At present, there is no known risk factor analysis in patients undergoing nephrectomy secondary to lithiasis that favor their entry into the intensive care unit. There is no consensus in methods that report post-surgical complications. As a consequence, the reported incidence of complications in renal surgery ranges from 2% to 54%, regardless of the surgical approach.
MethodologyA total of 58 patients with diagnosis of renal exclusion confirmed by renal scintigraphy, and lithiasis, were submitted to simple nephrectomy by a group of expert surgeons. A total of 58 patients were evaluated. Descriptive statistics were measured for the demographic variables. Inferential statistics were evaluated in quantitative variables using the Student's T test, with a p<0.005. Chi square test was used for the qualitative variables.
ResultsWhen the multivariate analysis was carried out between the variables: age, weight, height, diabetes mellitus, systemic hypertension, smoking, abscess and transfusion, it was not possible to identify correlation between these and the development of complications or admission to the intensive care unit. However, when assessing by logistic regression the relationship between transfusing a patient and developing complications, a positive relationship was found with a p=0.003, and an OR 13.45 CI [2.4–72]. Patients who suffered complications required a longer stay in the intensive care unit (p=0.002).
ConclusionsIt was observed that patients with comorbidities such as hypertension, diabetes mellitus and anemia are more likely to require handling per unit of intensive care, even greater in those requiring transsurgical transfusion. Because there are not enough studies that relate the different risk factors that require intensive care unit management, a risk classification or transsurgical transfusion indications in these patients cannot yet be mentioned.
En la actualidad no se conoce un análisis en lo que se refiere a los factores de riesgo en pacientes sometidos a nefrectomía secundario a patología litiásica que favorezcan su ingreso a la unidad de cuidados intensivos. A pesar de que las tazas de complicaciones son utilizadas para comparar el éxito en las distintas técnicas quirúrgicas, no hay un consenso en los métodos que reporten complicaciones post quirúrgicas. Por consecuencia, la incidencia reportada de complicaciones en la cirugía renal va del 2% al 54%, independientemente del abordaje quirúrgico.
MetodologíaSe incluyeron un total de 58 pacientes con diagnóstico de exclusión renal confirmado mediante gamagrafía renal, y litiasis, sometidos a nefrectomía simple por un grupo de cirujanos expertos. Se realizó medición de estadística descriptiva para las variables demográficas. La estadística inferencial fue evaluada en variables cuantitativas se utilizando la prueba T de Student, con una p<0.005. Para las variables cualitativas se utilizó prueba de Chi cuadrada.
ResultadosAl realizar el análisis multivariado entre las variables: edad, peso, talla, Diabetes Mellitus, Hipertensión Arterial Sistémica, tabaco, presencia de absceso y transfusión no se logró identificar correlación entre estas y el desarrollo de complicaciones o el ingreso a la unidad de cuidados intensivos. Sin embargo, al momento de evaluar mediante regresión logística la relación entre transfundir a un paciente y el desarrollo de complicaciones se encontró relación positiva con una p 0.003, y un OR 13.45 CI [2.4-72]. Los pacientes que sufrieron complicaciones requirieron mayor estancia en la unidad de cuidados intensivos (p=0.002).
ConclusionesSe observó que en los pacientes en quienes presentan comorbilidades como son hipertensión, Diabetes Mellitus y anemia son más propensos a requerir manejo por unidad de cuidados intensivos siendo aún mayor en los que se requirió de transfusión transquirurgica. Debido a que no se cuentan con suficientes estudios que relacionen los diferentes factores de riesgo que hagan requerir de manejo por unidad de cuidados intensivos no se puede aún hablar de una clasificación de riesgo ni de indicaciones de transfusión transquirurgicas en estos pacientes.
