Mucosa-associated lymphoid tissue (MALT) represents 8% of non-Hodgkin lymphomas (NHL), with 2% affecting the conjunctiva. The case is presented of a 19-year-old patient diagnosed with conjunctival MALT lymphoma of the right eye, treated with external radiotherapy (ERT), and showing a complete, 100% response. At 18 months, no signs of relapse.
The treatment of choice for MALT type extranodal lymphoma is ERT. It has shown excellent results in controlling the disease, overall survival, progression-free survival and relapse-free survival. The relapse rate is 6–27% and the transformation to a higher grade lymphoma between 18% and 23%, consequently patients must have adequate follow-up. If the above is confirmed, reirradiation, chemotherapy and/or molecular target-directed therapy should be considered.
El linfoma asociado a tejido mucoso (MALT) representa el 8% de los Linfomas No Hodgkin (LNH), afectando a la conjuntiva en el 2%. Se presenta el caso de paciente de 19 años de edad diagnosticada con linfoma MALT en conjuntiva de ojo derecho, tratada con radioterapia externa (RTE), mostrando respuesta completa del 100%. A 18 meses de seguimiento, sin datos de recaída.
El tratamiento del elección en linfoma MALT extraganglionar es con RTE, ha demostrado excelentes resultados en control de la enfermedad, sobrevida global, sobrevida libre de progresión y sobrevida libre de recaída. La recaída es del 6–27% y la trasformación a un linfoma de mayor grado ente 18–23%; motivo por el cual los pacientes deben tener un adecuado seguimiento, en caso de confirmarse lo anterior se deberá considerar re-irradiación, quimioterapia y/o terapia dirigida a blanco molecular.
NHL was first described in 1983 by Isaacson and Wright.1 It has an incidence of 4.3% and a mortality rate of 3.2% according to the surveillance, epidemiology, and end results program (SEER) statistics.2 In the United States it occupies fifth place in terms of incidence in both men and women, and ninth place in terms of mortality.3,4 More frequently among women, with an incidence peak at between 50 and 70 years of age.5
The presentation of mucosa-associated lymphoid tissue (MALT) in conjunctiva represents approximately 2–8% of cases.5–7 The most frequent location being the palpebral conjunctiva (64–70%), lacrimal gland (18%) and less frequently retrobulbar tissue or extraocular muscles.6,8,9
Some infectious agents are involved in the aetiology of MALT lymphomas, such as Chlamydia psittaci, Hepatitis B Virus and Chlamydia pneumoniae. This varies according to geographical region. In Europe, it presents at a rate of 87%, however, this association has not been clearly observed in America,6,10,11 given the above and based on the results of a meta-analysis it was concluded that the association between chronic C. psittaci infection and the development of orbital MALT lymphoma varies considerably.8 Furthermore, it is related to autoimmune processes such as thyroiditis and Sjögren's syndrome, increasing the relative risk to 70 and 40 times respectively among the general population.8,9,12
The form of presentation is indolent, it is characterised by frequent relapses that may transform into a diffuse large-B-cell lymphoma.13,14
In the majority of patients it presents unilaterally, although it presents bilaterally in 15% of cases.15–17
The diagnosis of orbital MALT lymphomas is based on the analysis of morphology, immunophenotype and genetic analysis of the biopsy material.
Histopathologically it is characterised by a heterogeneous morphology with irregular nuclei. Plasmacytoid cells with intranuclear pseudoinclusions of immunoglobulin may present, which are also known as Dutcher bodies, or acidophil spheres in the cytoplasm or Russell bodies may present.2,18,19
The immunohistochemical panel includes positivity for CD19, CD20 (more common), CD79a, CD53, CD2112 and over-expression of BCL2 Figures 1–5.
