Vascular malformations are anomalies caused by errors in the embryonic differentiation including a large number of diseases of the venous and lymphatic capillary network. They are rare (0.05–3%), and are classified according to their basic structural components (capillary, venous, lymphatic, arterial and combined forms)
Case descriptionThree-months-old boy, was admitted with respiratory distress; and medical history of bronchopulmonary dysplasia and chronic malnutrition, both treated with unknown manage.
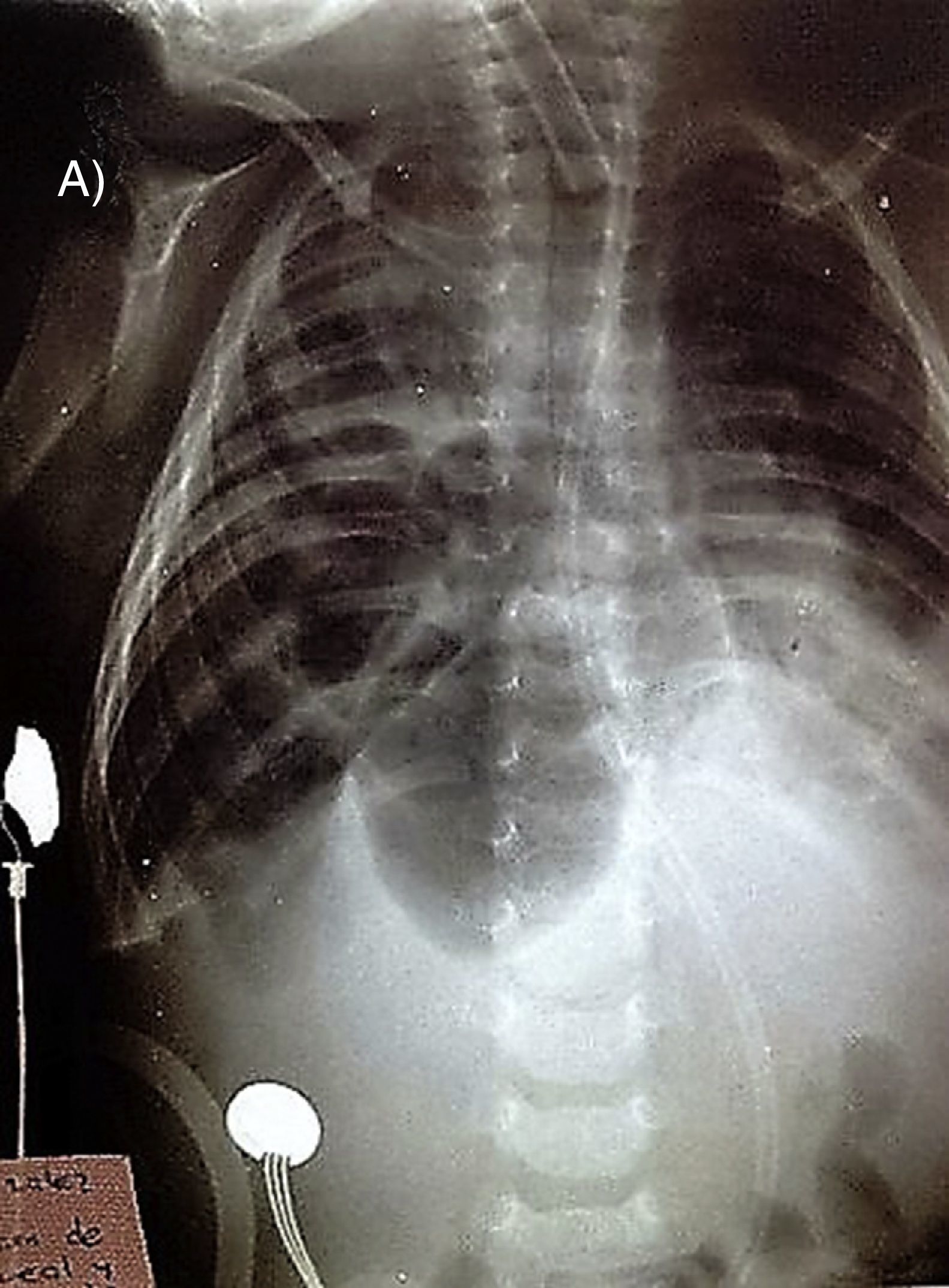
During the physical examination he was found: with poor general condition, atrial murmur grade IV and bilateral crackles on auscultation. Anteroposterior and lateral radiographs of the chest were taken; which they revealed polyhedral images in mediastinum and right chest; as well as cardiac silhouette shifted.
