Talar fractures are uncommon lesions (0.1–0.9%) and have a high rate of complications. One of the situations in which a fracture of the talus can occur is in the context of polytrauma which may further compromise the functional prognosis.
The aim of this study was to analyse the functional results in patients with talar fractures whether or not they occurred in the context of polytrauma.
Observational study on a retrospective cohort of 24 patients operated in our centre (2008–2016). They were grouped according to whether they were polytraumatized (ISS>16) or not (ISS≤16). Review of sociodemographic, radiographic, functional variables (VAS pain scale and FADI –Foot and Ankle Disability Index) and the onset of complications such as arthrosis, arthrodesis or avascular necrosis.
Review of 25 talar fractures in 24 patients with a mean age of 38 years (19–75) and a mean follow-up of 4.2 years (0.5–9). According to the ISS, 44% of patients (11) were polytraumatized and 56% (14) were not.
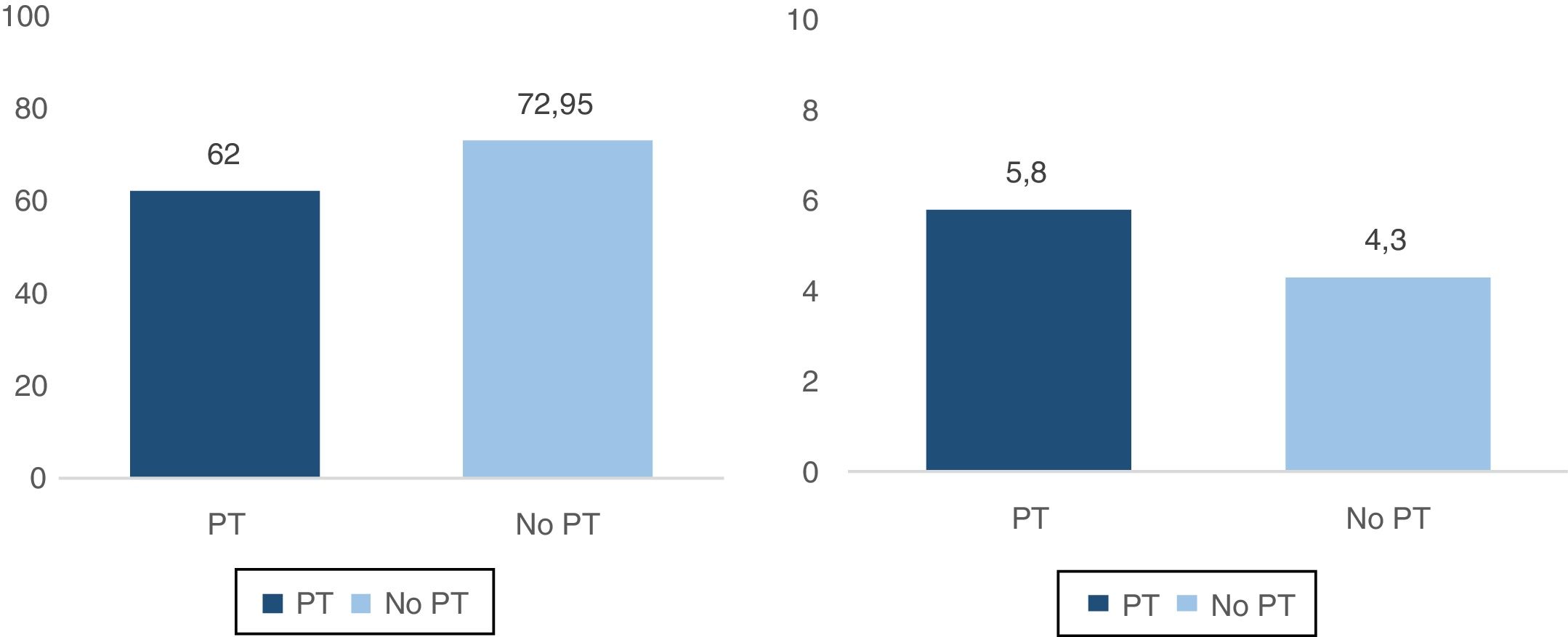
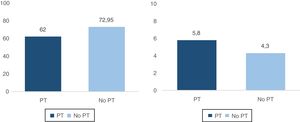
The average score according to the FADI scale was 62 points for the polytraumatized patients and 76.9 for the non-polytraumatized patients. The pain according to the VAS scale was 5.8 points in the group of polytraumatized patients and 4.3 in the non-polytraumatized patient group.