For the genetic analysis, studies such as fluorescent in situ hybridisation (FISH) are useful for determining translocations t(11;18), t(11;14), t(3;14). Of these, t(11;18) produces genetically stable MALT lymphomas, which do not transform into B lymphocyte lymphomas.12,18–20
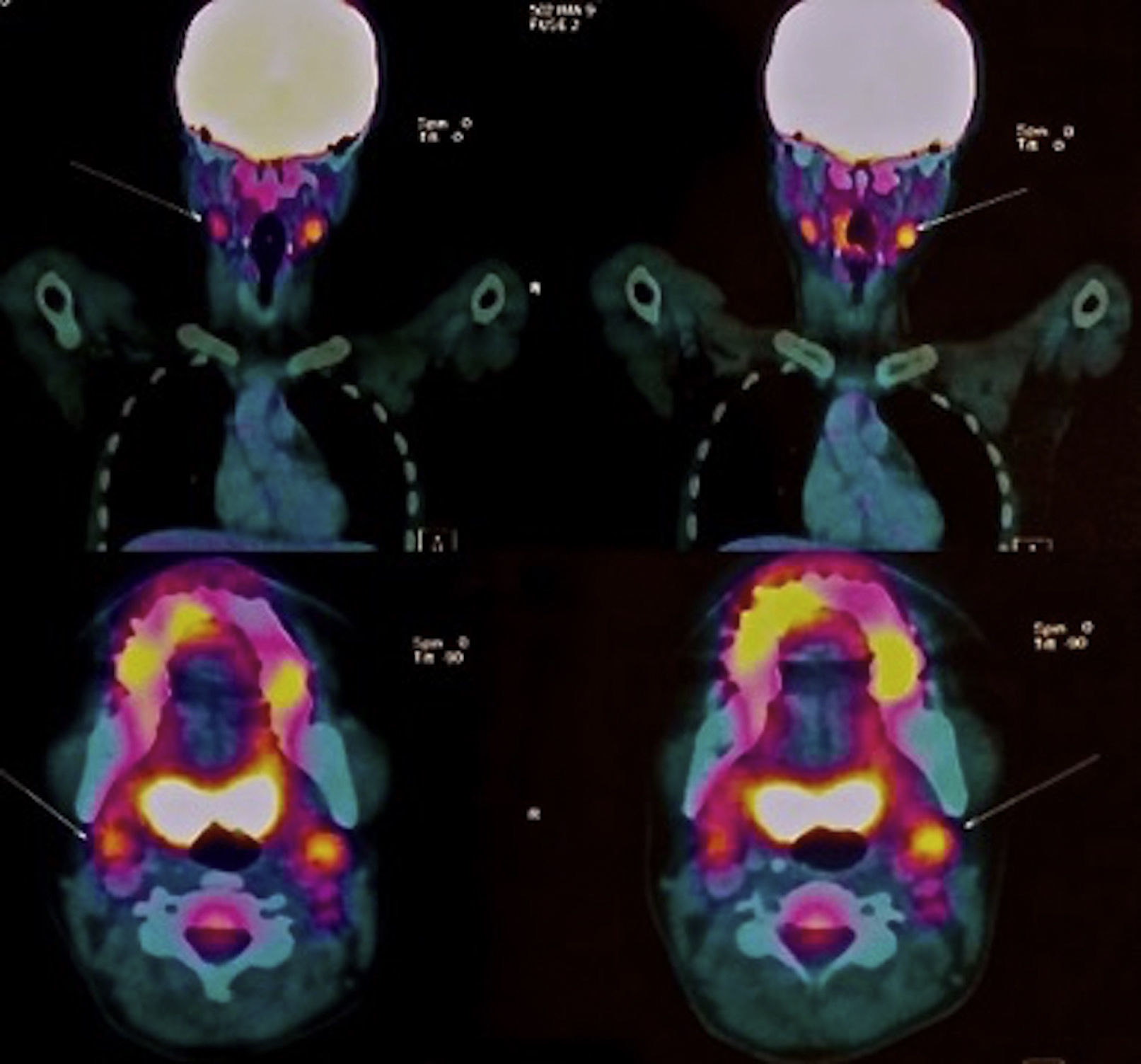
PET-CT is an imaging technique being increasingly used. This is performed with the radiotracer 18 FDG (fluorodeoxyglucose) to determine pathological progression, which can be present in up to 73% of cases in orbital or conjunctival sites.21 Other imaging techniques such as magnetic resonance do not have greater diagnostic precision.3,14,17
One of the most recent studies of orbital MALT lymphoma is DNA methylation. It has been demonstrated that a differentiated methylation exists between the different genes with respect to the C. psittaci infection status and the response to doxycycline, with IRAK1 and CXCR6 being the most associated genes.22
The treatment options are surgery, ERT, chemotherapy (CT) alone or concomitantly and molecular target-directed therapy.
