The aim of this study is to evaluate the usefulness of magnetic resonance imaging (MRI) at 20° of knee flexion in patients with patellofemoral pain syndrome (PFPS) caused by suspected patellofemoral malalignment (PFM).
Materials and methodsFifty MRIs were performed on 25 patients with PFPS secondary to suspected PFM based on clinical examination, and on 25 patients without PFPS (control group). Measurements were made of tibial tuberosity–trochlear groove distance (TTTG) and modified Laurin, Merchant and trochlear angles. The results were analyzed with ANOVA and Fischer's tests. Pearson's correlation coefficients were used to analyze differences between PFPS and control cases. Specificity, sensitivity, positive predictive value and negative predictive value for knee pain were documented.
ResultsSignificant differences were observed between PFPS and control groups in TTTG (11.79mm vs. 9.35mm; P=.002), Laurin angle (12.17° vs. 15.56°; P=.05), and trochlear angle (139° vs. 130.02°; P=.049). No differences were found between groups as regards the merchant angle (P=.5). TTTG was 70% predictive of PFPS; however, it was only 53.33% specific, with a sensitivity of 51.61% for PFPS. Laurin angle was 77.78% predictive of PFPS, with a specificity of 92% and a sensitivity of 28%. Trochlear angle was 85.71% predictive of PFPS, with a specificity of 96% and a sensitivity of 24%.
ConclusionsMRI can confirm clinically suspected PFPS secondary to malalignment. MRI determination of TTTG, patellar tilt, and trochlear angle correlates positively with clinical diagnosis of PFPS, suggesting that PFPS is caused by subtle malalignment.
Evaluar la utilidad de la resonancia magnética (RM) tomada en 20° de flexión de rodilla en el diagnóstico del dolor patelofemoral (DPF) causado por mal alineamiento patelar (MAP).
Material y métodoSe realizaron 25 RM en pacientes con DPF en los cuales se sospechó de MAP como causa y 25 en pacientes sin DPF (grupo control). Se midieron: distancia surco intertroclear-tuberosidad anterior tibial (SIT-TAT) y los ángulos de: Laurin modificado, Merchant y Troclear. Análisis estadístico con los test de ANOVA, Fischer y Pearson.
ResultadosHubo diferencias significativas entre los pacientes con DPF vs. grupo control en relación a: distancia SIT-TAT (11,79mm vs. 9,35mm, p=0,002), ángulo de Laurin modificado (12,17° vs. 15,56°, p=0,05) y ángulo Troclear (139° vs. 130,02°, p=0,049). Respecto al ángulo de Merchant no hubo diferencias significativas. La distancia SIT-TAT tuvo un valor predictivo positivo (VPP) del 70% para DPF, con una sensibilidad del 51,61% y una especificidad del 53,33%. El ángulo de Laurin modificado tuvo un VPP del 77,78% para DPF, con una sensibilidad del 28% y una especificidad del 92%. El ángulo Troclear tuvo un VPP del 85,71% para DPF, con una sensibilidad del 24% y una especificidad del 96%.
ConclusionesLa RM en 20° de flexión puede confirmar el MAP como causa de DPF. La determinación de alteraciones de la distancia SIT-TAT, báscula patelar y ángulo Troclear se correlaciona positivamente con la presencia del DPF, sugiriendo que este es causado por un mal alineamiento leve.
Young patients frequently seek consultation for anterior knee pain. This is related mainly to alterations in the patellofemoral joint, which can affect normal joint mechanics; this in turn causes patellar instability or long-term degenerative changes or patellofemoral osteoarthritis.1–3 The pain is normally related to patellar malalignment (PMA), with a patellar luxation representing the most extreme expression of this disorder.