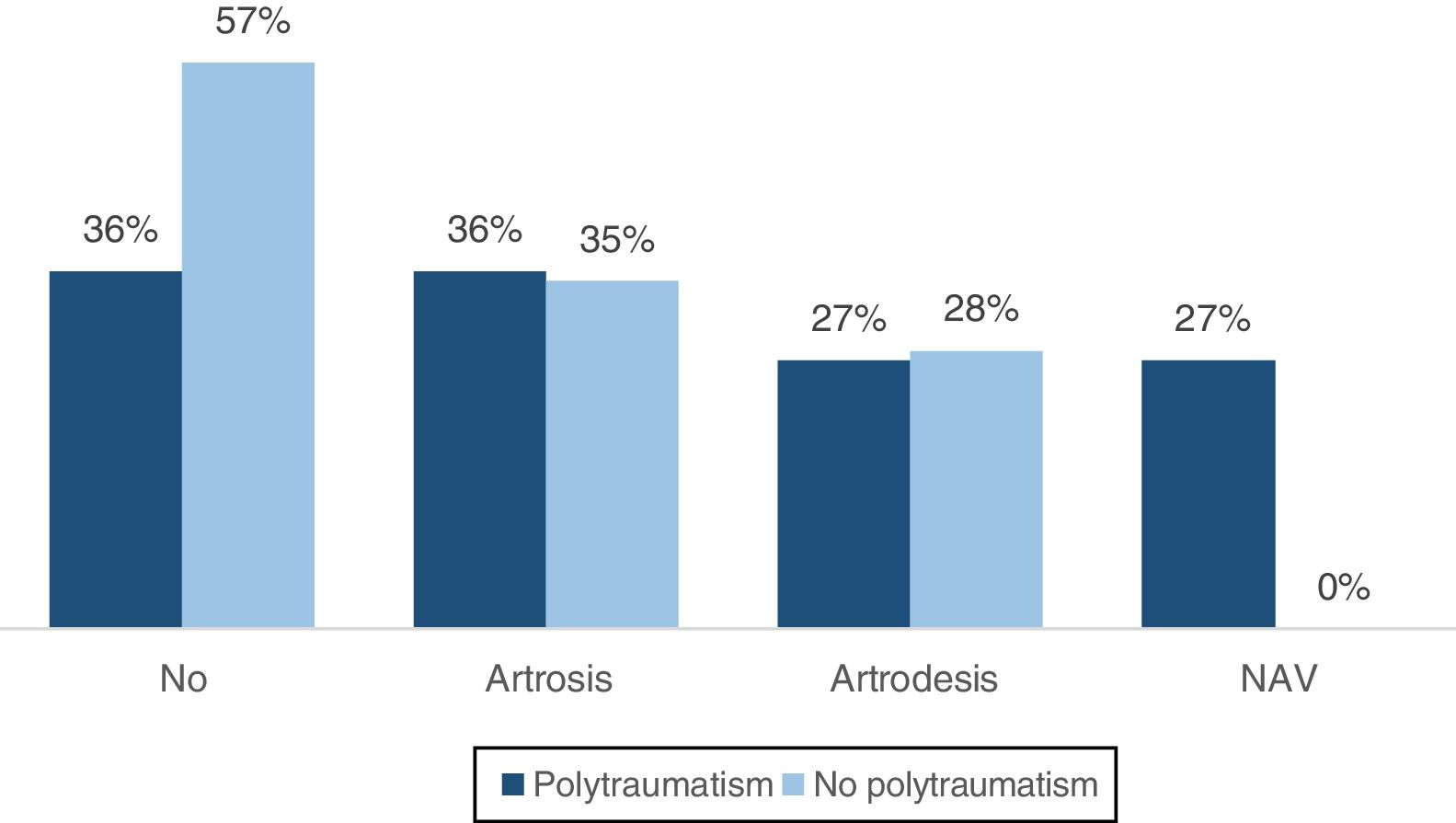
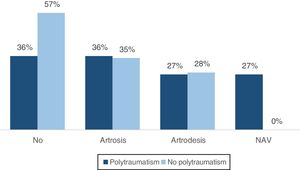
Regarding complications, 64% of the polytraumatized patients and 43% of the non-traumatized patients had a complication. 36% of the polytraumatized patients had clinical and radiological signs of subtalar arthrosis compared to 35% of the non-traumatized patients, of whom 27% underwent arthrodesis compared to 28% of the non-traumatized patients. 27% of the polytraumatized patients were diagnosed with avascular necrosis as opposed to 0% of the non-polytraumatized patients.
