Pain in intensive care units is often underestimated, and therefore patients are insufficiently treated, leading to psychological, haemodynamic, metabolic and neuroendocrine responses that cause greater morbimortality. Pain can also cause anxiety, insomnia and disorientation, agitation and delirium, and depression that often times becomes chronic. Lack of or inadequate treatment increases pulmonary, metabolic and infectious complications. The combined use of analgesics and sedative agents decreases the stress response of patients in intensive care.
There are many other situations in intensive care units that make communication between the patient and healthcare personnel difficult (being sedated, the presence of an endotracheal tube, etc.), making it difficult to manage analgesia.
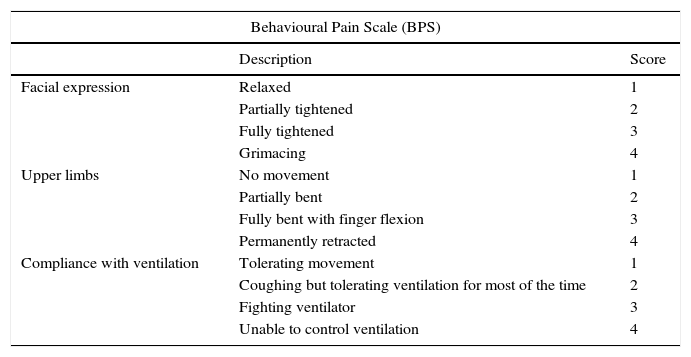
The BPS and the CPOT are the most validated and reliable behavioural scales to assess pain in adult patients in the ICU, when self-reporting is not possible.
Opioids are the cornerstone pain treatment in critically ill patients, however other classes of drugs are recommended to promote comfort and environmental tolerance, such as sedatives/hypnotics.
Specialised psychological services can provide improvements for both patients and family, especially in the prevention of anxiety and wasting syndrome.
In the spiritual dimension, the best method to alleviate pain is support for both the patient and the family.
El dolor en las unidades de cuidados intensivos es frecuentemente infravalorado, y por tanto los pacientes son insuficientemente tratados, conllevando a las respuestas psicológicas, hemodinámicas, metabólicas y neuroendocrinas que produce mayor morbimortalidad. El dolor puede provocar además de ansiedad, insomnio y desorientación, agitación y delirio, estados depresivos que en muchas ocasiones se vuelve crónico. La falta o inadecuado tratamiento incrementa complicaciones pulmonares, metabólicas e infecciosas. El uso combinado de agentes analgésicos y sedantes disminuye la respuesta al estrés de los pacientes de cuidados intensivos.
Existen muchas otras situaciones en las unidades de cuidados intensivos que generan dificultad para la comunicación entre el paciente y el personal de salud (estar sedado, la presencia de un tubo endotraqueal, etc.), generando cierta dificultad para el manejo de la analgesia.
El BPS y el CPOT son las escalas de comportamiento para evaluar el dolor en los pacientes adultos en la UCI más validadas y confiables, cuándo no es posible el autoreporte.
Los opioides son la piedra angular en el tratamiento de dolor en el paciente critico sin embargo se recomiendan otras clases de medicamentos para promover la comodidad y la tolerancia del medio como los sedantes-hipnóticos.
Los servicios psicológicos especializados pueden aportar mejorías tanto en pacientes como la familia sobre todo en la prevención de ansiedad y síndrome de desgaste.
En la dimensión espiritual el mejor método para paliar el dolor es el acompañamiento tanto para el paciente como para la familia.
The presence of pain and its effects negatively influence the complete experience of the critically ill patients and their healthcare context (Family-Healthcare team). Despite recognising that pain is a common stress factor,1 high rates of uncontrolled pain in critically ill patients remain and this increases morbimortality.2 This situation can be attributed, in part, to circumstances such as mechanical ventilation or being in a state of haemodynamic instability, which exclude self-reported pain assessments.3
Families contend with factors such as reorganisation, costs, and making decisions at different times over the course of the critical situation. The healthcare team often confronts the patient's inability to communicate by self-reporting. The particular social, cultural, political, and education situation can make it easier or harder for the patient to emphasise the symptom-syndrome, therefore a comprehensive view (biological, psychological, social, and spiritual) regarding the diagnostic and treatment approach becomes mandatory if seen based on current scientific information and its bioethical implications.
