We describe an unusual case of axillary vein thrombosis after extensive muscular and fibrillar rupture of the long tendon of the right biceps brachii in a 43-year-old patient after an effort. The difficult diagnosis of this condition requires high suspicion and early treatment.
Describimos un caso inusual de trombosis en la vena axilar tras una rotura fibrilar extensa, muscular y parcial del tendón largo del bíceps braquial derecho, en un paciente de 43 años tras la realización de un sobreesfuerzo. Esta afección supone un difícil diagnóstico, por lo que requiere una alta sospecha y un tratamiento temprano.
Injury to the biceps long tendon is very common, especially in people over 40 years of age.
By contrast, deep vein thrombosis of the upper extremity (UEDVT) is a much less frequent condition, constituting 1–4% of all DVT, whose incidence in the general population is estimated at 1.92 cases per 1000 inhabitants/year. Two types are differentiated: primary or spontaneous, in which the exact mechanism of production is unknown,1,2 and secondary. This second group is the most frequent (80%), and the known causes include the use of intravenous catheters, neoplasms, thrombophilia, clavicular fractures, thoracic outlet syndrome, or following arthroscopic shoulder procedures.3–5
Our aim is to bring this rare complication to light which, if undetected and not treated in time, could result in fatal complications.
Clinical caseA 43-year-old male patient, a painter with a personal history of high blood pressure and hyperuricaemia, and no other history of interest. The patient was admitted through the emergency department due to pain and haematoma in the right arm of one week's evolution, which was progressively worsening. He reported a history of indirect trauma at work, noticing a “snap” at the level of his shoulder. On physical examination, haematoma was seen on the medial surface of the arm up to the anterior flexure of the elbow, and increased local temperature, pain during passive and active mobilisation, especially when performing internal rotation of the shoulder and flexion of the arm; positive Popeye sign. Anteroposterior and axial shoulder radiography were normal.
