Mediastinitis is a potentially fatal condition. In addition to timely diagnosis, its prognosis depends on an early and systematic approach.
ObjectiveTo describe the results of mediastinitis treatment over a period of 34 years in a teaching hospital, its evolution and the current model of care.
Materials and methodsCross-sectional, retrospective and descriptive study of patients with mediastinitis admitted from 1 June 1982 to 30 July 2016. The analysed variables were demographic, classification and aetiology of mediastinitis, comorbidities, complications, length of hospital and intensive care unit stay and mortality.
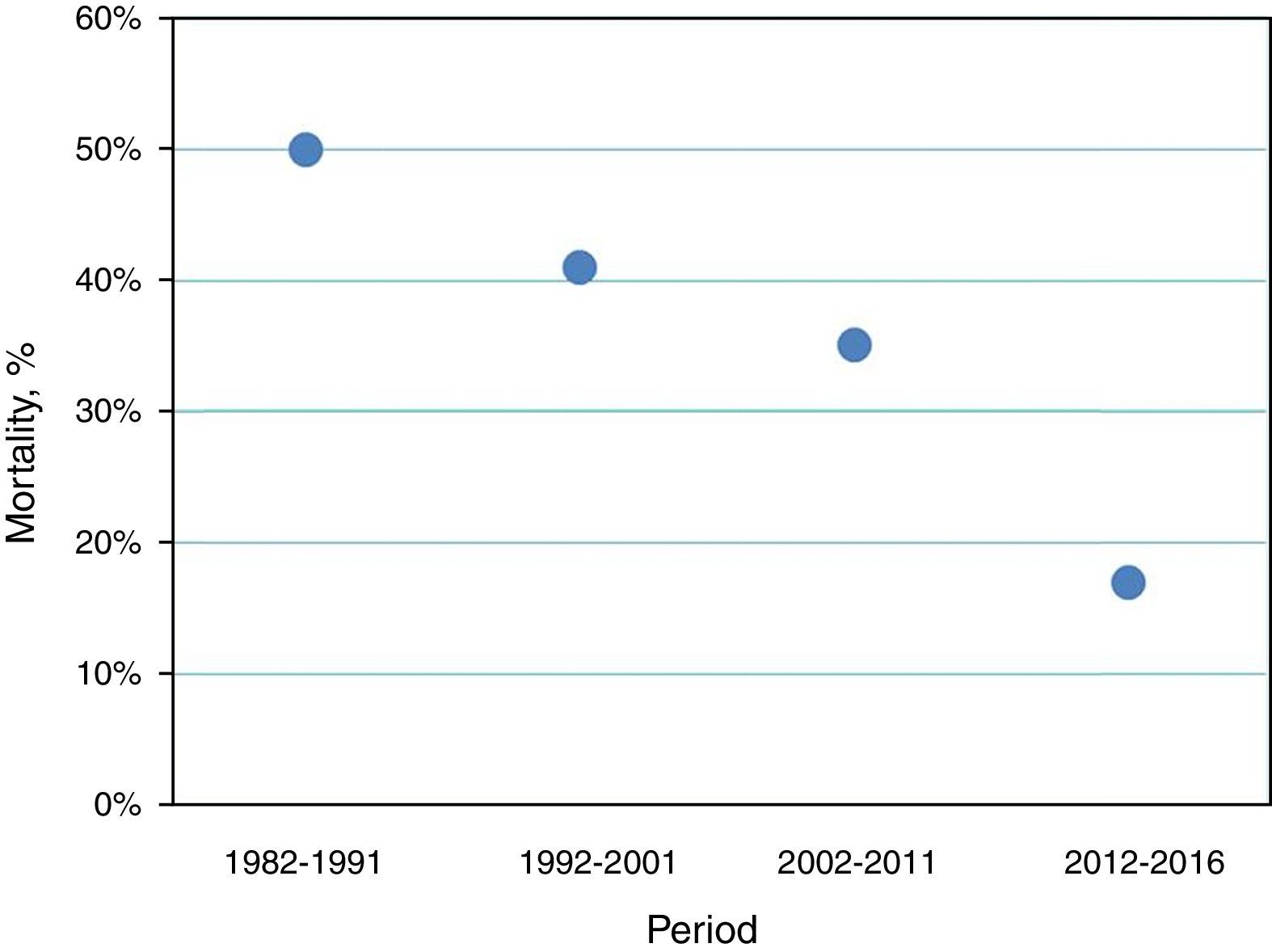
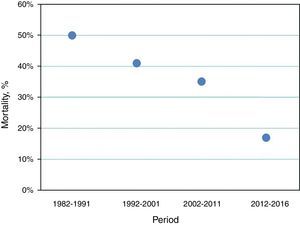
Results1880 patients were included of which 1496 (79.6%) were men. The mean age was 39.4±17.8 years. According to the classification of Endo, 603 (32.1%) corresponded to type I and 1277 (67.9%) to types IIA and IIB. According to the aetiology, in 910 cases the origin was odontogenic (48.4%), 526 due to retropharyngeal abscess (28%), 147 secondary to submandibular abscess (7.8%), 49 due to cervical lymphadenectomy (2.6%), 36 due to pharyngeal trauma (1.9%), 14 due to post-intubation tracheal rupture (0.7%) and 198 were of undetermined origin (10.6%). Mediastinotomy with right thoracotomy was performed in 86% and mediastinotomy with left thoracotomy was performed in 14%. Simultaneous tracheostomy was performed in 83% of cases, standardising this procedure since 2005. Mortality varied between periods and was 50% in 1982–1992, 41% in 1992–2001, 35% in 2002–2011 and 17% in 2012–2016.
ConclusionAlong with the standardisation of the management of mediastinitis, a fall in mortality from this cause has been observed over the years. The maturity of the proposed model of care is a result of, among other things, medical and scientific advances and the experience gained in this pathology over more than three decades.
La mediastinitis es un padecimiento potencialmente fatal. Además del diagnóstico oportuno el pronóstico dependerá de un abordaje sistemático temprano.
ObjetivoDescribir los resultados del tratamiento de la mediastinitis en un periodo de 34 años en un hospital escuela, su evolución y el modelo de atención vigente.
Material y métodosEstudio retrospectivo, descriptivo y transversal de pacientes con mediastinitis ingresados del 1 de junio de 1982 al 30 de julio de 2016. Las variables que se analizan son demográficas, clasificación y etiología de la mediastinitis, comorbilidades, complicaciones, días de estancia en hospital y en terapia intensiva y mortalidad.