ERT is indicated where response to antibiotics is poor or null, the dose studied is in the range of 25–36Gy with electrons or photons, giving good results in controlling the disease, overall survival and relapse-free survival.
The indications for CT or targeted therapy with anti CD-20 monoclonal antibodies (rituximab) are patients with a marked symptomatic disease or systemic disease with pulmonary and/or hepatic invasion.
Patients who present transformation to a high grade lymphoma (diffuse large-B-cell lymphoma), are candidates for treatment with rituximab-cyclophosphamide, doxorubicin, vincristine, prednisone (R-CHOP).23–25
Case reportFemale patient, 19 years of age, originating from Estado de México, student, negative background for cancer or autoimmune disease susceptible genetic profile, no surgery, chronic-degenerative or trauma history.
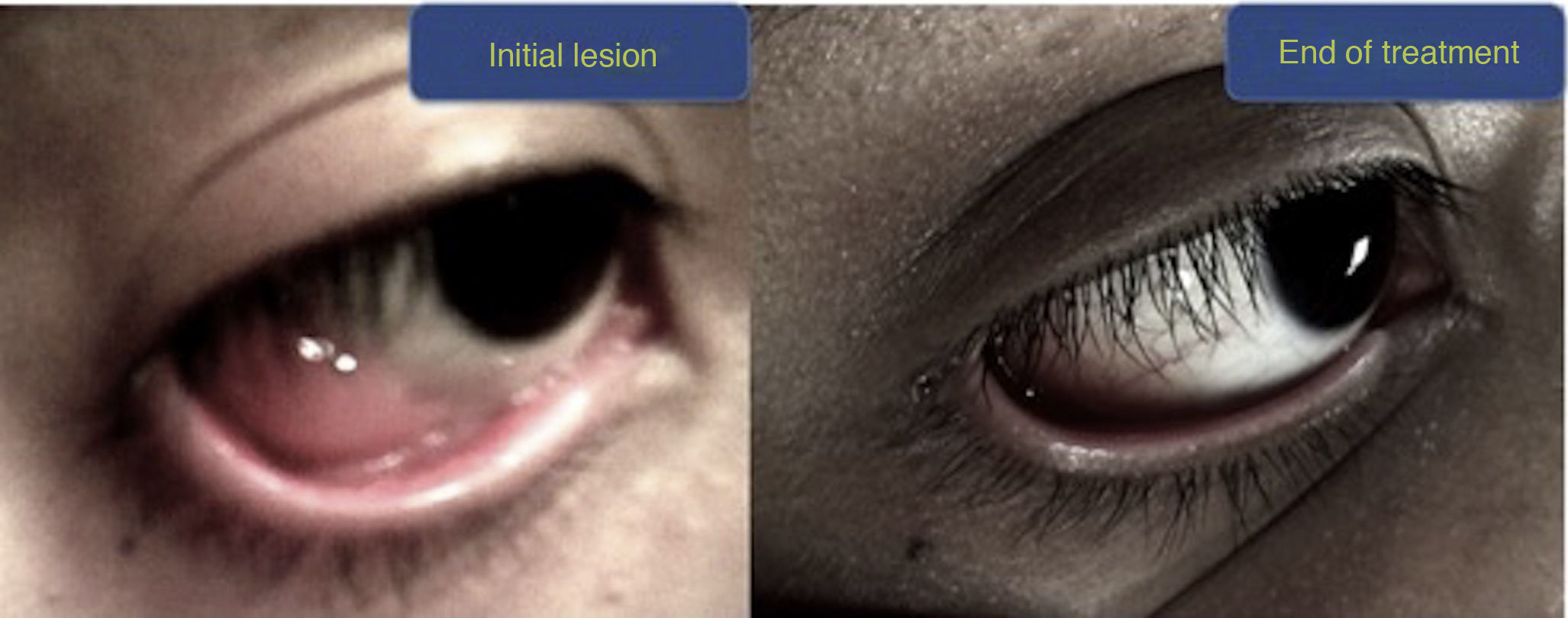
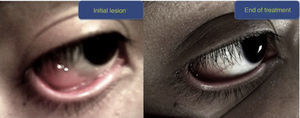
The patient's symptoms commenced 4 months before the physician's assessment, with the presentation of a tumour in the right lower eyelid of less than 1cm, accompanied by asthenia, adynamia, general deterioration, with no weight loss, euthermic. The patient consulted the ophthalmologist who performed an excisional biopsy, resulting in the histopathological report of marginal zone B lymphoma associated with MALT mucosa.