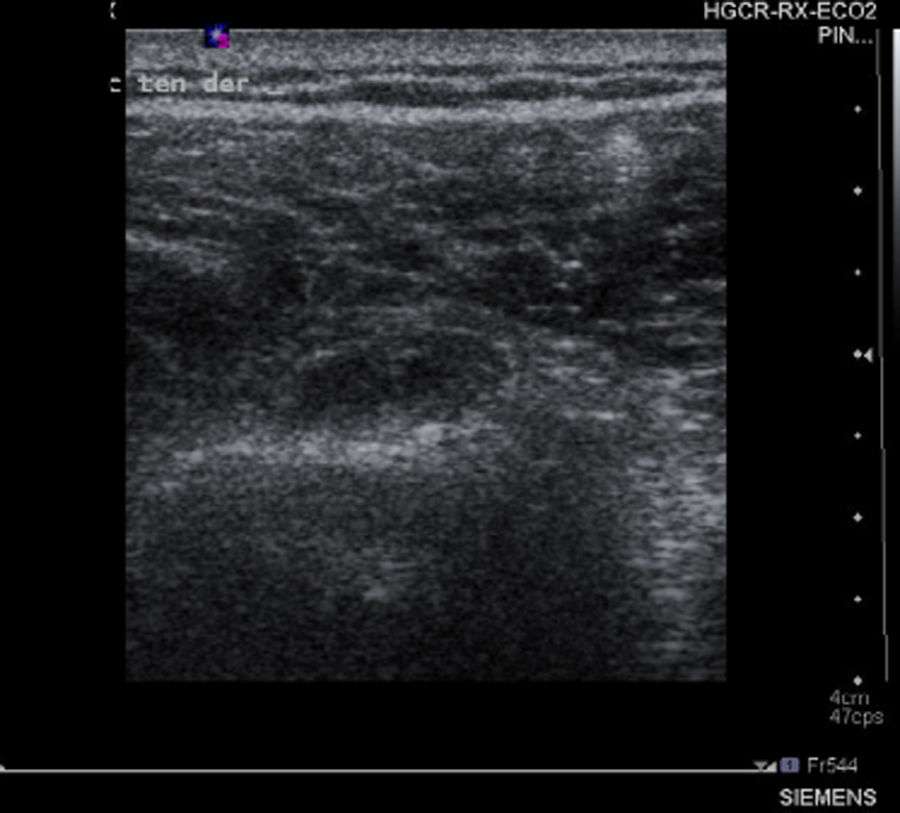
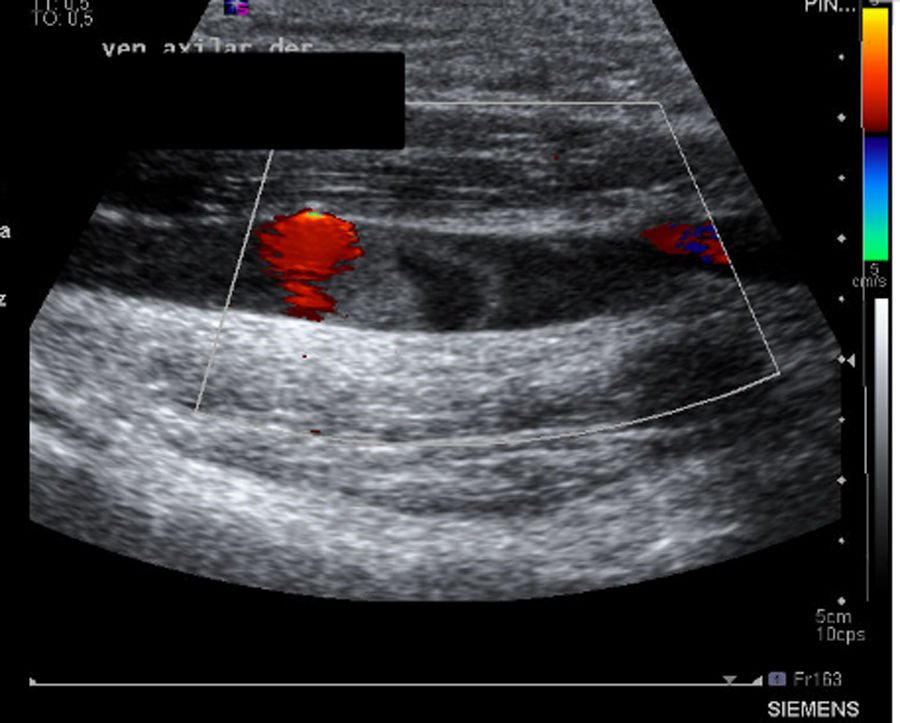
The suspected diagnosis was a probable rotator cuff injury but, due to the striking clinical manifestations, the following complementary tests were carried out: analytical tests, of which we include and highlight D-Dimer assay 309ng/ml, correlated with the Wells score, with high probability of thrombosis (score≥3), fibrinogen 480mg/dl, 100% prothrombin activity 100%, CPK 421<IU/l, CPR 1.6mg/dl; as well as shoulder ultrasound and upper limb venous Doppler ultrasound. The ultrasound findings were described as destructuring of the muscle fibres and increase in volume of the proximal and middle third of the biceps brachii in relation to extensive fibrillar tear with associated haematoma of 6cm and tendon of the long portion of the biceps with thickening and free fluid, compatible with partial tear (Fig. 1). In addition, occupation of the partial axillary vein in a segment of some 40mm compatible with thrombosis (Fig. 2). Permeable internal jugular, subclavian, humeral, basilic and cephalic vein, with no signs of DVT.
On confirmation of UEDVT, an anticoagulation regimen was started that consisted of subcutaneous Fraxiparine Forte® 171IU every 24h for one month, followed by subcutaneous Fraxiparine Forte® 85.5IU every 24h for 2 months and follow-up by the internal medicine department, which ruled out other secondary causes of UEDVT according to clinical symptoms, medical history and follow-up analytical tests (haemogram, basic coagulation study, biochemistry and enzymes). From the trauma perspective, conservative treatment was started with a regimen of rehabilitation, and the patient made satisfactory progress with functional recovery and return to work.