ResultadosSe incluye a 1880 pacientes de los cuales 1496 (79.6%) fueron hombres. La edad promedio fue de 39.4±17.8 años. Según la clasificación de Endo, 603 (32.1%) correspondieron al tipo I y 1277 (67.9%) a los tipos IIA y IIB. Según la etiología, en 910 casos fue de origen ondotogénico (48.4%), 526 por absceso retrofaríngeo (28%), 147 secundarios a absceso submandibular (7.8%), 49 a linfadenectomía cervical (2.6%), 36 a trauma faríngeo (1.9%), 14 a ruptura traqueal postintubación (0.7%) y 198 de origen indeterminado (10.6%). Se realizó mediastinotomía con toracotomía derecha en 86% y con toracotomia izquierda en 14%. La traqueostomía simultánea se realizó en el 83% de los casos, estandarizándose desde el año 2005. La mortalidad varió por periodos siendo de 50% en 1982 a 1992, de 41% en 1992 a 2001, de 35% en 2002 a 2011 y de 17% en 2012 a 2016.
ConclusiónA la par de una estandarización en el manejo de la mediastinitis, se observa un descenso en la mortalidad por esta causa con el pasar de los años. La madurez del modelo de atención que se propone responde entre otros a avances médico-científicos y a la experiencia acumulada en esta patología en más de tres décadas.
The mediastinum is a closed compartment that contains vital structures such as the heart, the great vessels, trachea and bronchi. Inflammation of the connective tissue that surrounds these structures, known as mediastinitis, is the result of various factors and has a reported mortality rate of between 12% and 47%,1,2 with a better prognosis when a systematic approach is used that includes timely identification, confirmation and surgery. In its acute form, despite being considered a rare condition, mediastinitis is becoming more frequent in our field, and is a phenomenon that is apparently linked to the increase in the prevalence of chronic diseases. Scientific literature on the topic remains limited and largely consists of a series of cases.3 In the Pneumology and Thoracic Surgery Department of the General Hospital of Mexico, between 30 and 50 patients are treated every year for this illness. As this is considered to be a serious health problem, the systematisation and protocolisation of its management is necessary. This study aims to describe the results of the treatment of mediastinitis over a period of 34 years, its characteristics, risk factors, complications and progression, along with the current model of care at our site.