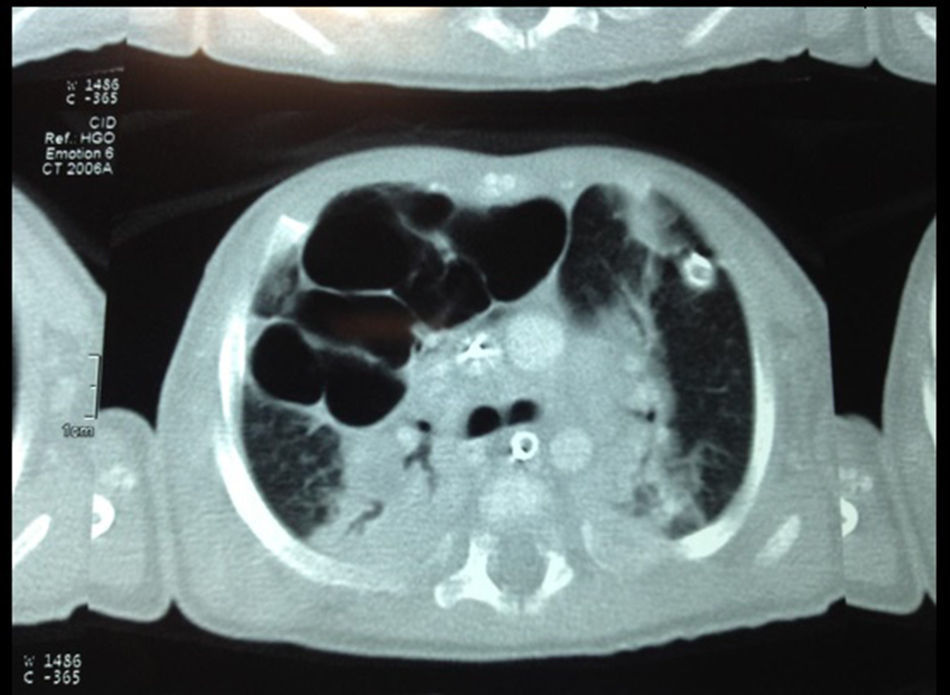
It was performed chest CT; in where multiple intrapulmonary air cysts in the middle lobe were observed; just as in previous and basal segments of the lower lobe of the right lung lesions rounded morphology.
It was made right middle lobectomy. Pathologic findings reported cellular elements compatible with hemangio-lymphangioma.
ConclusionDespite its “benign” histological quality, the hemangiolynphangioms are relate to severe deformity of cavity and limbs, due to the high capacity to invade locally organs and adjacent tissues (muscle, bone and soft tissue), accompanied by growth fast and high probability of local recurrence. Therefore, generally associated symptoms are mainly mechanical nature and depend on the damage to adjacent tissue, anatomic location of the lesion and the same size.
Las malformaciones vasculares son anomalías ocasionadas por errores en la diferenciación embrionaria que incluyen un amplio número de enfermedades de la red venosa, capilar y linfática; son poco frecuentes (0.05 al 3%), y se clasifican según sus componentes estructurales básicos (capilares, venosas, linfáticas, arteriales y formas combinadas)
Descripción del casoMasculino de tres meses de edad, quien ingresó por dificultad respiratoria; con antecedente de displasia broncopulmonar y desnutrición crónica, ambos tratados con manejo desconocido.
Durante la exploración física se encontró: paciente con mal estado general, soplo auricular grado IV y estertores crepitantes bilaterales a la auscultación. Se tomaron radiografías de tórax anteroposterior y lateral; las cuales revelaron imágenes poliédricas en mediastino y hemitórax derecho; asi como silueta cardiaca desplazada de forma contralateral.
Le fue realizada tomografía computarizada de tórax; en donde se observaron múltiples quistes aéreos intrapulmonares en el lóbulo medio; de igual manera en segmentos anteriores y basales del lóbulo inferior del pulmón derecho con lesiones de morfología redondeada.
Se efectuó lobectomía media derecha; los resultados anatomopatológicos reportaron elementos celulares compatibles con un hemangio-linfangioma.
ConclusiónA pesar de su cualidad histológica “benigna”, los hemangiolinfangiomas se relacionan a deformidad severa en cavidad y extremidades, debido a la alta capacidad para invadir de forma local órganos y tejidos adyacentes (músculo, hueso y tejidos blandos), acompañada de crecimiento rápido y probabilidad de recidiva local elevada. Por tal motivo, generalmente, los síntomas asociados son fundamentalmente de índole mecánica y dependen del daño a tejidos contiguos, localización anatómica de la lesión y tamaño de la misma.