DiscussionInjury to the biceps long tendon is a common condition in our clinical practice, especially associated with activities that involve efforts of the upper extremities.
The prevalence of the disease process of the biceps tendon is described as ranging from 5% to almost 40% and increases with age.6 There are 2 types of lesion, partial and complete.
Some authors have divided the causes by age group, they describe anomalies of the bicipital groove in young people, together with repeated trauma; in older people and the elderly the predominant causative factor is degenerative change to the tendon.7
However, UEDVT is a much less frequent condition. Mortality due to UEDVT can reach 12%.1 When it occurs, it affects males more (2:1), and the dominant arm; it can also be bilateral. We differentiate 2 types of DVT; primary or spontaneous, and secondary.
Primary UEDVT is also known as Paget-Schroetter syndrome or effort thrombosis, we do not know its exact mechanism of production and its incidence ranges from one to 2 cases per 100,000 inhabitants/year.2 It is believed that repeated microtrauma and/or chronic compression would lead to chronic inflammation that would lead to fibrosis, with relative fixation and adherence of neighbouring anatomical structures and perhaps intimal hypertrophy of the vessels.8,9 Loss of connective tissue around the veins has been observed in samples of pathological anatomy, which is replaced by dense scar tissue. This tissue would result in a less mobile costoclavicular space, with the consequent increased risk of thrombosis.10 The pathogenesis would be similar to that produced in thoracic outlet syndrome, where narrowing of the thoracic operculum occurs due to multiple causes (bone and musculoligamentous anomalies, abnormal fibrous tracts, etc.), giving rise to varied clinical neurovascular manifestations.
In most patients, secondary UEDVT is due to known causes, including the use of intravenous catheters, neoplasms, thrombophilia, clavicular fractures, thoracic outlet syndrome, or arthroscopic shoulder processes. These patients are older than those affected by the primary aetiology.1
High clinical suspicion is required for diagnosis, since manifestations such as pain, “heaviness”, oedema, inflammation or cyanosis can go unnoticed or be attributed to other causes. Therefore, we consider it particularly important in these cases to visualise the axillary-subclavian vein by means of Doppler ultrasound, and thus prevent a delay in diagnosis. This has been described in several cases in the literature.1
The natural history of UEDVT is unknown, but it is thought to entail an increased risk factor for future thrombosis, which would suggest invasive treatments. Each time a subclinical syndrome with partial venous obstruction occurs, followed by recanalisation, the local consequence of the inflammation itself and subsequent local fibrosis would progressively increase until total obstruction, with sudden and severe clinical symptoms, such as pulmonary thromboembolism, which can be fatal.8 Treatment includes anticoagulation or recanalisation by means of a stent. Most cases described in the literature have been resolved with medical treatment, which consists of anticoagulation for a minimum of 3 months.
ResultsWe found no cases in the literature of UEDVT as a complication of a musculotendinous injury to the biceps brachii; therefore its diagnosis requires a high level of suspicion. We describe this complication in which both conditions are associated, and therefore we must always consider their possible presence in order to make a prompt diagnosis and thus avoid fatal consequences.
Level of evidenceLevel of evidence v.
We would like to thank Pedro Zorrilla Ribot, Luis Alejandro Gomez Navalón and Juan Antonio Muñoz Berenguer, for their help, patience, understanding, great experience and constant dedication to teaching.
Please cite this article as: Muñoz Sánchez JL, López Salinas JT, Rosas Ojeda ML, Zorrilla Ribot P. Trombosis venosa profunda del miembro superior secundaria a rotura musculotendinosa del bíceps braquial: a propósito de un caso clínico. Rev Esp Cir Ortop Traumatol. 2020;64:74–76.