Materials and methodsStudy typeRetrospective, descriptive, cross-sectional.
Patients and siteAll patients that were admitted to hospital in Pneumology and Thoracic Surgery with a diagnosis of mediastinitis were enrolled. The General Hospital of Mexico is a public hospital with 1143 beds during the period between 1 June 1986 to 30 July 2016.
Variables of interestThe variables analysed were obtained directly from the Department's clinical and radiological files and computed databases of patients diagnosed with mediastinitis during the study period. Mediastinitis was classified according to the criteria of Endo,4 and, in the case of patients with descending necrotising mediastinitis (DNM), compliance with the diagnostic criteria of Estrera was also verified,5 with retrospective classification for cases that presented themselves prior to these classifications. The variables of interest were demographic, classification and aetiology of mediastinitis, comorbidities, complications, length of hospital and intensive care unit stay and mortality.
Statistical analysisDescriptive statistics were used. Quantitative variables are expressed in arithmetic means±standard deviation and qualitative variables in numbers and percentages.
Current model of care for mediastinitisIncludes the emergency surgical approach with posterolateral thoracotomy in layers. Once the thoracotomy has been performed, the lungs can be accessed if there are adhesions and a sample of pleural fluid is taken if there is any. In cases of DNM, the retrovisceral space connecting the neck with the mediastinum is examined in the first instance while dissecting the different structures. Then the retrosternal space connecting both hemithoraces is examined, and later the pretracheal, retroesophageal and preaortic spaces are dissected, ensuring that the azygos vein is properly released and allowing free drainage. Should this not be possible the vein should be ligated and cut. Once dissection of the mediastinum is complete, it is washed with a lukewarm sterile solution mixed with hydrogen peroxide to a ratio of 50:1, and two right chest tubes and one left are placed, which, depending on drainage, will be removed one at a time. In the case of DNM, management includes prior drainage of neck abscesses in the same surgery undertaken by the Otorhinolaryngology Department.
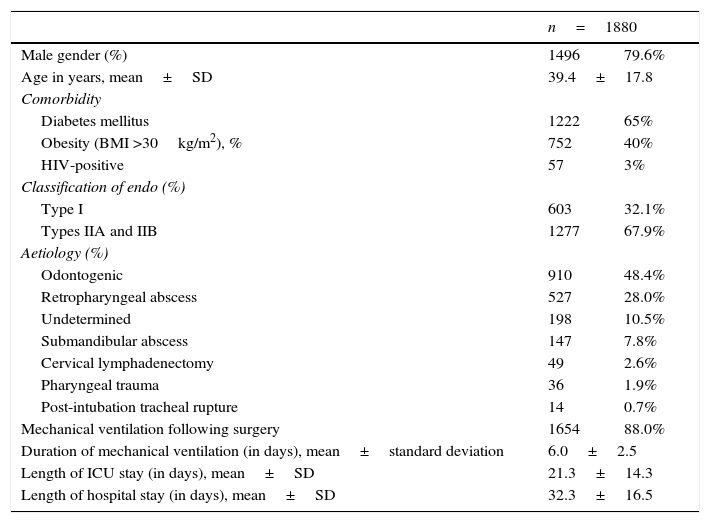
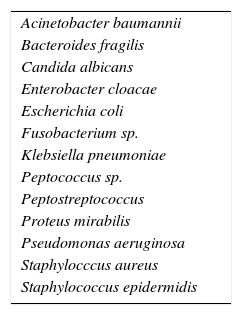
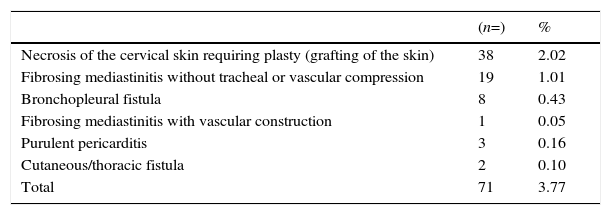
ResultsA total of 1880 patients diagnosed with mediastinitis were included of which 1496 (79.6%) were men. The mean age was 39.4±17.8 years. Demographic characteristics, comorbidity, and the classification and aetiology of mediastinitis are shown in Table 1. Time to progression from the onset of the illness to hospital admission was on average 8.5±2.5 days. Approximately 78% of patients received some form of medical treatment prior to their arrival at hospital (mostly oral antibiotics). The average time from arrival at hospital to surgery was 6h. The radiological findings upon admission were: mediastinal widening (in 100% of cases), pneumomediastinum (93%), mediastinal abscess (25%), and a combination of these findings in 80% of cases. A chest CT scan was performed in all patients, which confirmed the findings of the chest X-ray. In cases of DNM, a