Las fracturas de astrágalo son lesiones poco frecuentes (0,1-0,9%) y con un alto índice de complicaciones. Una de las situaciones en las que puede darse una fractura de astrágalo es en el contexto de un politraumatismo, lo que puede comprometer aún más el pronóstico funcional.
El objetivo del presente trabajo ha sido analizar los resultados funcionales en los pacientes con fracturas de astrágalo según se produjeran en el contexto de un politraumatismo o no.
Estudio observacional sobre una cohorte retrospectiva de 24 pacientes intervenidos por fractura de astrágalo en nuestro centro (2008-2016). Se agruparon según fuesen politraumatizados (ISS>16) o no (ISS≤16). Revisión de variables sociodemográficas, radiográficas, funcionales (escala EVA de dolor y FADI –Foot and Ankle Disability Index–) y la aparición de complicaciones como artrosis o necrosis avascular.
Revisión de 25 fracturas de astrágalo en 24 pacientes con una edad media de 38 años (19-75) y un seguimiento medio de 4,2 años (0,5-9). Según el ISS un 44% de pacientes (11) fueron politraumatizados y un 56% (14) no.
Respecto a los resultados funcionales entre politraumatizados y no politraumatizados, la puntuación media según la escala FADI fue de 62 puntos y de 76,9 respectivamente y según la escala EVA fue de 5,8 y 4,3 puntos respectivamente.
Respecto a las complicaciones, en el grupo de politraumatizados se presentaron en un 64% de los pacientes y en los no politraumatizados en un 43%. Un 36% de los pacientes politraumatizados tuvieron signos clínicos y radiológicos de artrosis subastragalina y un 27% fueron intervenidos mediante una artrodesis frente al 35% y al 27% del grupo de no politraumatizados, Respecto a la necrosis avascular del astrágalo, se registro un 27% frente a un 0% de los no politraumatizados.
Talus fractures are one of the most severe ankle fractures due to the difficulty of treatment and the major sequelae they may cause. Fractures of this type are not very common, at around 0.1–0.85% of fractures of the human body and approximately 3% of those affecting the foot. This is because the talus is very well protected by the bone and ligament covering that keeps it in its anatomical position. Although there are not many such fractures, they are highly important in prognostic and social terms due to their associated high rate of complications and functional sequelae.1
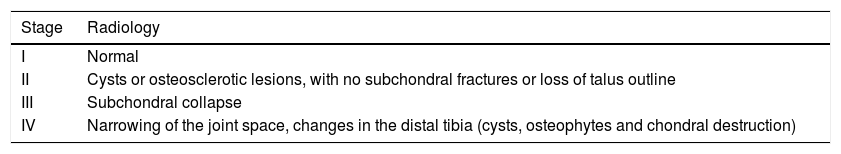
The high rate of complications2 has been associated historically with the poor vascularisation and peculiar anatomy of this tarsal bone, with more than 60% of its surface covered in joint cartilage. However, in recent years studies have shown that it does not have such poor vascularisation.3–5 The most important complications include arthrosis of one of the neighbouring joints, which often have to be treated by arthrodesis, and avascular necrosis (AVN).6 Talus neck fractures may be classified according to Hawkins’ classification, which we describe below, and we will be able to know the probabilities of one of these complications arising according to the type of fracture in question.7
Fractures of this type are usually secondary to high energy trauma,8 generally traffic accidents and falls from a great height, so that they may occur within the context of multiple trauma that, for many reasons, may compromise the functional prognosis even more. This is because of the need for surgery to control injuries and bring about initial stabilisation, and this usually delays the definitive osteosynthesis of the talus.
The aim of this study was to analyse the functional results and clinical evolution of patients operated on in our hospital for talus fractures, regardless of whether or not they occurred within the context of polytraumatism.