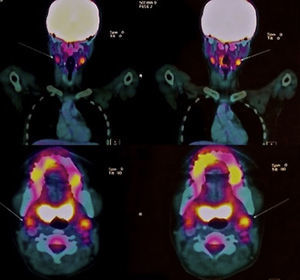
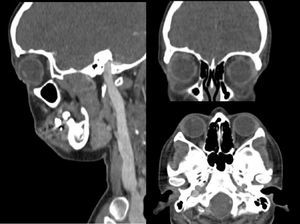
The immunohistochemical panel was positive for CD20, BCL2 and Lambda chain and negative for CD5, CD43 and Kappa chain. The viral panel was negative for cytomegalovirus (CMV), hepatitis B virus (HBV), hepatitis C virus (HCV), human immunodeficiency virus (HIV); bone biopsy without infiltration. Initial FDG PET/CT with evidence of level IIA bilateral cervical ganglia, of up to 11mm on its short axis, SUVmax 3.37 of higher metabolic activity on the left side. Ocular structures with no evidence of morphological or metabolic lesions.
Consequently, the case was managed in conjunction with the Haematology Department.
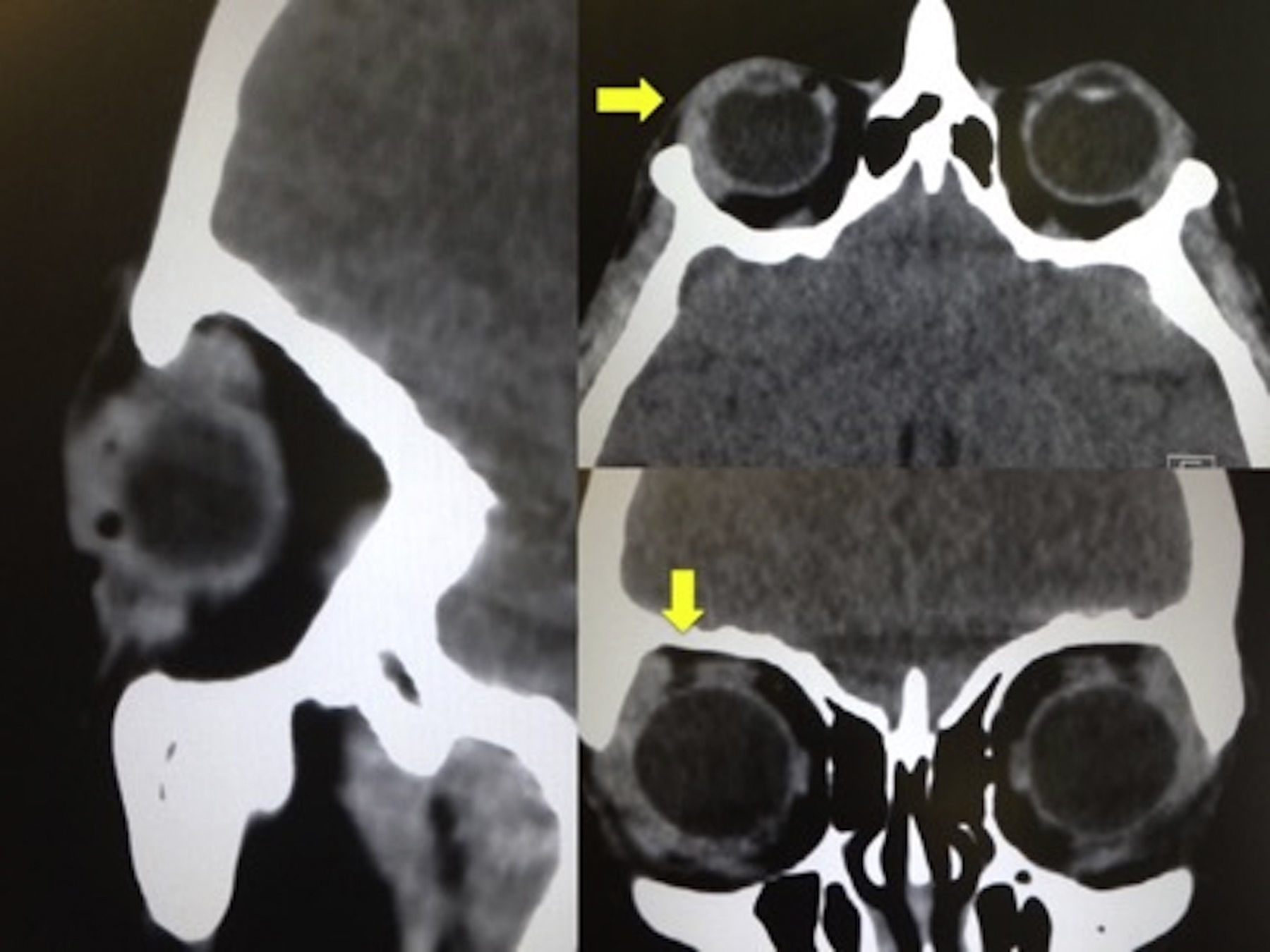
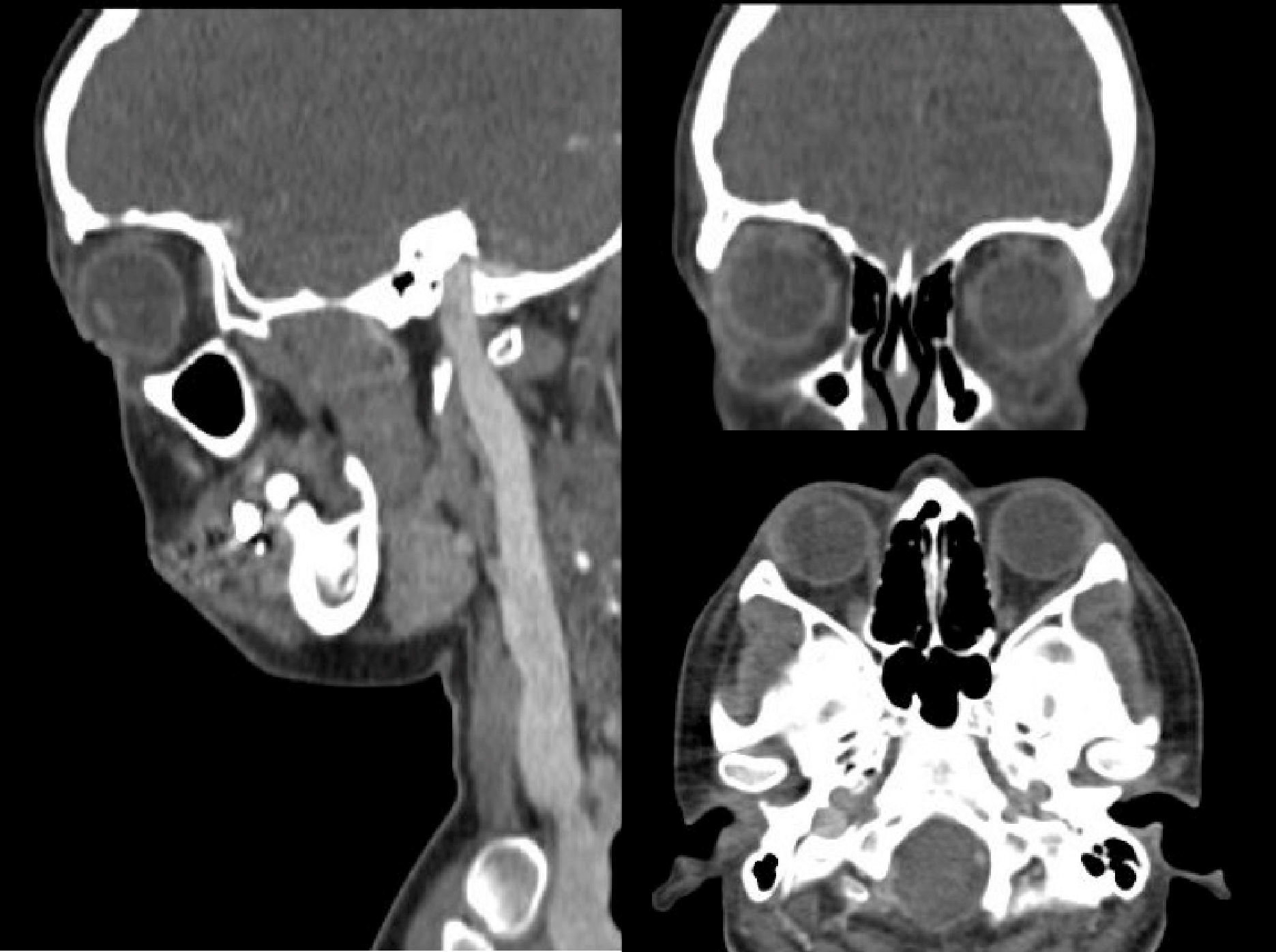
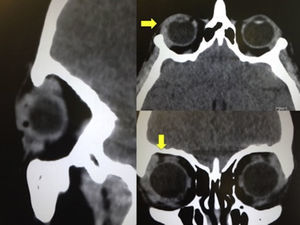