pre- and postsurgical diagnosis was made according to the criteria of Estrera.5 Out of the total patients, mediastinotomy with right thoracotomy was performed in 86% and mediastinotomy with left thoracotomy was performed in 14%, a decision based on the clinical/radiological assessment of the cases. Time to removal of chest tubes varied from 7 to 45 days. Simultaneous tracheostomy was performed in 83% of cases, with this procedure being standardised since 2005. The bacteria isolated in positive cultures are shown in Table 2. Postsurgical morbidity rate was 3.77%. Postoperative complications are shown in Table 3. Mortality varied between periods and was 50% in 1982–1992, 41% in 1992–2001, 35% in 2002–2011 and 17% in 2012–2016 (see Fig. 1).
Characteristics of the patients included.
| n=1880 | ||
|---|---|---|
| Male gender (%) | 1496 | 79.6% |
| Age in years, mean±SD | 39.4±17.8 | |
| Comorbidity | ||
| Diabetes mellitus | 1222 | 65% |
| Obesity (BMI >30kg/m2), % | 752 | 40% |
| HIV-positive | 57 | 3% |
| Classification of endo (%) | ||
| Type I | 603 | 32.1% |
| Types IIA and IIB | 1277 | 67.9% |
| Aetiology (%) | ||
| Odontogenic | 910 | 48.4% |
| Retropharyngeal abscess | 527 | 28.0% |
| Undetermined | 198 | 10.5% |
| Submandibular abscess | 147 | 7.8% |
| Cervical lymphadenectomy | 49 | 2.6% |
| Pharyngeal trauma | 36 | 1.9% |
| Post-intubation tracheal rupture | 14 | 0.7% |
| Mechanical ventilation following surgery | 1654 | 88.0% |
| Duration of mechanical ventilation (in days), mean±standard deviation | 6.0±2.5 | |
| Length of ICU stay (in days), mean±SD | 21.3±14.3 | |
| Length of hospital stay (in days), mean±SD | 32.3±16.5 | |
SD, standard deviation; BMI, body mass index; ICU, intensive care unit.
Bacteria isolated in positive cultures.
| Acinetobacter baumannii |
| Bacteroides fragilis |
| Candida albicans |
| Enterobacter cloacae |
| Escherichia coli |
| Fusobacterium sp. |
| Klebsiella pneumoniae |
| Peptococcus sp. |
| Peptostreptococcus |
| Proteus mirabilis |
| Pseudomonas aeruginosa |
| Staphylocccus aureus |
| Staphylococcus epidermidis |
Postoperative complications.
| (n=) | % | |
|---|---|---|
| Necrosis of the cervical skin requiring plasty (grafting of the skin) | 38 | 2.02 |
| Fibrosing mediastinitis without tracheal or vascular compression | 19 | 1.01 |
| Bronchopleural fistula | 8 | 0.43 |
| Fibrosing mediastinitis with vascular construction | 1 | 0.05 |
| Purulent pericarditis | 3 | 0.16 |
| Cutaneous/thoracic fistula | 2 | 0.10 |
| Total | 71 | 3.77 |
Considered a rare condition, mediastinitis most frequently occurs in the postoperative period following sternotomy for cardiac surgery; it often arises from oesophageal perforation and DNM (severe oropharyngeal infection spreading to the thorax).2 Mediastinitis can be secondary to trauma to the central airway, cervical lymphadenitis and, to a lesser degree, the origin may be undetermined.6,3 The series of cases presented (the largest series of cases known to the authors to date) predominantly included patients with DNM and a smaller proportion of cases that were secondary to tracheal rupture of undetermined origin, which is explained due to the fact that in our hospital cardiac surgery patients and those with oesophageal perforation are mostly admitted to the cardiology and gastrosurgery departments, respectively.