Material and methodAfter approval by the hospital ethics committee an observational study was performed of a retrospective cohort of 24 patients operated on for talus fracture in our hospital from March 2008 to June 2016. All of the patients were evaluated during a visit or telephonically at the end of follow-up, and they were informed that their data would be used in the study.
All of the patients operated on in the hospital for talus fracture were included, regardless of whether an open reduction with internal fixation or closed reduction and internal fixation had been performed, independently of the osteosynthesis executed9–12 (Kirschner needles or cannulated screws). The time lapse from the moment of the fracture to the surgical operation was also recorded. Cases of pure luxation of the talus or posttraumatic osteochondral lesions of the same were excluded.
The sociodemographic variables reviewed were age at the moment of injury, sex, patient comorbidities and whether or not they were smokers at the time of the fracture.
All of the fractures were classified radiographically by simple X-ray and CT13,14 according to Hawkins’ classification.15 Type I, fractures without displacement; type ii, fractures with associated luxation or subluxation of the subtalar joint; type iii, with luxation of the subtalus and tibiotalar joint; and type iv, which adds luxation of the talar-scaphoid joint to the others. All types of fracture were included in the study. Records were also kept of whether lesions were open or closed.
The Injury Severity Score (ISS)16 scale was used to define the 2 main groups in the study: ISS>16 for polytraumatised patients and ISS≤16 points for those who were not polytraumatised. Other data recorded were the other types of injuries in polytraumatised patients13 (CET, facial injuries, abdominal injuries, pelvic or spinal trauma, thoracic trauma and associated fractures).
Evaluation of functional resultsThe Analogue Visual Scale (AVS) was used to make it possible to analyse the results of these interventions. This enables measurement of the pain felt by patients subjectively on a scale from 0 to 10, where 0 is the absence of pain and 10 is the maximum possible pain. Postoperative functionality was evaluated using the Foot and Ankle Disability Index (FADI).17 This questionnaire was designed to evaluate the functional limitations arising due to foot and ankle pathologies, taking into account pain and the difficulty in performing certain everyday activities. FADI scores run from 0 to 100, where 100 is no discomfort or difficulty for any of the activities asked about, and 0 is complete disability and unbearable pain for the activities recorded.