The spiritual approach for critically ill patients and their context must be adjusted taking into account the situation built around a physical body, family, and emotional relationships with others, with themselves, with their depths or their being, in a certain setting and culture, a specific time, and based on circumstances and experiences to which they respond. In this way they structure their way of being in life and their history may, or may not, be guided through a belief or religion.
The threat to the identity they established over the course of their lives and the hopes, unease, suspicions, diagnosis, symptoms, treatments, fear, shame, isolation, dependence, and lack of control are a source of suffering. This can be expressed in many ways: anxiety, anger, and depression, among others. Critically ill patients frequently confront suffering, defined by E. Cassel (in Barbero, 2008) as “a state of severe distress associated with events that threaten the intactness of the person and continues until the threat has passed or until the integrity of the person can be restored”. The objective of the spiritual approach is to promote healing defined in terms of developing a personal sense of full physical, mental, emotional, and social aspects of the human experience.4
AssessmentAccording to the expert guidelines, the presence of pain should be assumed in uncommunicative critically ill patients,5–7 and it should be systematically analysed as the fifth vital sign.8 Despite strong evidence that indicates that documenting the assessment of pain improves its management and decreases its intensity, no assessment instrument has been universally recommended for self-reporting critically ill patients (considered the gold standard in assessing pain),9 therefore the one that is best suited to the patients should be used.9–11
The physiological indicators alone are losing more and more significance, since they do not offer good sensitivity and/or specificity for diagnosing the presence and intensity of pain.
Adequately treating pain and anxiety is associated with a decrease in the duration of mechanical ventilation (8 vs 11 days, p<0.01),12 a decrease in the rate of nosocomial infections,13 and an increase in patient-satisfaction.14 Furthermore, systematically assessing pain can decrease the duration of stay in the ICU (13 vs 18 days, p<0.01).13
The Joint Commission on Accreditation of Health care Organizations (JCAHO), the Agency for Health Care Policy Research (AHCPR), the International Association for the Study of Pain (IASP), and the Spanish Society of Intensive Medicine and Coronary Care Units (SEMICYUC), are some of the international commissions that recommend behavioural scales to make it easier for professionals to manage pain.
Professional organisations, such as the American Association of Critical Care Nurses, American College of Chest Physicians, the Society of Critical Care Medicine, the American Society for Pain Management, and the Agency for Health Care Policy and Research (AHCPR) back using standardised pain assessment instruments, including behavioural indicators (Behavioural Pain Scale – BPS – developed by Payen et al., Critical-Care Pain Observation Tool (CPOT) by Gélinas), in patients who are sedated or on mechanical ventilation and therefore incapable or self-reporting or whose self-reporting may be unreliable (Table 1).15–17
Behavioural Pain Scale (BPS).
| Behavioural Pain Scale (BPS) | ||
|---|---|---|
| Description | Score | |
| Facial expression | Relaxed | 1 |
| Partially tightened | 2 | |
| Fully tightened | 3 | |
| Grimacing | 4 | |
| Upper limbs | No movement | 1 |
| Partially bent | 2 | |
| Fully bent with finger flexion | 3 | |
| Permanently retracted | 4 | |
| Compliance with ventilation | Tolerating movement | 1 |
| Coughing but tolerating ventilation for most of the time | 2 | |
| Fighting ventilator | 3 | |
| Unable to control ventilation | 4 | |
Pain grade: presence of pain ≥6/unacceptable pain >7/objective <6.
The BPS and CPOT are the most validated and reliable behavioural scales for monitoring pain in adult patients in the medical, surgical, and trauma ICU (except brain damage), whenever motor function is intact and their behaviour can be observed.18
Attempts to validate the instruments as a method to assess the severity of the pain have not been successful. Moreover, these scales have not been extrapolated in other populations outside the ICU and they have also not been validated for languages other than French and English.
The Behavioural Indicators of Pain Scale (Escala de Conductas Indicadores de Dolor, ESCID) has been demonstrated to be the most objective at assessing pain when procedures are being performed: bronchial secretion aspiration, turning, and treatments in non-communicative patients with severe trauma and mechanical ventilation.
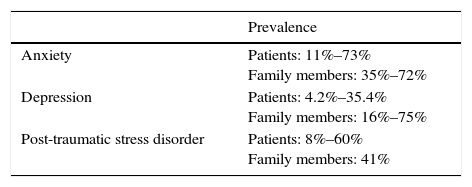
The most used and validated instructions for assessing emotional symptoms in critically ill patients include: Hospital Anxiety and Depression Scale (HADS), which assesses anxiety and depression without taking somatic symptoms into account, so it is easy to use among patients with these symptoms; the Impact of Event Scale-Revised (IES-R), which assess symptoms related to Post-Traumatic Stress Disorder; and the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU), which assesses symptoms of delirium (Table 2).