Kidney-related diseases have helped to understand the normal physiology of the kidney. As a result of a better understanding of the anatomical structures and the pathophysiology of the kidney, the surgical approaches for the management of diseases related to the kidney have evolved. Since the first successful nephrectomy in 1869 for the management of a ureterovaginal fistula to the first radical nephrectomy, the reconstruction of the vena cava and renal vessels, as well as the advances made in transabdominal and retroperitoneal approaches in renal surgery have all helped to better understand the renal anatomy and its surrounding structures.1–6
However, no analysis has been intentionally performed in regard to risk factors in patients undergoing nephrectomy secondary to lithiasis that promote their admission to the intensive care unit. Although complication rates are used to compare success in different surgical techniques, there is no consensus in methods that report post-surgical complications. As a result, the reported incidence of complications in renal surgery ranges from 2% to 54%, regardless of the surgical approach. One system that can classify severity in complications is the Clavien Classification of Surgical Complications (CCSC).7,8
In studies conducted with the Clavien classification, the presence of complications in open nephrectomy range from infections, which are the most common (52% of grades I and II), to scarring problems (12%) and neurological alterations (9%). The most common infection in the group of minor complications was pneumonia (43% of grade II complications). Intervention was required in 5% more commonly secondary to wound dehiscence (40%), retroperitoneal abscess (30%) or ileus (20%). Admission to intensive care occurred in 3%, and this was secondary to respiratory failure secondary to pneumonia.7,8
For this reason, a study was conducted in patients who underwent nephrectomy secondary to lithiasis, where it was intentionally sought to observe the factors that lead to admission to the intensive care unit.
ObjectiveTo describe the results of simple retroperitoneal open nephrectomies secondary to lithiasis in Hospital General de México “Dr. Eduardo Liceaga” and to determine the factors associated with admission to the intensive care unit.
MethodologyThe patient information needed to analyze this work was collected in Hospital General de México “Dr. Eduardo Liceaga”. Records were searched in the clinical file that were in line with the ICD-9 code for nephrectomy, in the period from January 2010 to May 2016. A total of 110 files from patients who underwent open nephrectomies were evaluated. 52 patients were excluded because they did not have a lithiasis diagnosis. A total of 58 patients with a diagnosis of renal exclusion confirmed by renal scintigraphy, and lithiasis, who underwent simple nephrectomy by a group of expert surgeons were included. In all patients, a retroperitoneal approach was performed by lumbotomy; all patients had antibiotic cover at the time of surgery.
A retrospective analysis was conducted within a cohort of patients undergoing simple nephrectomy. A total of 58 patients were evaluated, who were included for the statistical analysis. Descriptive statistics were measured for the demographic variables. Inferential statistics were evaluated in quantitative variables using Student's T-test, with a p<0.005. For the qualitative variables the Chi square test was used. SPSS version 21 software was used to conduct the statistical analysis.
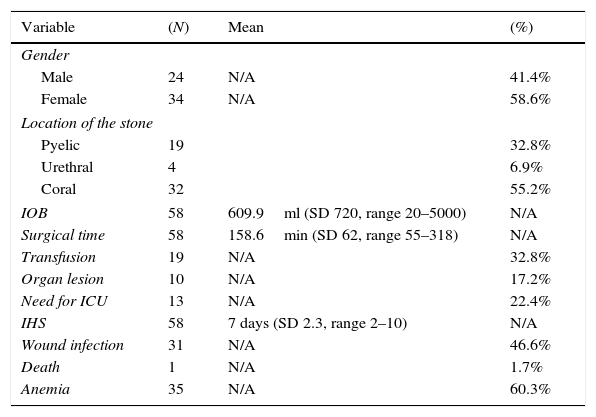
ResultsThe total population consisted of 58 patients with a history of open simple nephrectomy. There were 24 male (41.4%) and 34 female (58.6%) patients. The mean age was 46 years (SD 14.1). The location of the stone was pyelic 32%, urethral 6.9% and coral 55.2%. Regarding transoperative variables, the mean transoperative bleeding was 604.9ml (SD 720, range 20–5000ml) and the mean surgical time, taken from the incision of the skin to wound closure was 158.6min (SD 62, range 55–318). The postoperative variables were as follows: Nineteen patients required transfusion (32.8%) (Clavien-Dindo II), ten patients had vascular or solid organ lesion during surgery, (17.2%) (Clavien-Dindo III b) and thirteen patients were admitted to the intensive care unit (22.4%) (Clavien-Dindo IV). The mean hospital stay was 7 days (SD 2.3, range 2–10), thirty-one patients had a surgical wound infection (46.6%) (Clavien-Dindo II) and one patient died (1.7%) (Clavien-Dindo V). The population studied had a normal distribution (Table 1).