Finally the appearance of the most frequent complications following talus fracture were recorded during follow-up; development into clinically significant arthrosis, the need for arthrodesis in any of the neighbouring joints or the development of AVN in the same. The absence of Hawkins’ sign18 was used to diagnose necrosis, and a MR scan was taken in all cases.19 The Ficat and Arlet AVN scale was used, modified for the ankle and based on radiology (Table 1).
The data from both scales and the record of complications were compiled in surgeries after the consent of the patient at the time of undertaking this study, so the time of evolution coincides with the follow-up time, which amounted to an average of 4.2 years (.5–9 years).
ResultsDemographic data24 patient cases were reviewed, with 25 talus fractures (one case of bilateral fracture is included) in the period from March 2008 to June 2016, operated on in our hospital and with an average age of 38 years old (19–75 years old). The average follow-up time was 4.2 years (.5–9 years).
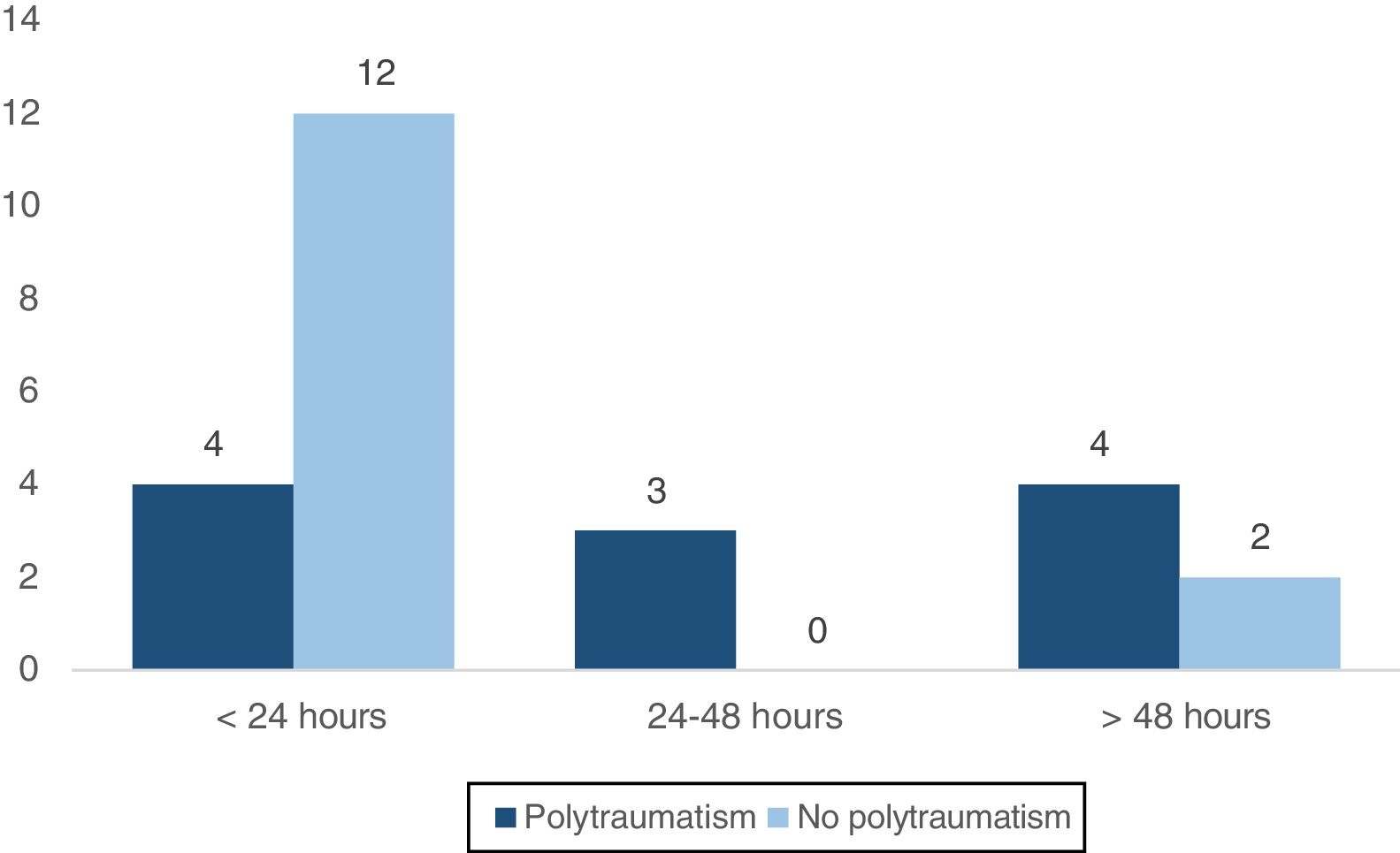
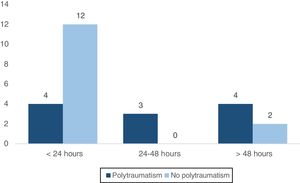
Talus fractures are considered to be an emergency according to current evidence.20 In this study 64% (16/25) of talus fractures were operated on in less than 24h, 12% were operated on from 24h to 48h, and 24% (6/25) were operated on after more than 48h. The last group includes 4 cases that have a delay of more than 2 days in their diagnosis.
According to Hawkins’ classification, 12% (3) of the fractures were type i, 32% (8) were type ii, 32% (8) were type ii and 16% (4) were type iv. There was only one case (4%) of an open lesion.
According to the ISS16 and classifying the patients as polytraumatised (ISS>16) or not polytraumatised (ISS≤16) 56% of patients were found to be polytraumatised (14) while 44% of patients (11) had suffered an isolated talus fracture. The average ISS score was 18 (13–48).
The most common associated lesion in the group of polytraumatised patients was pelvic or spinal trauma; in 63% of cases (7/11) in our series talus fracture was associated with fracture of the pelvic ring or spinal column. In 45% of patients (5/11) with an ISS>16 the diagnosis was accompanied by thoracic trauma involving rib or sternum fracture, and in 27% there was associated CET.
No complications were recorded in 48% of patients during follow-up, while 36% (9) developed arthrosis, of which 12.5% (5) were operated for arthrodesis and 12% developed AVN.
At the time of the examination the average score recorded on the AVS was 4.96, within a range of from 0 to 9. The average score on the FADI17 was 70 points (29–100).
Data analysisOnce the 24 patients had been divided into the 2 groups described above of polytraumatised and non-polytraumatised patients, they were examined and the distribution of the variables recorded was analysed.