The patient was initially treated by the haematology department with antibiotic therapy for one month, the exact drug and dose are unknown, with no clinical improvement, consequently cranial tomography was requested, which revealed conjunctival enlargement of the right eye (2.6mm), contralateral eye with conjunctival thickness of 1.7mm within normal parameters.
After the treatment described, the patient continued in follow-up for 8 months, during which time FDG PET/CT was again performed showing persisting level IIA bilateral cervical ganglia, with a reduction in the size of the same (less than 10mm) and reduction of the SUVmax 2.9.
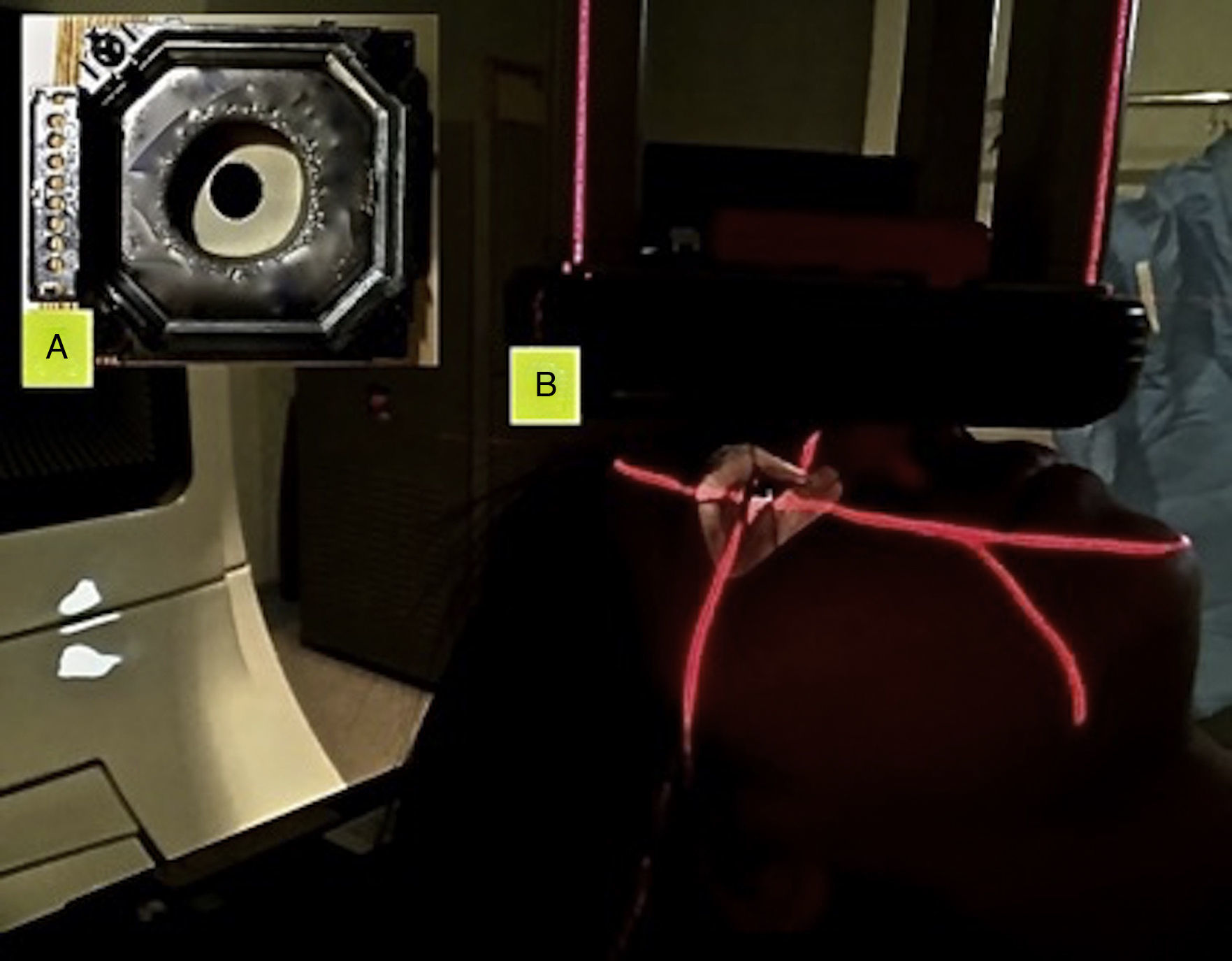
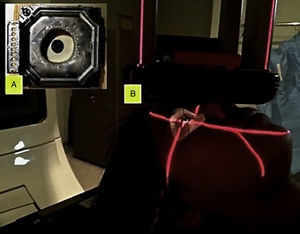
Given the persistence and progression of the disease, the patient was considered to be a candidate for electron-based external radiotherapy, with a prescribed dose of 36Gy in 20 sessions, conventional fractionation of 1.8Gy and a single direct field of treatment, adjusting this, with a cerrobend block to the electron cone to protect the lens, this being considered an organ at risk.