As this is a serious disease with a high mortality rate, it is necessary to learn more from the case studies and standardise protocols for mediastinitis that will lead to better clinical outcomes. In the first instance, we note that this is an illness that affects young male adults with a male-female ratio of 4:1, similar to that already reported.3 The most common comorbidity was diabetes mellitus, a chronic disease that has been linked to the development of DNM7,8 and for this reason it is a risk factor for death due to this cause.9 Obesity has also proven to be a risk factor for the development of poststernotomy mediastinitis.10 Considering a significant proportion of the patients included (40%) had a body mass index of >30kg/m2, obesity could also play a role in influencing the development of mediastinitis of other origins, namely DNM. Deu-Martín et al.9 were also unable to find a delay in diagnosis/treatment of over 72h as a predictor of mortality; however, in the group of patients that was analysed, the delay in seeking medical attention was considerably lengthy, around eight days on average, with more than three-quarters of the patients having received some form of medical treatment. Despite the limited resources of public hospitals, time from diagnosis to surgery, which was 6h on average, is similar to that reported in other case series11; as it is considered to be an emergency surgical indication, mediastinitis, along with other thoracic surgical indications at our site, has been proven to have a better prognosis compared to surgical emergencies in areas other than the thorax.12
Although early intervention is considered to be an indicator of a good prognosis, there is currently no consensus as to the way in which to approach mediastinitis from a surgical point of view. There are groups that propose different approaches such as the technique of selection according to results (generally in small case series). The most described approaches are the transcervical,11,13 posterolateral thoracotomy,14,15 anterolateral thoracotomy16 and median sternotomy3 approaches, the transthoracic approach,6,17,18 and those of thoracoscopy and mediastinoscopy1,19 and variations or combinations of the techniques described18,20–23 with or without adjuvant treatments such as the use of a hyperbaric chamber24 or vacuum devices.25 One of the biggest controversies continues to be the treatment of mediastinitis, which is limited to the superior mediastinum above the tracheal carina2,26,27 in which there are those that advocate a conservative approach. Our stance is to opt for a thoracotomy from the outset.
The proposed model of care (right posterolateral thoracotomy in layers, connecting both hemithoraces through the retrosternal space, dissection and washing of the mediastinum, placing two endopleural tubes in the right hemithorax and one in the left, and where necessary, prior cervical drainage with cervico-mediastinal retrovisceral access) has been in place since 2005 at our site and with good results. Early tracheotomy during initial surgery appears to be a promising strategy14 that is associated with better results. We have observed that the mortality rate for mediastinitis at our site has decreased on par with the global trend.28,29 The phenomenon of the decrease in mortality at this institution may well be a result of the protocolisation of the approach, medical and scientific advances that include broad-spectrum intravenous antibiotic therapy, management protocols in intensive care units, ongoing monitoring by medical specialists at these units and technological advances in organ support,30,31 as well as early recognition and surgical treatment20,32 among other things.
One of the greatest advantages of the study that we are presenting is the number of patients included and the period that the study covers; however, at the moment its retrospective nature limits it to describing only a few variables in detail. While the proposed model of care has shown good results at our site, the validation of same requires a more stringent design that can compare groups that have been subject to different techniques.
ConclusionsMediastinitis continues to be a serious condition with a high mortality rate. To date, there is no consensus regarding the best surgical technique for its treatment. In our experience, along with the standardisation of the management of mediastinitis, we have observed a fall in mortality from this cause over the years. The maturity of the proposed model of care is a result of, among other things, medical and scientific advances and the experience gained in this pathology over more than three decades.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNone.
Conflict of interestThe authors declare that there is no conflict of interest related to the drafting of this manuscript.