Vascular malformations are anomalies caused by errors in the embryonic differentiation including a large number of diseases of the venous, lymphatic and capillary network; are rare (0.05–3%), and are classified according to their basic structural components (capillary, venous, lymphatic, arterial and combined forms).1–3
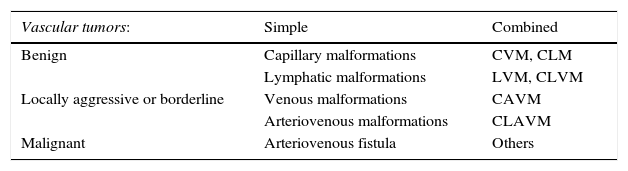
Due to the serious problems for its nomenclature, in 1982, Mulliken and Glowacki proposed a classification based on biological and histopathological differences were two groups were distinguished: benign vascular malformations and vascular tumors. This classification was adopted by the International Society for the Study of Vascular Anomalies (ISSVA) and in recent years (2014) it was revised (Table 1).4–7 Also can be divided into low-flow lesions (capillary, venous, lymphatic or combinations) and high flow injuries (usually arteriovenous components).2,4,6
Vascular anomalies.
| Vascular tumors: | Simple | Combined |
|---|---|---|
| Benign | Capillary malformations | CVM, CLM |
| Lymphatic malformations | LVM, CLVM | |
| Locally aggressive or borderline | Venous malformations | CAVM |
| Arteriovenous malformations | CLAVM | |
| Malignant | Arteriovenous fistula | Others |
ISSVA classification for vascular anomalies (Approved at the 20th ISSVA Workshop, Melbourne, April 2014).
Commonly they are diagnosed during childhood and have a favorable outcome.1,5–7 In 90% of cases, vascular abnormalities can be differentiated through the detailed physical examination, however it is necessary to consider the patient's age, evolution, injury extension and possible complications for the treatment.1,8,9
Complementary studies are rarely necessary; however, Doppler ultrasound and MRI are useful for the diagnosis of deep lesions.
Case reportThree-months-old male, was admitted with respiratory distress and a clinical history of bronchopulmonary dysplasia and chronic malnutrition, both conditions were previously treated with unknown manage. During the physical examination (PE) it was found: patient with poor general condition, atrial murmur (grade IV), bilateral rattles and crackles on auscultation; with auxiliary ventilation and inotropic support.