A systematic review of the psychological assessment scales used in the ICU is needed, therefore it is important to use them with caution since they are not diagnostic instruments, and as a result may overestimate the prevalence. To make a diagnosis, an interview and detailed knowledge of the instrument and the professional clinical-ethical considerations are required.
An updated discussion about the development, validation, and applicability of behavioural pain assessment tools in ICU patients is needed,19 as with the psychological evaluation scales.
To conduct a spiritual assessment, a classification taken from Barbero et al. is presented4 where some of the spiritual needs that may serve as a basis for this are mentioned:
Being recognised as a person: As healthcare resources and processes become more technical, separating patients from the decisions concerning them, a lack of family support, and a dehumanising work environment can relegate the patients to anonymity, losing their identity of who they are. This need is considered essential.
The search for meaning: Awareness of one's own mortality awakens the need to find a meaning and purpose for existence and makes a person realise what is essential. What is important is not the meaning of life in general terms, but rather that the specific meaning of each individual's life at a given time will lead some people to a difficult, but creative process with renouncements and compromises.
Need for continuity: Patients frequently intensify their relationship with the past, present, and future. As regards the past, there is a need to review one's own life and make peace with it. In the present, being ill often causes a confrontation by bring a new hierarchy of values into consideration. Regarding the future, the time may be lived as a frustration, but it can also be open to the transcendent.
Need for hope: P. Barreto mentions that hope work is possible in the present based on the concept of “expanding hope”, in which very short-term operational goals can be set that satisfy what the patient can live at that time as an authentic quality of life. According to Perakyla, the conversational activity identified as hope work has variants: In curative hope work the patient is defined as “getting better”; in palliative hope work, the patient is defined as “feeling better”. For Havel, hope is not the conviction that something will turn out well, but the certainty that something makes sense, regardless of how it turns out.
Need to express feelings and experiences: This need occurs in all cultures. Many people, regardless of their religion, have a specific way of expressing them.
Healthcare staff require an attitude of detection, patience, and exploration. An active attitude regarding the spiritual dimension tends to be undervalued. It is important to note that the goal is to not only reduce spiritual discomfort, but also to promote well-being. The early detection of spiritual needs and resources enables creating a preventative dynamic, even if initially there was no express request for accompaniment.
To structure the spiritual exploration according to specificity, it can be classified according to the following levels:
General level: At this level the patients’ mood and worries are explored as well as their degree of difficulty in confronting them; their experience of discomfort or suffering, the support resources and the expectations about the level of help that can be provided.
Intermediate level: Resources and/or ideas are explored that help to live through the process; presence of certain questions that express unresolved needs and the degree of influence these questions have on the process; level or satisfaction or dissatisfaction regarding life and expectations or desires in the current situation.
Specific level: The spiritual and/or religious world, the potential benefits, the desire to delve into everything, and the need to seek another spokesperson.4
TreatmentPatients in pain will appear to be agitated and anxious. This puts them at risk of self-extubation and catheter and tube removal. They will adapt poorly to the ventilator (asynchrony), which has repercussions on their haemodynamic condition.20
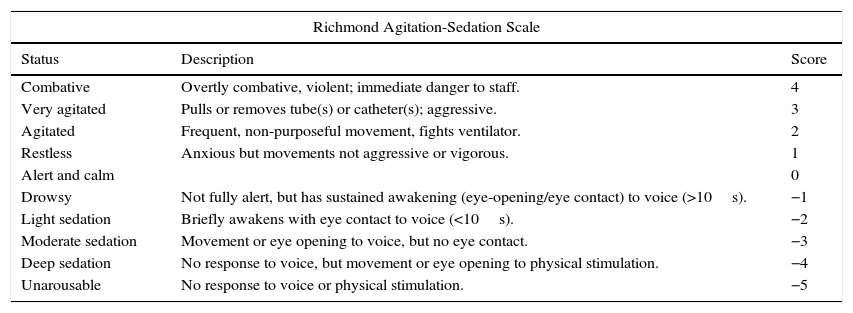
The Richmond Agitation-Sedation Scale (RASS) has been validated for critically ill patients (Table 3).21
Richmond Agitation-Sedation Scale (RASS) modified from “Monitoring sedation status over time in ICU Patients”.