During treatment, the acute toxicity was conjunctivitis, RTOG grade 1 radioepidermitis, no delayed toxicity presented at 18 months of follow-up.
Upon completion of treatment a favourable response was obtained with a 100% reduction in the size of the lesion.
During the 18 month follow-up, a new imaging study was performed (CT scan), which showed no evidence of the disease.
DiscussionWe present the case of a patient diagnosed with conjunctival MALT lymphoma of the right eye. In accordance with the literature, this lymphoma is strongly associated with females, as in the case described. The natural history of the typical disease presents a lesion that tends to slowly and progressively increase in size. In this case the development coincides with that reported in the international literature.
The Haematology Department indicated antibiotic therapy for this patient, since some studies demonstrate that drugs that target C. psittaci can improve symptoms,22,26 however this is only feasible in initial stages, since they have no impact in advanced stages.23,27 In our patient, the conjunctival lesion initially measured 0.5cm and after one month of antibiotic treatment and 8 more months of monitoring, the lesions increased in size to 1.5cm, with an unfavourable response to this first treatment.
It is documented that ERT is an excellent treatment mode for low grade MALT lymphomas located in the conjunctiva, eyelid and lacrimal gland, with few complications and a low recurrence rate. Consequently, the patient was assessed by the Radiotherapy Department.
The dose varied from 25 to 36Gy,12,28,29 including doses between 20 and 25Gy24,28,30 with either photons or electrons; obtaining excellent results, complete response of 84–100% in local control of the disease, improvement in progression-free survival (PFS), relapse-free survival (RFS) which is estimated at 77–94% at 5 years and 71–93% at 10 years.