In the last few years, greater understanding of the disorders responsible for patellofemoral pain (PFP) has led to an improvement in the methods for managing this pain; however, for this treatment to be a success, it is essential to identify the origin of the pain using the physical examination and imaging techniques.4
When the cause of PFP is malalignment, X-rays or computed axial tomography (CAT) scans can be used to detect the site where the anatomy is altered.4,5 However, there are many ways to perform these tests and a wide range of values is described as “normal” in the literature, which makes final interpretation confusing.2,4,6–8 That is why the usefulness of imaging techniques in the diagnosis of PFP has often been debated.
Magnetic resonance imaging (MRI) can facilitate diagnosis in patients with equivocal clinical symptoms, given that it is capable of visualizing chondral defects that can cause pain, as well as probable PMA in these cases. Detecting lesions of the cartilage of the patellofemoral compartment can be useful in preoperative planning for procedures designed to lower the pressure of patellofemoral contact in the injured places or to treat chondral lesions.
Various studies report the use of MRI as a diagnostic tool for PMA in patients with anterior knee pain, indicating that they are comparable in diagnostic value to other classic examinations.6,9–11
The objective of this study was to assess the usefulness of the MRI at 20° knee flexion in patients with PFP caused by probable PMA.
Our hypothesis was that the findings of PMA in MRIs would have a positive value with PFP and that it would likewise be possible to detect, at the same time, chondral lesions that also act as a source of PFP.
Materials and methodsThere were 25 MRIs taken at 20° knee flexion of 25 patients with PFP with suspicion of PMA as the cause of pain (patients who visited the doctor due to anterior knee pain that increased in loaded flexion more than 20°, with episodes of patellar subluxation, without clear luxation episodes). There were also 25 MRIs at 20° knee flexion taken of 25 patients without PFP, who represented the control group. The MRIs were performed at 20° knee flexion because, at this instant of flexion, the patella fits into the trochlea. Data were taken measuring in the axial cut-off corresponding to the deepest area of the femoral trochlea.
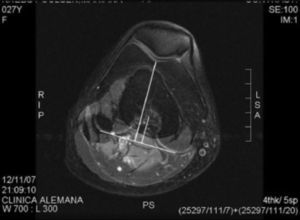
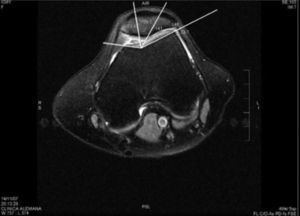
The parameters measured were the tibial tubercle–trochlear groove (TT–TG)12 distance (to assess the lateral displacement of the extensor mechanism [Fig. 1]), the modified angle of Laurin13 (using a line drawn on the posterior aspect of the femoral condyles as a reference to assess patellar tilt [Fig. 2]), the Merchant congruence angle14 (used to assess patellar subluxation [Fig. 3]), and the trochlear angle13 (to assess possible trochlear dysplasia [Fig. 3]). All parameters were measured at 20° knee flexion using MRI bone images.
Patellar anterior knee pain was defined as the presence of a heterogeneous signal or defects in patellar cartilage in the MRI.
In addition, we documented chondral, meniscal and ligament lesions in the entire knee.
A General Electric® 1.5Tesla scanner (GE Medical Systems, Milwaukee, WI, USA) was used.
In the group of patients with PFP, 6 (24%) were men and 19 (76%) were women. Mean age was 37.1 years (range: 15–54). In the control group, 3 (12%) patients were men and 22 (88%) women, with a mean age of 38.85 years (range: 16–56). In this group, MRI examination was requested due to clinical suspicion of meniscus syndrome, without other accompanying clinical findings.
Statistical analysisWe analyzed TT–TG distance and the angles of modified Laurin, Merchant congruence, and trochlear in the patients with and without PFP using ANOVA and Fischer tests. We measured the Pearson correlation coefficients to analyze the difference between the 2 groups.
In addition, we documented the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
This study was carried out according to ethical standards and had been approved by our institution.