| Richmond Agitation-Sedation Scale | ||
|---|---|---|
| Status | Description | Score |
| Combative | Overtly combative, violent; immediate danger to staff. | 4 |
| Very agitated | Pulls or removes tube(s) or catheter(s); aggressive. | 3 |
| Agitated | Frequent, non-purposeful movement, fights ventilator. | 2 |
| Restless | Anxious but movements not aggressive or vigorous. | 1 |
| Alert and calm | 0 | |
| Drowsy | Not fully alert, but has sustained awakening (eye-opening/eye contact) to voice (>10s). | −1 |
| Light sedation | Briefly awakens with eye contact to voice (<10s). | −2 |
| Moderate sedation | Movement or eye opening to voice, but no eye contact. | −3 |
| Deep sedation | No response to voice, but movement or eye opening to physical stimulation. | −4 |
| Unarousable | No response to voice or physical stimulation. | −5 |
The two main drug classes to promote comfort and tolerance of the setting in critically ill patients are sedative-hypnotic agents and analgesics. The literature recommends alpha-2-andrenergic agonists (Dexmedetomidine) or benzodiazepines (Midazolam).
Something extremely important discussed at the 5th Consensus Conference in Critical Care held in Brussels in 2003 is the following: “The patient must be given sufficient analgesia to alleviate pain and distress; if such analgesia hastens death, this “double effect” should not detract from the primary aim to assure comfort”.22
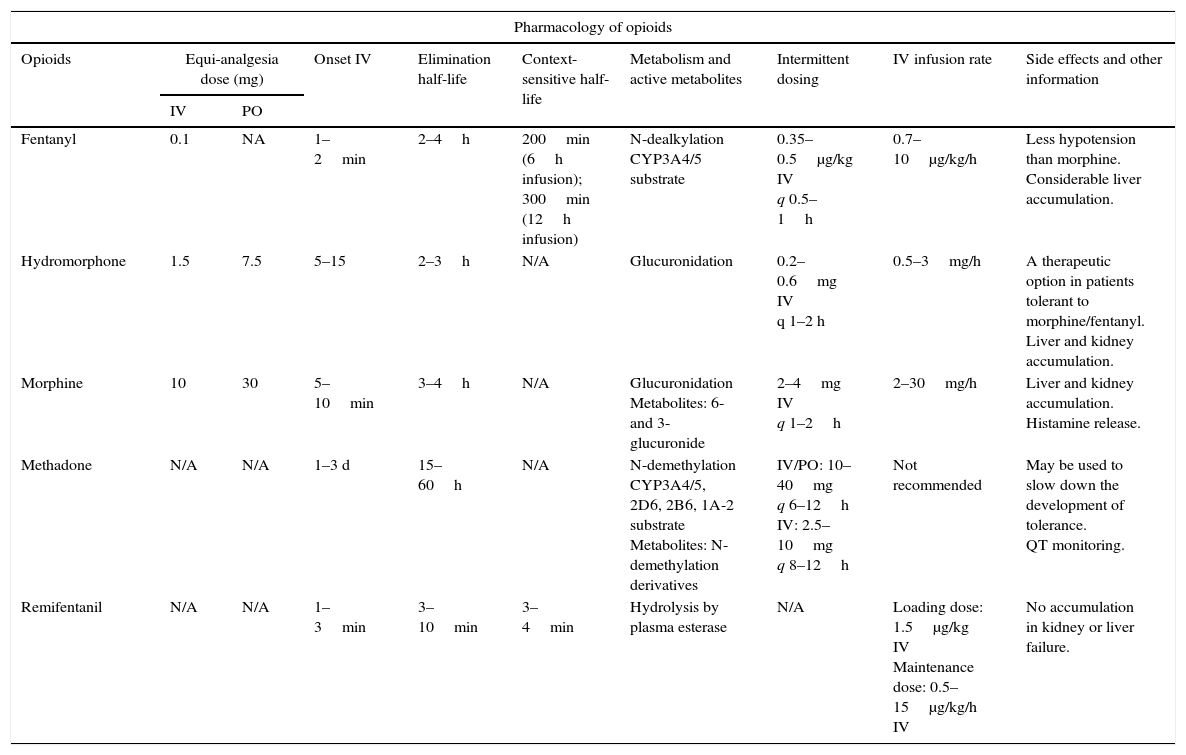
Opioids are the analgesics of choice; however, the American Society of Health-System Pharmacists (ASHP) also recommends the use of non-steroidal anti-inflammatory drugs (NSAIDs) and paracetamol.