Descriptive statistical analysis was performed using SPSS® v.20 (IBM Chicago, IL, U.S.A.) software, with core tendency and dispersion measurements for quantitative variables and frequency distribution for qualitative variables. Bivariate analysis of the distribution between groups was applied, where the grouping variable was whether or not patients were polytraumatised. The chi-squared test was applied to qualitative variables and the Mann–Whitney U test was used for quantitative variables. The limit of significance was set at P<.05.
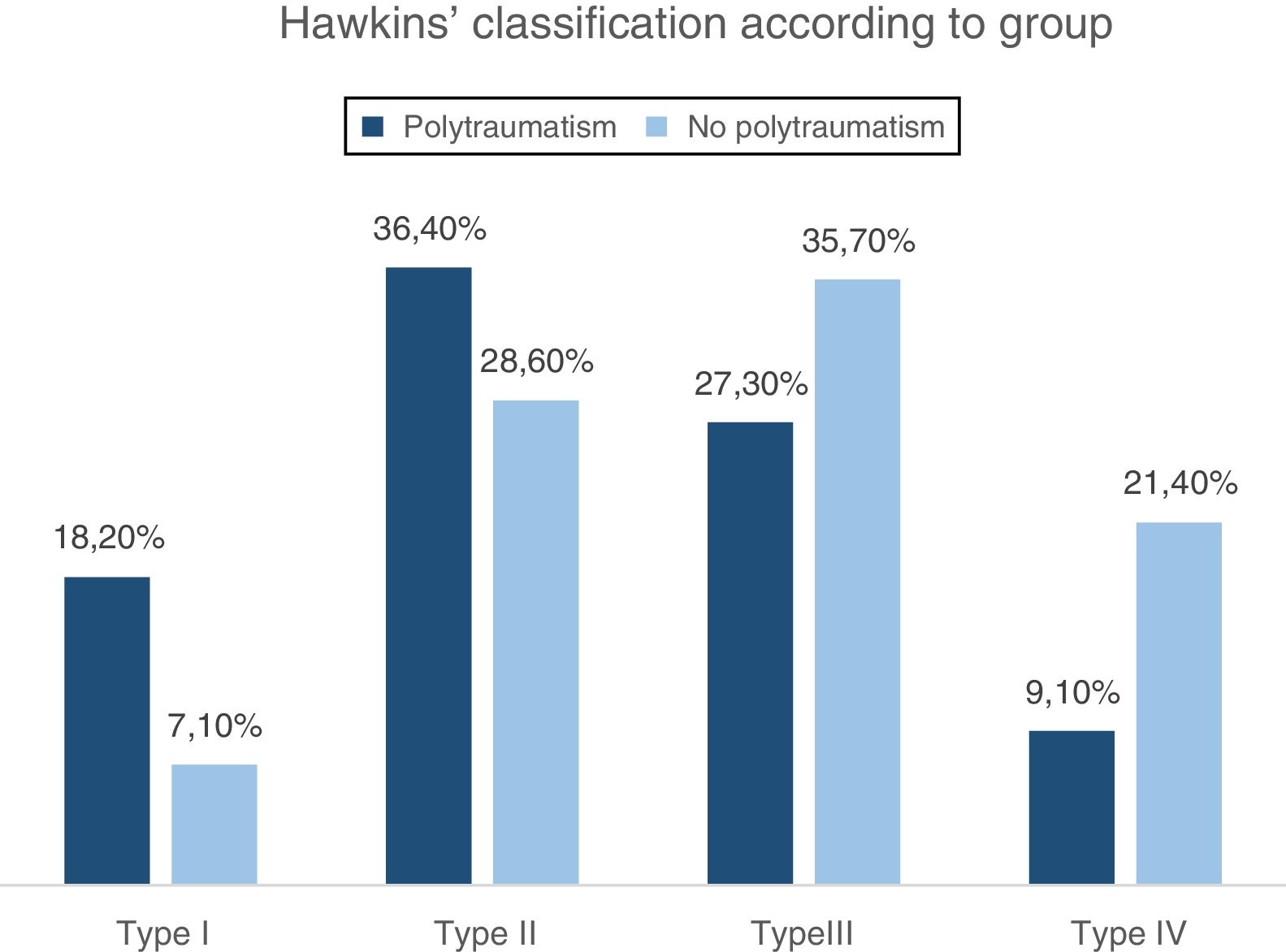
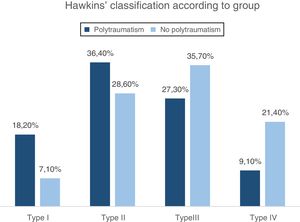
A similar distribution between both groups was found for the Hawkins’ classification (Fig. 1): type i 18.2% in polytraumatised patients vs 7.1% in non-polytraumatised patients; type ii 36.4% in polytraumatised patients vs 28.6% in non-polytraumatised patients; type iii 27.3% in polytraumatised patients vs 35.7% in non-polytraumatised patients, and type iv 9.1% in polytraumatised patients vs 21.4% in non-polytraumatised patients. These differences were not statistically significant.
