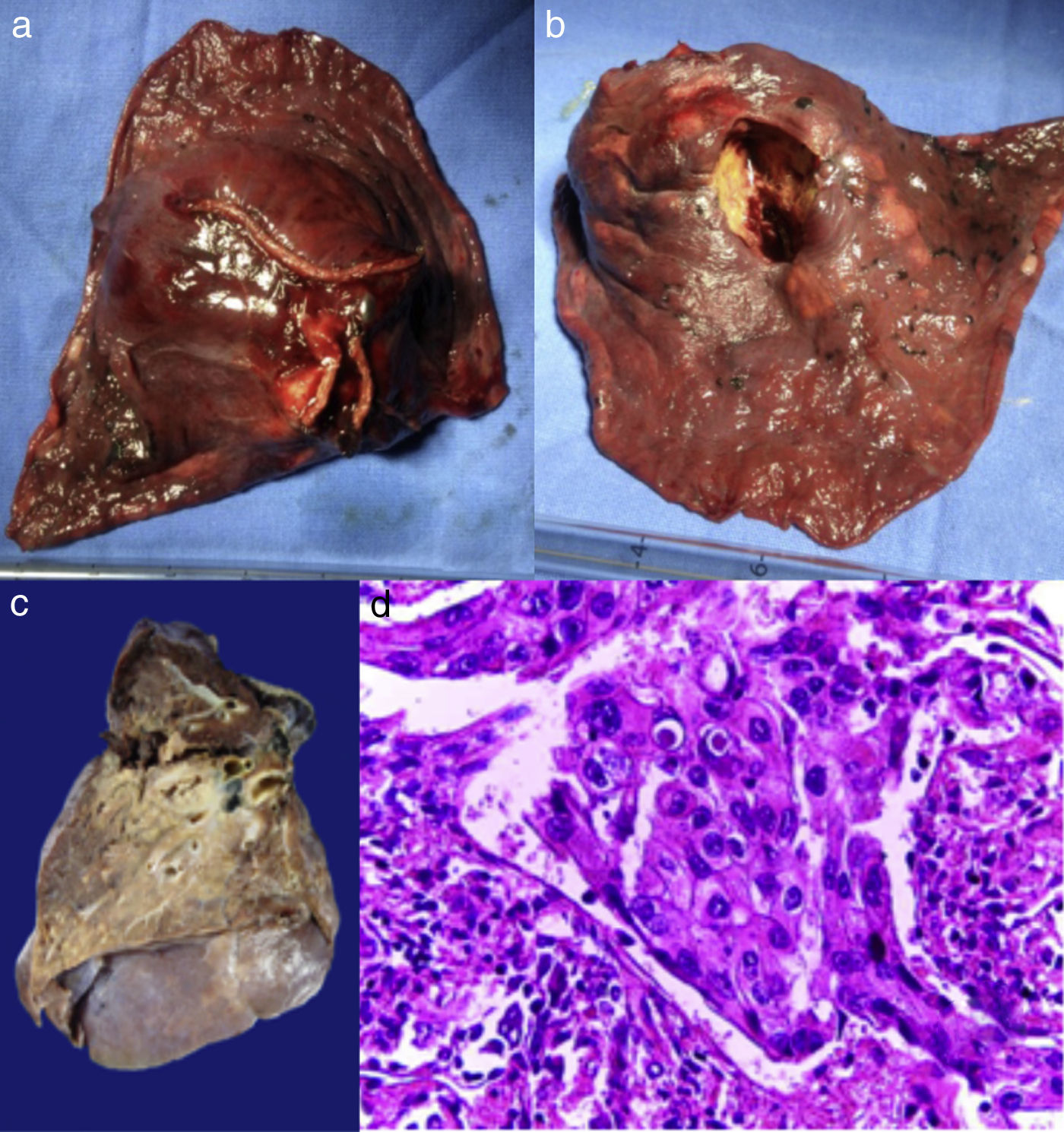
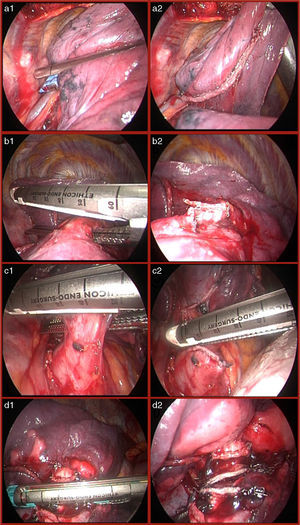
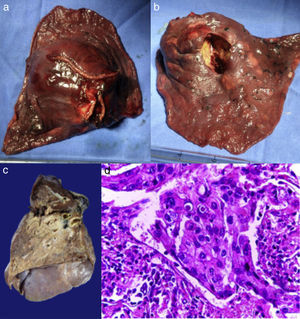
Resection surgery was performed (right lower lobectomy) with systematic mediastinal lymph node sampling by thoracic surgery assisted with hybrid video without complications (Figs. 4 and 5). An endopleural tube was placed that was removed on the second day after surgery and the patient was discharged to his home on the third day of hospitalization. A piece was sent to pathology with an adenosquamous carcinoma report (Fig. 5) with histological grade G2 (moderately differentiated) and nodular sampling with mixed hyperplasia without neoplastic cells.
