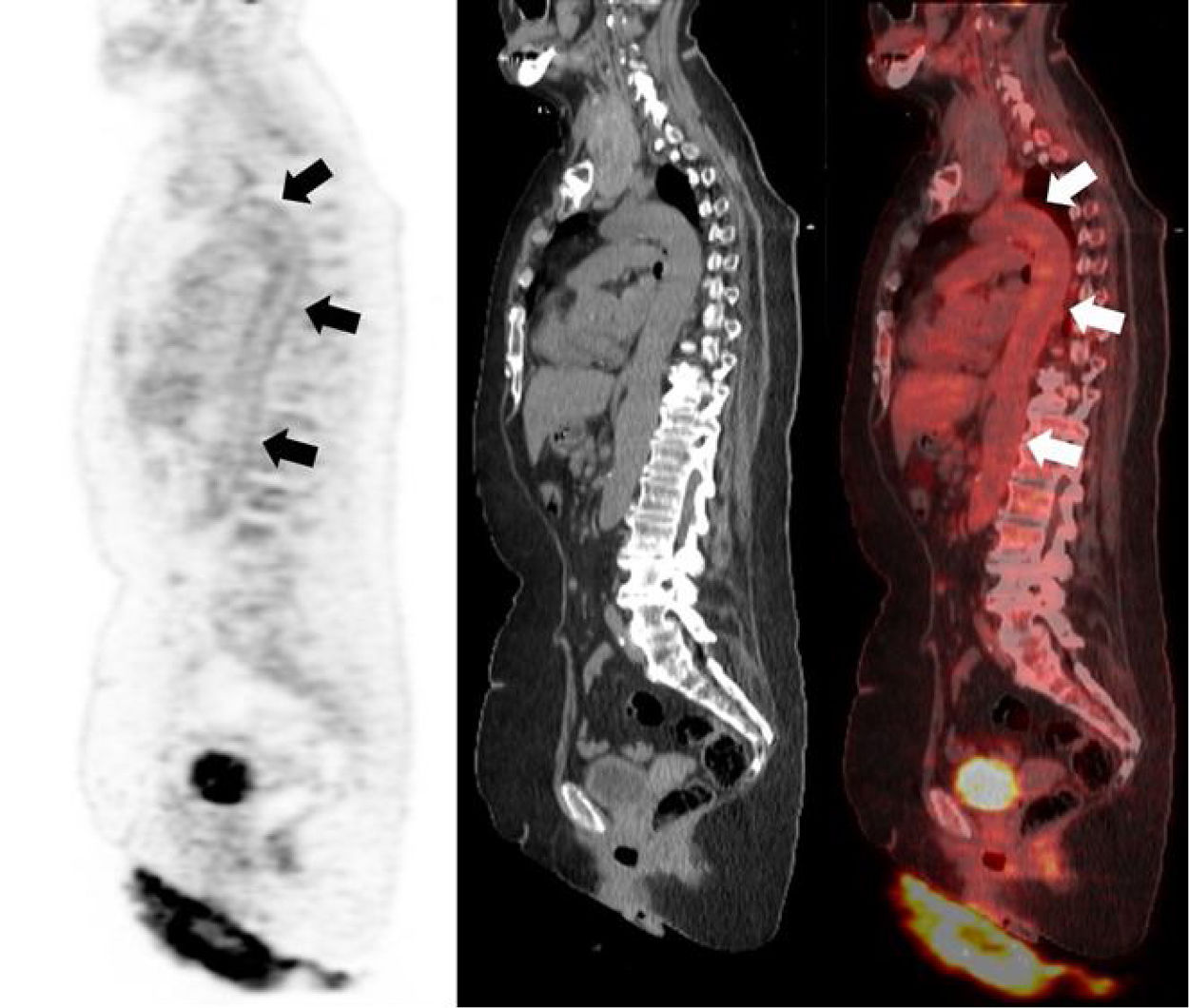
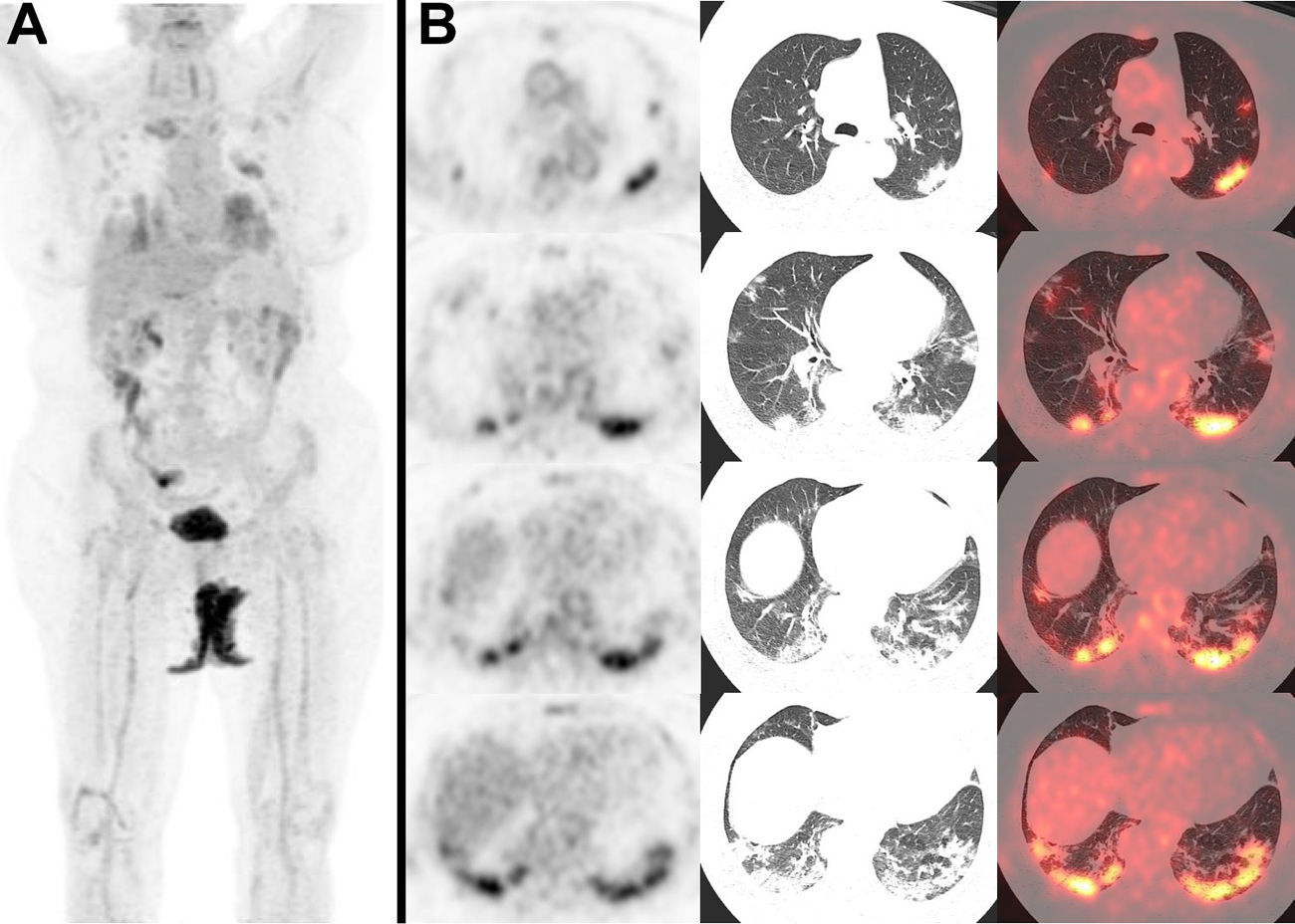
A 69-year-old woman diagnosed of ischemic stroke of the basal ganglia and no respiratory symptoms had a blood test with leukocytosis with left shift, increased acute phase reactants, high levels of d-dimer and antithrombin III deficiency. Cranial magnetic resonance imaging was consistent with cerebral vasculitis and a computed tomography angiography showed narrowing of the left subclavian artery. Due to the clinical suspicion of a systemic vasculitis, a 18F-FDG PET/CT study was performed, showing a diffuse increased glucose metabolism in the wall of main arterial vessels, suggesting a large vessel vasculitis (Fig. 1). As an incidental finding, bilateral multifocal lung lesions were detected, especially in the lower lobes, with ground glass opacifications and increased 18F-FDG uptake, consistent with bronchopneumonia (Fig. 2). In the context of the world 2019 coronavirus disease (COVID-19) pandemic, these findings were interpreted as suspicious of coronavirus SARS-CoV-2 pneumonia, so the patient underwent both nasal and throat swab polymerase chain reaction (PCR) tests, with negative results on three different occasions, and a serology test for IgM and IgG anti-SARS-CoV-2 antibodies, with a positive result indicating active infection. The patient was isolated for two weeks and developed no symptoms during that period.