Respecting surgical delay (Fig. 2), in non-polytraumatised patients 85.7% were operated on in less than 24h vs 36.4% of polytraumatised patients. No non-polytraumatised patient was operated on after a delay of from 24h to 48h, while 3/11 (36.4%) of the polytraumatised patients were operated on in this period. As was pointed out above, 6 patients were operated on more than 48h after the fracture occurred, in the majority of cases due to delayed diagnosis. 2 of these patients were non-polytraumatised (14.3%) and 4 were polytraumatised (36.4%). No statistically significant differences were found in terms of surgical delay between both groups.
Respecting the evaluation of the functional results for the groups on the FADI17 scale (Fig. 3a) the score was 62/100 in the polytraumatised patients and 76.95/100 in the non-polytraumatised patients (P=.232). The score on the AVS (Fig. 3b) was 5.8 in the group of polytraumatised patients and 4.3 in the non-polytraumatised patients (P=.257).
When the frequency of complications was analysed (Fig. 4) according to the group in which patients were assigned, it was found that 57% of the patients with an isolated talus fracture developed no adverse events, while only 36% of the patients who suffered such a fracture in the context of polytraumatism did not develop any associated complications. 35% of the group of non-polytraumatised patients% (5/14) had clinical and radiological signs of arthrosis in one of the neighbouring joints, of which 28% (4) required arthrodesis in one of them. These figures are similar to those for polytraumatised patients, of which 36% (4/11) had arthrosis and 27% (3) required arthrodesis. Fig. 4 shows the accumulated percentage to be higher than 100% because the “arthrosis” heading included the patients subjected to arthrodesis due to arthrosis.
None of the patients included in the group of non-polytraumatised patients has been diagnosed AVN at the time of this study, while 27% of the polytraumatised patients (3/11) have satisfied criteria for the diagnosis of tarsal AVN.
No statistically significant differences were found between both groups in terms of the appearance of complications.
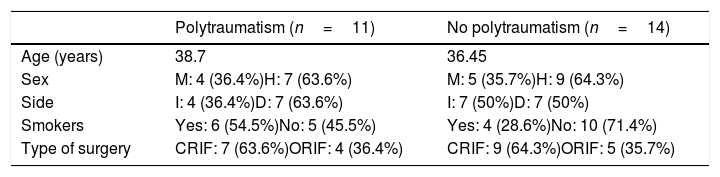
No statistically significant differences were found between the other sociodemographic variables (age, sex, smoker/non-smoker or the side of the fracture) (Table 2).
Variables studied in both groups.
| Polytraumatism (n=11) | No polytraumatism (n=14) | |
|---|---|---|
| Age (years) | 38.7 | 36.45 |
| Sex | M: 4 (36.4%)H: 7 (63.6%) | M: 5 (35.7%)H: 9 (64.3%) |
| Side | I: 4 (36.4%)D: 7 (63.6%) | I: 7 (50%)D: 7 (50%) |
| Smokers | Yes: 6 (54.5%)No: 5 (45.5%) | Yes: 4 (28.6%)No: 10 (71.4%) |
| Type of surgery | CRIF: 7 (63.6%)ORIF: 4 (36.4%) | CRIF: 9 (64.3%)ORIF: 5 (35.7%) |
An observational study was performed on a retrospective cohort of 25 talus fractures operated on in our hospital. A series of demographic variables were recorded and the patients were divided into 2 groups, of polytraumatised patients and non-polytraumatised patients, according to the ISS classification. After this division the functional results were studied, together with the incidence of complications in both groups.