Anteroposterior and lateral radiographs of chest (Fig. 1), revealed polyhedral images on mediastinum and right chest; as well as cardiac silhouette shifted to contralateral side; for this reason, Morgagni's diaphragmatic hernia was suspected.
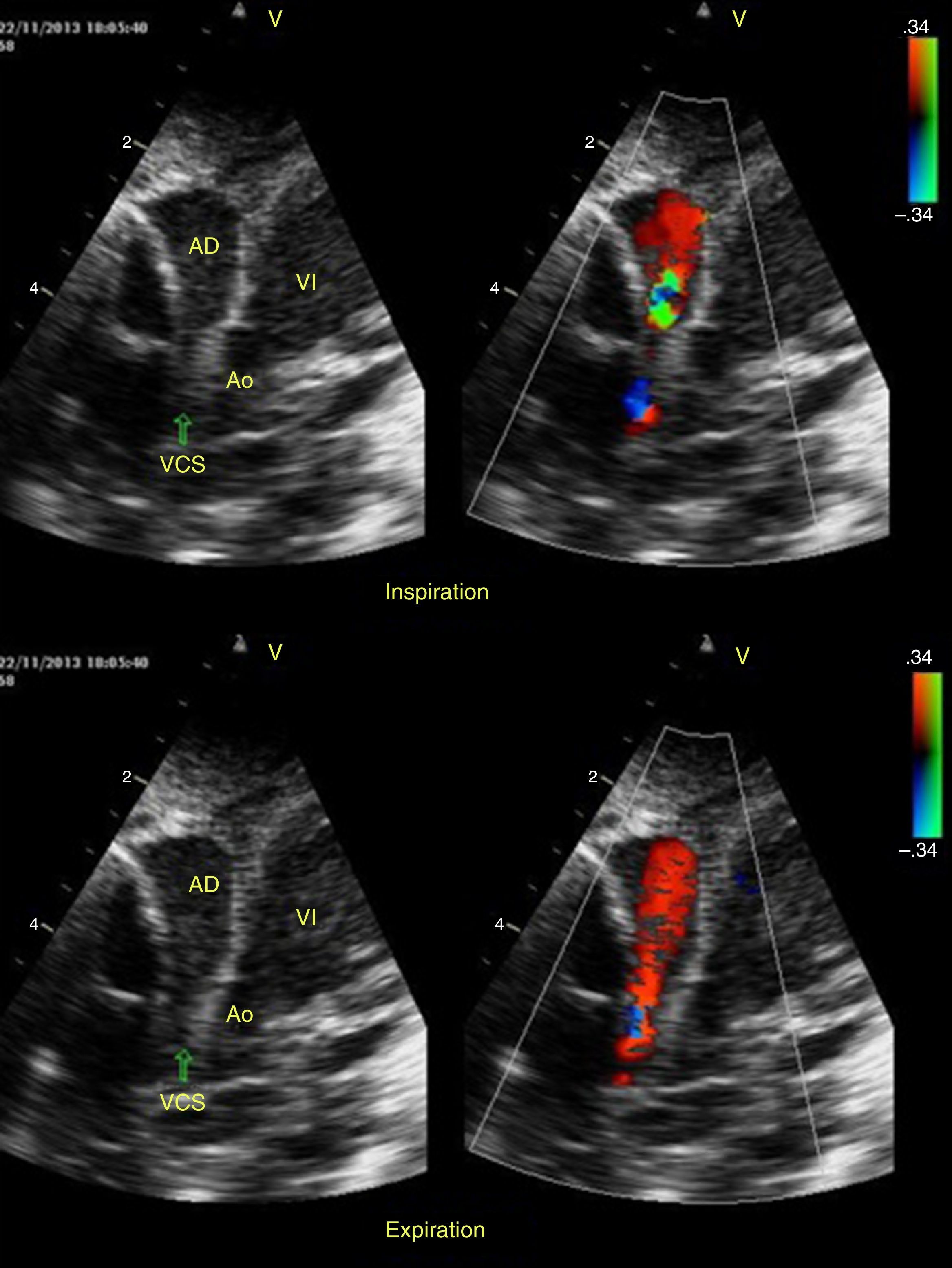
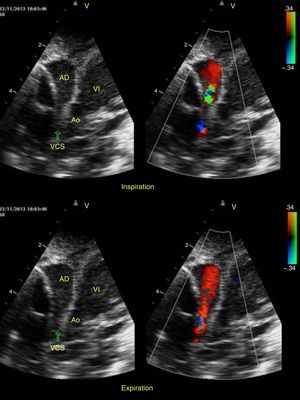
He underwent an echocardiogram study (Fig. 2), in which mechanical obstruction of the flow was revealed by extrinsic compression of the right atrium (RA) and superior vena cava (SVC), with reduction of preload at inspiration.
Exploratory laparotomy was performed; the main finding was integral diaphragm flawless in its entirety.
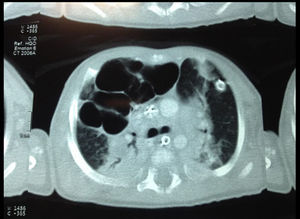
Subsequently, chest CT (Fig. 3) was performed. Intrapulmonary multiple cysts in the middle lobe were observed; the largest measured 32mm in diameter. Similar images were found in anterior and basal segments of the lower lobe at the right lung; was suspected post-infectious neumatocele.
Due to decreasing overall during evolution, surgical re-intervention was decided; in where right middle lobectomy was performed. The surgical findings were: multiple cystic lesions predominating in medial area of 5cm (approx.) of diameter in upper lobe, without evidence of granulomatous tissue or data purulent discharge.
After the procedure, he was evaluated by an echocardiogram where the SVC was extended. Also, displayed lesser retrograde flow by dilatation of the right chambers and lower pulmonary blood pressure (85mmHg). As treatment, was used sildenafil.
After 2 days of extubating, was performed a new echocardiogram. The study reported ventricular hypertrophy, interventricular septum with paradoxical movement, bi-ventricular diastolic dysfunction; and pulmonary artery pressure of 55mmHg. He was discharged to home on the 19th day of hospital stay after improvement.
The anatomopathological study results reported compatible cellular elements with a hemangio-lymphangioma.