Currently the patient has been taking part in follow-up visits in the outpatient clinic and only says in the first few weeks he had some pain that was easily mitigated with paracetamol 500mg every 6h and that he no longer takes analgesics. Follow-up has been performed with positron emission tomography and no image is observed with increased standardized uptake value of fluorodeoxyglucose. Follow-up is planned for 5 years.
DiscussionIn recent years, there have been great advances in all lung cancer-related matters.
Since the introduction of fibre optics in medicine in the 1960s and the description of the first laparoscopic cholecystectomy in the 1980s, there has been an extraordinary growth of minimally invasive surgery in many areas of clinical practice. Sadly, the implementation of these techniques in thoracic surgery has been much slower in the world, particularly in our country. Also, in oncology minimally invasive surgery is poorly developed at a global level, mainly due to the concern that it would jeopardize the principles of oncological surgery, such as: not resecting the entire tumour, leaving the tumour in the suture line or not being able to take biopsy of lymph nodes that allow for surgically staging.7
Video Assisted Thoracic Surgery (VATS) involves making a working incision of approximately 4cm (without separating the ribs) to introduce conventional surgery instruments through this opening and this is generally used for complex procedures. If costal separation is performed using a retractor is called hybrid Video Assisted Thoracic Surgery or Minimally Invasive Thoracic Surgery.8
It is important to stress that experts in minimally invasive surgery agree that the application of this type of approach requires trained personnel and a learning curve, enabling the development of centres of excellence for minimally invasive thoracic surgery procedures.9
Two meta-analyses claim that the VATS approach is equivalent to open surgery in terms of morbidity and mortality, with no differences in loco-regional recurrences; with an advantage in systemic recurrences and better 5-year survival demonstrating at least that the VATS approach is oncologically equivalent to open surgery.10,11
Although 70% of patients showed in advanced stages where they can no longer receive surgical treatment or treatment with the intent to cure (having an overall 5-year survival rate of 17%). Fortunately, the patient was diagnosed in early clinical stage IIB for T2b, N1, M0, being a candidate for resective surgery with mediastinal lymph node dissection or systematic lymph node sampling.
Because the patient did not have medical contraindications to surgery, it was decided to perform the procedure. We opted for a minimally invasive approach, seeking its virtues (less postsurgical pain, less time with endopleural probe in the postsurgical period, shorter hospital stay than with traditional open surgery, better pulmonary reserve in addition to equivalence in terms of oncological principles). The procedure was performed without complications and the patient experienced the benefits of a minimally invasive surgery.
In this specific case, we recognize that use of the telescope during lobectomy gave us a considerable improvement in terms of the view of the different anatomical, crucial structures during the procedure, such as the lobar artery and vein, bronchus and the incision itself (compared to open surgery). This resulted in increased security during placement of endoscopic staplers and cutting of the tissues, as well as contributing to decreasing surgical time.
Conclusions- •
Resective surgery through video-assisted thoracoscopic surgery is a feasible option for treating patients with lung cancer in early clinical stages.
- •
Minimally invasive thoracic surgery for lung cancer treatment has advantages over the open approach: less postsurgical pain, shorter hospital stay and better pulmonary reserve.
- •
Video-assisted thoracic surgery in lung cancer is at least equivalent to open surgery as far as oncological principles are concerned, since the lung parenchyma containing the tumour can be resected and systematic lymph node sampling can be performed.
- •
It is currently possible to perform procedures using the minimally invasive approach to treat lung cancer in the operating theatre of Pulmonology and thoracopulmonary surgery of Hospital General de México.
The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThere was no outside funding to complete this case study.
Conflict of interestThe authors declare that they have no conflict of interests.
We would like to thank Dr. César Athié Gutiérrez, General Director of Hospital General de México “Dr. Eduardo Liceaga”, as he provided us with the technology in order to carry out this type of procedure.