The opioid of choice is fentanyl, which is highly soluble in lipids with a quick onset of action (1min). It is rapidly distributed to peripheral tissues, resulting in a short half-life (0.5–1h) after a single dose due to low renal and hepatic interference.
Morphine is an opioid analgesic that can be used in critically ill patients, although it has low solubility in lipids and has a relatively slow onset of action (5–10min). It is excreted through the kidneys, so it is a poor choice for patients with kidney failure.
Agonist–antagonist analgesics, such as nalbuphine, butorphanol, and buprenorphine, can cause withdrawal symptom and prolonged use should be avoided.23Table 4 shows different opioid drugs for use in critically ill patients.
Pharmacology of opioids.
| Pharmacology of opioids | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Opioids | Equi-analgesia dose (mg) | Onset IV | Elimination half-life | Context-sensitive half-life | Metabolism and active metabolites | Intermittent dosing | IV infusion rate | Side effects and other information | |
| IV | PO | ||||||||
| Fentanyl | 0.1 | NA | 1–2min | 2–4h | 200min (6h infusion); 300min (12h infusion) | N-dealkylation CYP3A4/5 substrate | 0.35–0.5μg/kg IV q 0.5–1h | 0.7–10μg/kg/h | Less hypotension than morphine. Considerable liver accumulation. |
| Hydromorphone | 1.5 | 7.5 | 5–15 | 2–3h | N/A | Glucuronidation | 0.2–0.6mg IV q 1–2 h | 0.5–3mg/h | A therapeutic option in patients tolerant to morphine/fentanyl. Liver and kidney accumulation. |
| Morphine | 10 | 30 | 5–10min | 3–4h | N/A | Glucuronidation Metabolites: 6- and 3-glucuronide | 2–4mg IV q 1–2h | 2–30mg/h | Liver and kidney accumulation. Histamine release. |
| Methadone | N/A | N/A | 1–3 d | 15–60h | N/A | N-demethylation CYP3A4/5, 2D6, 2B6, 1A-2 substrate Metabolites: N-demethylation derivatives | IV/PO: 10–40mg q 6–12h IV: 2.5–10mg q 8–12h | Not recommended | May be used to slow down the development of tolerance. QT monitoring. |
| Remifentanil | N/A | N/A | 1–3min | 3–10min | 3–4min | Hydrolysis by plasma esterase | N/A | Loading dose: 1.5μg/kg IV Maintenance dose: 0.5–15μg/kg/h IV | No accumulation in kidney or liver failure. |
Another category includes NSAIDs, which provide analgesia through non-selective and competitive cyclooxygenase (COX) inhibition, although they can still cause significant adverse effects in patients with hypovolaemia or hypoperfusion, in addition to probable side effects such as gastropathy, nephrotoxicity, and thrombogenicity. Senile patients and those with pre-existing kidney failure may be more susceptible to NSAID-induced injury.23
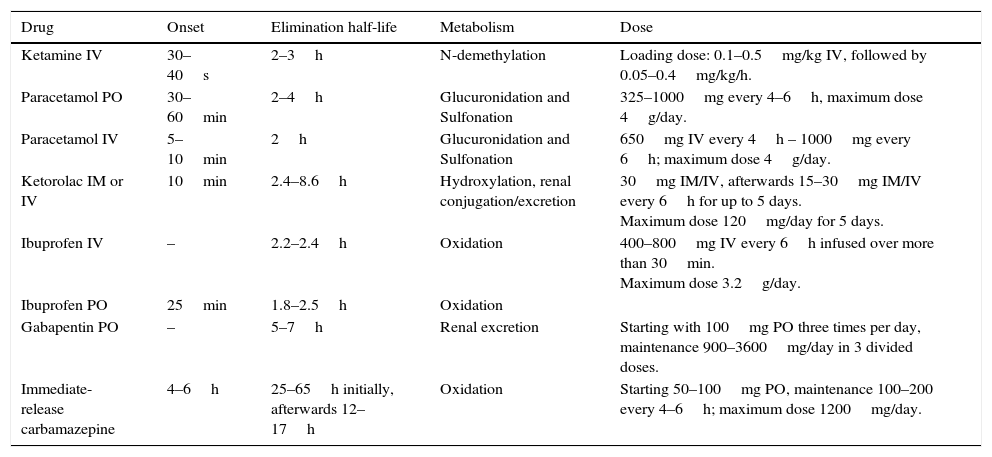
In 2007, SEMICYUC issued strong recommendations to not use these drugs in this population, with a 1C evidence level. The Society of Critical Care Medicine (SCCM) mentions their use only as opioid potentiators due to their adverse effects.23Table 5 presents different pharmacological characteristics of non-opioid analgesics.