DiscussionLymphangioma (lymphaticum angioma) are congenital malformations of the vascular system comprising newly formed lymph; differ in their clinical appearance, radiological and pathological findings and their biological behavior.3,10
Although its etiology is not fully described, there are various theories; the most accepted considers a defect of differentiation during embryogenesis from the sixth week, where an error in the formation of the jugular sacs, with anomalous result of deposits of lymphatic tissue occurs; also the consequent connection of the capillary system and lymphatic system.3,11–13
According Landing and Farber14 are divided into four categories: (1) capillary lymphangioma, (2) cavernous lymphangioma, (3) cystic lymphangioma (hygroma) and (4) haemangiolymphangioma. Also Rosillo-Ruiz et al. classify the vascular malformations, where they make reference to “linfangiohemangiomas” as benign neoplasms.
As already mentioned, hemangiolymphangioms (HLP) are mixed vascular malformations of benign type, composed of nodes and capillary elements; mostly occurring in childhood and presentation decreases as age increases.1–6 Its incidence is estimated at one per 12,000 newborns (approx.); predominates in men (2–2.4: 1) premature (40–60% can be considered congenital); commonly (95% of cases) originate from own structures of the head (oral cavity, orbit, etc.), neck and mediastinum (esophagus, and pericardium), also axillary region. To a lesser extent come from abdominal cavity, retroperitoneum (adrenal gland), rectum, cervix and limbs.11,15,16
The HLP have been associated with lymphatic Klippel-Trenaunay syndrome, which is characterized by congenital overgrowth of vascular tissue, manifested by congenital varicose veins or venous malformations, capillary malformations or wine stains covering a large area and soft-tissue hypertrophy8; but in this case it was not possible to prove the existence of such a syndrome due to the absence of characteristics of the disease.
Despite its “benign” histological quality of HLP is related to severe deformity of cavity and limbs, because the high capacity to locally invade adjacent organs and tissues (muscle, bone and soft tissue), accompanied by rapid growth and high probability of local recurrence. Therefore, the associated symptoms are essentially mechanical and depends of the damage to adjacent tissue, anatomic location of the lesion and size of it, as in this report.10–13
The diagnosis is usually clinical; sometimes can achieve great proportions before being diagnosed and cause compression symptoms, cough and dyspnea. It can infiltrate neighboring organs and been locally invasive.
It is noteworthy that, in the current medical literature, reports related to pulmonary HLP are extremely limited, not to mention zero; but its importance lies in the severity of complications caused, generally by the invasion of adjacent structures or by the compressive effect on them. As happened in this case which have demonstrated extrinsic compression of the right atrium.
Lymphatic malformations tend to occur in loose tissues, where they can expand and create large cystic spaces as demonstrated in this case by CT (Fig. 3).9,13
In this case, the presence of a mixed malformation of lymphatic vascular characteristics, as well as high flow features, could be the origin of hemodynamic decompensation, which initially appeared as breathlessness.
While nutritional deficits of the patient are unknown, according to the current literature, it is likely that the state of chronic malnutrition were associated with this type of vascular malformations, either by their interaction with adjacent organs such as the intestine, which can cause gastrointestinal bleeding or tube intrinsic cause chronic blood loss; It is also associated with states of anemia.13
In agreement with the most reports or case series, the HLP diagnosis is made during the first years of life through simple radiographic studies; also Doppler ultrasound and computed tomography (CT) are used for the differentiation and delineation of structures respectively.1–6,10,17,18 In our case, due to the uncertainty caused by the images obtained by simple radiography and subsequent suspected diaphragmatic hernia, it was done Doppler ultrasound, showing extrinsic obstruction of the heart; it was necessary to introduce the patient to CT, in where multiple lesions were visualized aforementioned characteristics. It is noteworthy that, as in casuistry currently identifying the injury was incidental. Despite the existence of reports (five approx.) with prenatal diagnosis, there was no such in our case.15–17
The differential diagnosis should consider any other benign or malignant neoproliferative disorder that affects the lungs as: intravascular bronchioloalveolar tumor (also called angiogenic tumor sclerosing), pulmonary neoplasm of endothelial origin usually detected incidentally, that in half of the cases leads to death due to progressive respiratory failure; however, is usually manifested radiologically as multiple pulmonary nodules of small size. We must also think of a pulmonary hamartoma, whose peak incidence is in the sixth decade but these tend to be solitary, well-circumscribed peripheral pulmonary masses.19
The treatment is by surgical intervention; consisting in that the tumor resection with negative edges due to its high probability of relapse; although in this case there was no diagnostic accuracy prior to surgery, lobectomy performed meets the therapeutic guidelines described above.
As in reports Campos et al.15 and Nakamura et al,18 postoperative complication was held pulmonary hypertension; although both reported no therapeutics used, here it was decided to use sildenafil for its effectiveness in the treatment of this entity.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.