Descriptive statistics for 58 postoperative patients with simple retroperitoneal nephrectomy secondary to lithiasis.
| Variable | (N) | Mean | (%) |
|---|---|---|---|
| Gender | |||
| Male | 24 | N/A | 41.4% |
| Female | 34 | N/A | 58.6% |
| Location of the stone | |||
| Pyelic | 19 | 32.8% | |
| Urethral | 4 | 6.9% | |
| Coral | 32 | 55.2% | |
| IOB | 58 | 609.9ml (SD 720, range 20–5000) | N/A |
| Surgical time | 58 | 158.6min (SD 62, range 55–318) | N/A |
| Transfusion | 19 | N/A | 32.8% |
| Organ lesion | 10 | N/A | 17.2% |
| Need for ICU | 13 | N/A | 22.4% |
| IHS | 58 | 7 days (SD 2.3, range 2–10) | N/A |
| Wound infection | 31 | N/A | 46.6% |
| Death | 1 | N/A | 1.7% |
| Anemia | 35 | N/A | 60.3% |
IOB, intraoperative bleeding; ICU, intensive care unit; IHS, intra-hospital stay.
The dependent variables of our study were the presence or absence of complications, as well as the stay in the intensive care unit. When the Chi square test was performed between the presence of complications and the independent variables, transfusion was identified as a factor associated with developing complications (p: 0.001). The variables anemia, lithiasis, presence of preoperative abscess, smoking, hypertension and diabetes were not associated with the development of postoperative complications (p>0.005).
The variables that presented an association with stay in the intensive care unit were: anemia (p: 0.007), systemic hypertension (p: 0.004), diabetes mellitus (p: 0.021) and the need for transoperative transfusion (p: 0.001).
The group of patients who were in intensive therapy had greater bleeding. (Mean ICU bleeding 987ml vs 494ml with p: 0.029). They also had a greater weight (61 vs 69kg, p: 0.046). There were no differences in age, height and surgical time.
When the multivariate analysis was performed among the following variables: age, weight, height, diabetes mellitus, systemic hypertension, smoking, abscess and transfusion, it was not possible to identify a correlation between these and the development of complications or admission to the intensive care unit. However, when the relationship between transfusing a patient and the development of complications was assessed by logistic regression, a positive ratio was found with p: 0.003, and OR 13.45 CI [2.4–72]. Patients who suffered complications required a longer stay in the intensive care unit (p=0.002).
DiscussionIn the present study, patients who presented comorbidities such as hypertension, diabetes mellitus and anemia were the ones that were more likely to require a stay in the intensive care unit, but those that were characterized with a higher incidence of admission were those who had undergone transoperative transfusion.
In this study, no significant relationship regarding weight and height was observed in patients who were admitted to intensive care.
Organizations such as the National Institute of Health (NIH) and American College of Physicians even mention that in patients who do not present a critical disease, or in those who do not present heart disease, the cut-off point of transfusion should be with hemoglobin levels of 7.0–8.0g/dl. For patients with a critical disease or presence of cardiovascular disease, the cut-off point can be considered at 9g/dl.9–11
In a study conducted by Bachar Zelhof et al. it was observed that patients that underwent simple nephrectomy due to lithiasis tended to have more comorbidities than those that underwent radical nephrectomy; this may be related to the presence of adhesions secondary to chronic inflammation, as well as infections secondary to the underlying lithiasis.3
For this reason it has been referred to as benign nephrectomy rather than simple nephrectomy, since on multiple occasions it tends to be much more or just as complicated to perform this procedure compared to a radical nephrectomy.14
At present, no specific consensus has been reached on how to report a surgical complication; therefore, the use of the Clavien classification continues to be supported for this reason. Patients that are post-surgically admitted to an intensive care unit are included within the Clavien Dindo IV classification, which refers to conditions that threaten the life of the patient.2
Likewise, the lack of clinical guidelines that promptly indicate the use of transsurgical transfusions leads to this procedure, depending on hemoglobin levels. A greater number of studies are therefore required in order to determine the use of this procedure with the lowest probability of presenting comorbidities.12,13,15
In the literature, there is no relationship between the use of transsurgical transfusion and the risk of admission to an intensive care unit. Also, studies have only been conducted regarding transsurgical transfusion in patients that underwent partial or radical nephrectomy in patients with tumoral pathology. Randomized clinical trials are needed to compare the difference in bleeding and transfusion requirements between a transperitoneal abdominal technique and the one used in our retroperitoneal lumbotomy population to determine the impact of the technique on transoperative bleeding, since as of today there are only comparisons in laparoscopic surgery in which there was no significant difference.16
ConclusionIt was observed that patients with comorbidities such as hypertension, diabetes mellitus and anemia are more likely to require management in the intensive care unit. This probability is even greater in those that required transsurgical transfusion. As there are not enough studies that relate the different risk factors that require management in the intensive care unit, it is still not possible to speak of a risk classification or transsurgical transfusion indications in these patients.
Ethical disclosuresProtection of person and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors of this paper state that they have no conflicts of interest.