Pharmacological characteristics of non-opioid analgesics.
| Drug | Onset | Elimination half-life | Metabolism | Dose |
|---|---|---|---|---|
| Ketamine IV | 30–40s | 2–3h | N-demethylation | Loading dose: 0.1–0.5mg/kg IV, followed by 0.05–0.4mg/kg/h. |
| Paracetamol PO | 30–60min | 2–4h | Glucuronidation and Sulfonation | 325–1000mg every 4–6h, maximum dose 4g/day. |
| Paracetamol IV | 5–10min | 2h | Glucuronidation and Sulfonation | 650mg IV every 4h – 1000mg every 6h; maximum dose 4g/day. |
| Ketorolac IM or IV | 10min | 2.4–8.6h | Hydroxylation, renal conjugation/excretion | 30mg IM/IV, afterwards 15–30mg IM/IV every 6h for up to 5 days. Maximum dose 120mg/day for 5 days. |
| Ibuprofen IV | – | 2.2–2.4h | Oxidation | 400–800mg IV every 6h infused over more than 30min. Maximum dose 3.2g/day. |
| Ibuprofen PO | 25min | 1.8–2.5h | Oxidation | |
| Gabapentin PO | – | 5–7h | Renal excretion | Starting with 100mg PO three times per day, maintenance 900–3600mg/day in 3 divided doses. |
| Immediate-release carbamazepine | 4–6h | 25–65h initially, afterwards 12–17h | Oxidation | Starting 50–100mg PO, maintenance 100–200 every 4–6h; maximum dose 1200mg/day. |
Administering NSAIDs can reduce the need for opioids, although the analgesic benefit has not been systematically studied in critically ill patients. Paracetamol has been used to treat mild or moderate pain in combination with an opioid producing a synergistic effect. The role of paracetamol as a monotherapy in the intensive care unit is limited to relieving mild pain, such as that associated with prolonged bed rest or as an antipyretic.
Analgesia and sedation are frequently indicated empirically with an inadequate choice of drug and dosage. Pain assessment depends on the ability to communicate, and most times the doctor does not know how to identify the presence of this sensation. Therefore we emphasise the recommended scales to determine the presence of pain, such as the Behavioural Pain Scale (BPS), validated in critically ill patients.24
Several studies suggest that attention should first be focused on providing analgesia before anxiolysis, since this may provide greater comfort and a shorter duration of conditions such as mechanical ventilation or delirium.25
In 2013 the Society of Critical Care Medicine (SCCM)23 issued recommendations that can serve as important guidelines for managing pain in critically ill patients.
Among these, we can point out:
- 1.
Pre-emptive analgesia and/or non-pharmacologic interventions (e.g. relaxation) to alleviate pain in ICU patients prior to chest tube removal. Recommended (1C)
- 2.
For invasive and potentially painful procedures in adult ICU patients, pre-emptive and/or non-pharmacologic interventions may also be administered to alleviate pain. Weakly recommended (2C)
- 3.
Intravenous opioids should be considered as the first-line drug of choice to treat non-neuropathic pain in critically ill patients. Recommended (1C)
- 4.
All available IV opioids, when titrated to similar pain intensity endpoints, are equally effective. Weakly recommended (2C)
- 5.
Gabapentin or carbamazepine should be administered in addition to an IV opioid to treat neuropathic pain. Strongly recommended (1A)
- 6.
Non-opioid analgesics should be considered to decrease the amount of opioids administered (or to eliminate the need for IV opioids) and to decrease opioid-related side effects. Weakly recommended (2C)
- 7.
Thoracic epidural anaesthesia/analgesia may be considered for postoperative analgesia in patients undergoing abdominal aortic aneurysm surgery. Strongly recommended (1B)
- 8.