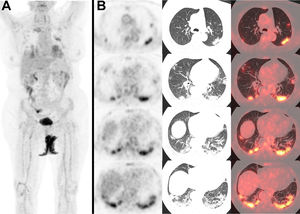
A) Maximum intensity projection showing hypermetabolic foci in both lungs. B) Axial views of PET images (left), CT (center), and PET/CT image fusion (right) showing bilateral multifocal lung lesions with ground glass opacifications, especially in the lower lobes, with some consolidation areas in the posteriorbasal segments, and increased glucose metabolism (SUVmax left lower lobe 11,69), consistent withbronchopneumonia.
Patients infected with coronavirus SARS-CoV-2 are usually asymptomatic or present unspecified symptoms, like fever, asthenia or dry cough.1 The most serious clinical manifestation is viral pneumonia, often requiring hospitalization, or even ventilatory support on severe cases, like acute respiratory distress syndrome.1 Chest X-ray is not recommended for the diagnosis of SARS-CoV-2 pneumonia due to its low sensibility in comparison with chest CT, which is the preferred imaging technique. The most frequent findings on CT are ground glass opacifications (72%), that can be bilateral in more than half of the cases, and sometimes associated with consolidations (13%) or crazy paving pattern (12%).1 Other associated findings are linear opacities (61%), adjacent pleura thickening (56%) and interlobular thickening (37%).1 SARS-CoV-2 lung lesions show increased 18F-FDG uptake, and can be associated with mediastinal or supraclavicular hypermetabolic lymph nodes.2 No disseminated extrapulmonary lesions from coronavirus SARS-CoV-2 have been yet reported with 18F-FDG PET/CT, suggesting that this virus may have specific lung tropism, although there is still a limited number of cases described.2
In the context of the COVID-19 pandemic, the detection of suspicious findings of pneumonia on CT or PET/CT, in both symptomatic or asymptomatic patients, requires further investigation by performing specific PCR and antibody serology tests. In our case, SARS-CoV-2 pneumonia was confirmed on the basis of PET/CT imaging and antibody serology, despite the absence of respiratory symptoms and the negativity of PCR tests. Although an association between SARS-CoV-2 coronavirus infection and mid-vessel vasculitis in children (Kawasaki disease)3 has been reported, to date no studies have been published linking directly or indirectly this infection with large vessel vasculitis in adult patients. Therefore, it cannot be assumed in our case that they were two independent nosological entities, as long as there is no advanced knowledge about this new viral infection.
Please cite this article as: Salvat Dávila C, Suárez Fernández JP, Domínguez Grande ML, Vigil Díaz C, Fernández Llana B, Martín Fernández N. Neumonía por SARS-CoV-2 (COVID-19): Hallazgo casual en estudio PET/TC con 18F-FDG para el diagnóstico de vasculitis. Rev Esp Med Nucl Imagen Mol. 2021;40:251–252.