Treating talus fractures is still a challenge for surgeons, and they continue to arouse a high level of interest due to the impact which the results of treatment may have on patients’ quality of life.
In this study the average AVS and FADI scores showed better results in the group with isolated talus fracture. The polytraumatised patients had an average AVS of 5.8 vs 4.3 in the other group, showing that there is a certain tendency in our sample for the polytraumatised patients to feel greater subjective residual pain. The statistical analysis of these data gave a value of P=.257, so that we can conclude that the differences are not statistically significant.
As was the case for pain, the functional results recorded in this work by the FADI scale also show worse results in the group of polytraumatised patients. More specifically, the average FADI score in the polytraumatised patients was 76.95/100 vs 62/100 in the group of non-polytraumatised patients. Following statistical analysis of these data the conclusion was reached that the differences were not statistically significant, as P>.05 (P=.232), probably due to the small size of the sample. In any case a tendency was detected for polytraumatised patients with talus fractures to have greater functional sequelae in the extremity.
The other aspect analysed was comparison of the incidence of complications associated with talus fracture between both groups. In our series 43% of the patients with isolated talus fracture developed some type of adverse event prior to the date of the study, vs 64% of the polytraumatised patients. The incidence of AVN was also analysed, and none of the patients with isolated talus fracture developed this complication while 3 of the 11 fractures in the group of polytraumatised patients fulfilled the diagnostic criteria for AVN of the talus. This last complication, talar AVN, is the result of fracture of the neck or head of the talus in 75% of cases.19 It gives rise to a major challenge for the surgeon because of the same factors that were described above, the precarious vascularisation and anatomical arrangement of this bone. Up to 31% of talus fractures eventually develop this complication of AVN.6
Talar AVN is a cause of ankle fracture that is hard to diagnose, and it is often the consequence of fracture of the talus. Talar osteonecrosis arises when there is a reduction in the vascular supply to the talus and the bone is deprived of its source of oxygen. This may occur alone or in association with bone loss, collapse, sepsis, deformity and severe arthritis of the neighbouring joints.21
Based on these data it can be said that there is a certain tendency for the prognosis in talus fractures to be worse in the context of multiple trauma, and it would be necessary to study the possible causes of this. One of the proposed causes is the increased delay prior to surgery, as polytraumatised patients have to be stabilised beforehand, together with other emergency procedures. Although some papers2,22,23 find no differences in terms of functional results or the rate of complications depending on the time lapse between a fracture and its definitive fixation, in our series there is a tendency for the delay to be longer in polytraumatised patients, so that this hypothesis may explain our results. However, the said studies2,22,23 consider any type of open fracture to be a surgical emergency, together with reduction in the case of luxation.
The purpose of this study was to determine the differences in the functional results of talus fractures operated on in polytraumatised patients and others with an isolated talus fracture. Other factors were also studied, as they may influence the functional results and possible complications. Follow-up was achieved with only one loss, and a sufficiently large sample size was achieved for analysis of both groups. It should also be pointed out that the type of sample stratification used of polytraumatised and non-polytraumatised patients, would require a study with a larger sample to make it possible to draw significant conclusions in the resulting analyses.
No differences were found in the results obtained according to fracture type according to Hawkins’ classification or the sociodemographic variables studied (age at the time of trauma, sex, patient comorbidities and whether or not they smoked or when the fracture occurred).
This study found less a favourable clinical evolution and functional results in patients with talus fracture in the context of multiple traumas, in comparison with the patients with an isolated fracture that was operated on. The former scored 1.5 points worse on the AVS and 14.95 points less on the FADI.
Thanks to the introduction of the damage control concept in the treatment of polytraumatised patients, their morbidity and mortality have declined in recent decades. The lesions that traditionally have a poor prognosis and which may lead to severe functional restriction over the long term, such as talus fractures, requires therapeutic optimisation in polytraumatised patients to improve their clinical results over the long term.
With all of these arguments we may conclude that it is necessary to optimise the management of talus fractures in the emergency department in polytraumatised patients, to improve the results of surgical treatment.
Level of evidenceLevel of evidence II.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Hierro-Cañas FJ, Andrés-Cano P, Rabadán-Márquez G, Giráldez-Sánchez MA, Cano-Luis P. Fracturas de astrágalo. Resultados funcionales en pacientes politraumatizados. Rev Esp Cir Ortop Traumatol. 2019;63:336–341.