Thoracic epidural analgesia may be considered for patients with traumatic rib fractures. Weakly recommended (2B)
- 9.
Neuroaxial/regional analgesia over systemic analgesia in medical ICU patients may not be recommended, due to lack of evidence in this patient population. There are no articles justifying it. No recommendation (0)
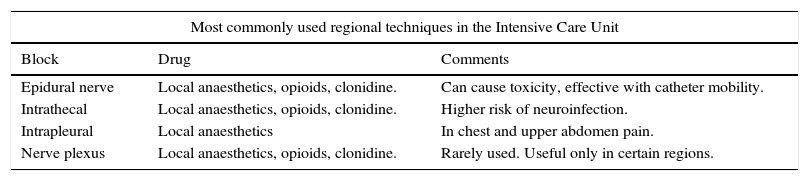
Regional techniques have been used in the ICU. The most common are discussed in Table 6.
Most commonly used regional techniques in the ICU.
| Most commonly used regional techniques in the Intensive Care Unit | ||
|---|---|---|
| Block | Drug | Comments |
| Epidural nerve | Local anaesthetics, opioids, clonidine. | Can cause toxicity, effective with catheter mobility. |
| Intrathecal | Local anaesthetics, opioids, clonidine. | Higher risk of neuroinfection. |
| Intrapleural | Local anaesthetics | In chest and upper abdomen pain. |
| Nerve plexus | Local anaesthetics, opioids, clonidine. | Rarely used. Useful only in certain regions. |
Contrary to what is recommended in non-surgical critically ill patients, there are articles that do recommend regional or neuroaxial analgesia modalities (spinal or epidural) for postoperative analgesia after select surgical procedures.26
Therefore, after reviewing the above, it would be unforgiveable to not recall that “Most critically ill patients experience pain at some time during their stay in the ICU, identifying it as a great source of stress”.27–29
The International Association for the Study of Pain also affirms that “inability to communicate verbally does not negate the possibility that an individual is experiencing pain and is in need of appropriate pain-relieving treatment”.30 And it is striking that these patients have identified pain as their major concern and the main cause of lack of sleep.31
The optimal choice of opioid and dosing regimen used for an individual patient depends on many factors, including pharmacokinetics and pharmacodynamics.27
Regarding neuropathic pain, which is poorly relieved with pure mu-opioid agonists, patients should be treated with tramadol, due to the combination between the mu effect and its inhibitory effect on serotonin and norepinephrine reuptake. It should always be kept in mind that there is a ceiling effect at 400mg within 24h in adults and 600mg for cancer patients. Furthermore, it should not be forgotten that ICU patients with sufficient gastrointestinal absorption and motility can be treated with enteral gabapentin and carbamazepine.32,33
The strategic choice between bolus vs continuous IV administration of drugs in critically ill patients depends on the pharmacokinetics of the drug, the frequency and intensity of pain, and/or the patient's mental status.34
Additional non-pharmacologic interventions to treat pain, such as music therapy and relaxation, have been demonstrated in some articles to reduce opioid use; to be low cost, safe and easy to provide; and to be beneficial for the treatment of depression and/or delirium.27,35
The National Institute for Health and Care Excellence (United Kingdom) has issued a series of treatment guidelines for anxiety, depression, and post-traumatic stress disorder supporting the use of cognitive behavioural therapy (CBT) and eye movement desensitisation and reprocessing (EMDR). Their combined use makes most patients asymptomatic by the end of therapy, with most reporting feeling much better.11 They can thus return to their normal activities and commit to on-going medical treatment when necessary for chronic health conditions.36
Peris et al.21 report that early, intra-ICU psychological intervention can help critical trauma patients to recover from the stressful experience. The care is based on emotional support, training on coping strategies, educational interventions, counselling, bedside stress management, and cognitive-emotional restructuring to reduce the discomfort caused by the health conditions and medical procedures. The interventions were also designed to help family members, starting during the phase while the patient was still unconscious, by promoting family-focused decision making and supporting family members to choose appropriate interactions during their visits. The probability of a PTSD (Post-Traumatic Stress Disorder) diagnosis was significantly lower in the psychological intervention group versus the control group (without psychotherapy). The number of patients who used anxiolytic and antidepressant drug therapy at discharge was significant higher in the group without a psychological intervention.