Moreover, the results from treatment with a 30Gy dose during a 10-year follow-up showed an overall survival (OS) of 97% at 5 years and 93% at 10 years, RFS of 98% at 5 and 10 years, an RFS of the contralateral eye of 97% at 5 years and 90% at 10 years. With this same dose, in tumours larger than 4cm (which have a high probability of relapse or transformation into a high grade lymphoma), patients should be monitored for at least 84 months, since this measure impacts on the RFS of the affected eye and PFS of the contralateral eye.31 In the case described, the prescribed dose was 36Gy, with electrons, in a conventional fractionation (size of fraction between 1.8 and 2Gy per session), to be administered over 20 sessions. In other words, one session per day, 5 times a week for 4 weeks. Taking into account that the size of the patient's lesion was less than 4cm and that the treatment matched that described in the international literature, we expect the OS RFS and PFS to be higher than 90% and that relapse in the contralateral eye does not present.
Since no treatment is innocuous, acute and chronic radio-toxic effects may present. The first are defined as those that present before 90 days. Depending on the degree of toxicity, ERT treatment may be suspended, this being radiobiologically unfavourable, since stopping the ERT sessions results in the accelerated repopulation of clonogenic cells, which impacts on the decrease in local control.
In the case described in this report, during the 4 weeks of treatment, conjunctivitis was the only acute toxic effect that presented, which did not require suspension of the treatment.
One of the chronic radio-toxic effects to be considered during irradiation of the ocular region is the formation of cataracts, which present in relation to the dose. In other words, with a dose of 30.6Gy the probability of affectation of the lens is 32% and with a 25Gy dose this probability decreases to 10%.28
Consequently, it was considered important to take measures to decrease this percentage with the use of ocular protection made of cerrobend material, which will decrease the toxicity of the lens by 13–27%.23,31
In the case presented, the dispersion dose to the rest of the healthy structures was decreased by irradiating the conjunctiva with electrons, using ocular protection made of cerrobend material, which was intended to cover the exposed skin and the rest of the conjunctiva. In addition, in the centre of this protection a 1cm cerrobend circle was placed in order to decrease the dose to the ocular globe.
At 18 months of follow-up, no delayed radio-toxicity was in evidence, accordingly we recommend the use of protectors, since they decrease the dissection dose to adjacent healthy tissue, especially to the lens, and also reduce acute and chronic toxicity caused by the treatment.
It was reported that relapse can be at local, locoregional or systemic level with a frequency of 6–27%. In the orbital-conjunctival region, the main relapse site, the reported level is 51% for the lacrimal gland and 11% for conjunctiva. The average time to local relapse is estimated at 13 months and average time to remote relapse at 40–68 months.28 With a follow-up of 18 months, until now no relapse has presented, assessed from the results of the last CT, where no relapse was detected at any level, thus the patient will continue with appointments every 3 months for 6 additional months and subsequently, every 4 months for 2 years and finally twice yearly for 1 year to complete 5 years of follow-up. If no relapse occurs in this time, discharge from the Radiotherapy Department is planned for the end of 5 years follow-up.
We propose that in patients with conjunctival MALT lymphoma, irradiation should be with electrons at a dose of 36Gy, which is adequately tolerated, with no need to suspend the treatment due to radio-toxicity, using a direct field during the planning, only directed at the lesion, making use of cerrobend blocks, which contributes to reducing the dose to the surrounding healthy tissue. A clinical follow-up with imaging is recommended for at least 5 years, since relapse or transformation, although uncommon, is possible.
ConclusionConjunctival MALT lymphoma is not very common, with an incidence of 2% within the non-Hodgkin lymphomas. It is justified to commence antibiotic therapy as initial treatment, given the association between the lymphoma and bacteria such as C. psittaci.
If the disease persists or progresses, the ideal treatment is RT at a dose of between 25 and 36Gy, since this has shown to have excellent results with respect to local control, overall survival and relapse-free survival, with low toxicity (xerostomia, keratitis, cataracts); however, the toxicity may diminish with the use of a shielded lens or cerrobend blocks.
In patients presenting local relapse, reirradiation may be considered, if the relapse is systemic or, if symptomatic disease presents, the ideal treatment is CT-RT or molecular target-directed therapy.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.