Ullman et al.37 performed a systematic review in collaboration with Cochrane on intensive care diaries used in several countries as a tool to improve the memory of acts in the ICU, with the goal of improving recovery from critical illness in patients at discharge. It was concluded that to date there is minimal evidence from randomised controlled trials on the benefits or harms from the use of diaries for patients and family members.
Specialised psychological services during critical illness are not generally available worldwide. Studies on psychological support interventions in the ICU are very scarce and have methodological limitations that require more scientific research in this area. There are focuses on psychology that could support tools for both assessment and treatment in this context that have not been fully integrated in the literature to date.
Regarding the spiritual dimension, the treatment method is based on accompaniment. To specifically confront the spiritual needs, the professionals need to have done the work of confronting their own losses, developing in themselves a conscience sensitive to the needs of this dimension.
The companion must have some necessary attitudes such as hospitality, decisiveness, and a stand for creating links of trust with a certain vocation of continuity and permanence, prudence, and interdisciplinary teamwork.
The companion needs to know the methodological itineraries necessary for a specific, in-depth intervention. These are:
Detection: This is related to classifying the spiritual needs that are the responsibility and duty of all team members, therefore common, homogeneous training procedures are required to adequately achieve this goal of detecting spiritual needs and resources in the person.
Exploration: The way to explore must be cautious and not iatrogenic. It is possible that at a certain time they decide to not go in-depth, but at least known that if at any time they wish to discuss these questions, they have the staff to do so. This does not involve using a questionnaire, but rather enabling them to get closer to the spiritual world in a natural and non-threatening manner, without distress, respecting the pace of the person being accompanied. The exploration already has therapeutic content and involves a potential intervention.
Intervention: Once the patient has explored and reached a suitable balance of threats and opportunities, needs and resources, there can be an intervention on those that cause the most concern, within the spiritual area, or on those aspects that seem timely for promoting a preventative intervention or developing unexpressed or updated potential.4
One of the objectives of the intervention is to creating a humanising relationship, from a so-called “deliberative” relationship model, where the staff member relates with the other person trying to establish the clinical and technical aspects, as well as emotions and values. This relationship model requires the staff member to have training in bioethics and deliberative communications, and it requires personal introspection and self-awareness along with a compassionate attitude, based on awareness of the pertinence of a goal, but also on the search for tools that enable effectiveness and efficiency in approaching the spiritual needs of patients, family members, and the healthcare team.18
DiscussionPain in critically ill patients can have different origins, spanning the condition itself that motivated their admission to the techniques and the care necessary to manage it.
The implementation of analgesia and sedation protocols has been demonstrated to reduce in time the duration of mechanical ventilation (AMV), the duration of stay in the Intensive Care Unit (ICU),12,13 associated nosocomial infections, and the incidence of episodes of pain and agitation. It is important to assess in some way whether the pain suppression sought with analgesic treatment has been satisfactorily achieved.
As pain is predominantly subjective, if the patient's state permits, obtaining their perception of it should be tried. Using a behavioural assessment such as the CPOT or BPS is recommended.15–17 Furthermore, the assessment can be supplemented by observing the physiological equivalents of pain. Although observing these indicators, such as variation in heart rate, blood pressure, and tachypnoea may be related to pain, their use in critically ill patients is very limited since they can be affected by the condition itself or the use of drugs that directly influence these values.
For medical treatment, it is recommended to start with opioid analgesics22,23 and continue increasing the plasma concentration of the drug until reaching the desired analgesia goal. This approach focuses on prioritising analgesia before sedation24 (analgosedation or analgesia first).
As for PTSD, integrating family through psychotherapy decreases the incidence, helping to identify symptoms such as anxiety and depression for timely treatment.21
Specialised psychological services can provide improvements for the patients, family, and the medical team.
In the spiritual dimension, the best method to alleviate pain is support for both the patient and the family.
ConclusionsCurrently, decreases in the physical, psychological, and spiritual sequelae at the time of discharge from the ICU are sought. One strategy to achieve this goal is to implement a pain assessment and treatment protocol, since a patient without this symptom will require less sedation, be less predisposed to develop delirium, and will have easier active or assisted mobility. Moreover, an adequate level of analgesia along with a lower level of sedation in select patients will enable a better adjustment to mechanical ventilation, faster weaning, fewer days on mechanical ventilation, and fewer days in the ICU.
The family-healthcare team, by being an entity related to the critically ill patient, should watch for pain, and treat it if necessary; thus preventing wasting syndrome and a lack of emotional adjustment.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.