ResultsTable 1 presents the results obtained after assessing the parameters of a PMA in the MRI of the patients with and without PFP, comparing our results with those described in the literature for a PMA assessed using CAT scan.15–17 We found a significant difference in our results between the patients with PFP and the control group in TT–TG distance, modified angle of Laurin, and trochlear angle. No significant differences were found in the Merchant congruence angle between the patients with PFP and the control group.
Mean values of the measurements assessed with MRI in the PFP patients and in the control group, and mean CAT values according to the literature.
| MRI/PFP group | MRI/control group | P value | CAT scan (according to the literature) | |||
| Mean | SD | Mean | SD | Mean | ||
| TT–TG | 11.79 | ±3.2 | 9.35 | ±2.7 | 0.002 | ≥10.2±3.1 |
| Laurin | 12.17 | ±5.7 | 15.56 | ±3.4 | 0.05 | >10±4 |
| Merchant | −5.5 | ±2.4 | −15.19 | N/A | 0.5 | −8+16 |
| Trochlear | 139 | ±7.2 | 130.02 | ±5.1 | 0.049 | 138±6 |
In the analysis of TT–TG distance, when 10mm was chosen as the cut-off value, we found that a TT–TG distance ≥10mm had sensitivity of 51.61%, specificity of 53.33%, PPV of 69.57%, and NPV of 34.78% for the presence of anterior knee pain. The patients with PFP showed significantly greater lateral deviation of the anterior tubercle of the tibia than the patients in the control group did.
With respect to the Merchant congruence angle, when we chose −8° to +16° as the critical range, an angle ≥16° had sensitivity of 60%, specificity of 36%, PPV of 48.39%, and NPV of 47.37% for the presence of anterior knee pain.
In spite of the fact that the patients with PFP had larger values in the Merchant congruence angle, this difference was not significant.
In the analysis of the modified Laurin angle, when we chose <8° as the cut-off value, an angle of <8° had sensitivity of 28%, specificity of 92%, PPV of 77.78%, and NPV of 56.1% for the presence of anterior knee pain.
Patients with PFP had significantly lower values in this angle. Consequently, they had greater lateral patellar tilt than the patients in the control group.
Insofar as the trochlear angle, when we chose 144° as the cut-off value, an angle >144° had sensitivity of 24%, specificity of 96%, PPV of 85.71%, and NPV of 55.81% for the presence of anterior knee pain.
Patients with PFP had significantly larger trochlear angles than the patients in the control group. Consequently, they had a greater tendency to develop trochlear dysplasia.
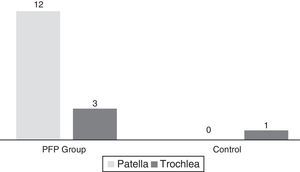
Fig. 4 indicates the frequency of patellofemoral chondral lesions found in the groups with PFP and in the control group. Within these, we observed chondromalacia patella only in subjects in the group with PFP (12). These lesions showed a PPV of 93.7% for the presence of anterior knee pain, with sensitivity of 60% and specificity of 96%.
DiscussionThe literature includes references to the fact that the MRI in patients with anterior knee pain can show an abnormal patellar tilt or even patellar subluxation.9,10,15–18
In this study, the mean TT–TG distance in patients with PFP was 11.79±3.2mm. This results strongly correlated with the results presented by Jones et al.15 (12.2mm in studies using CAT scans at 20° knee flexion) and Wittstein et al.19 (12.6mm with MRI at complete knee extension).
However, as we mentioned earlier, there are differences between the measurements considered as “normal” by different studies. This may be due to the fact that the external rotation of the tibia in complete knee extension increases the lateralization of the tibial tubercle. That is why the study was performed at 20° knee flexion, because at this degree of flexion, the patella fits into the trochlear grove and the angles measured are more predictive of PFP.
Values for the TT–TG distance >10mm can be used to identify patients with slight PMA with high specificity and sensitivity. This is true for both the CAT scan (95% and 85% respectively)15 and the MRI (70% and 64% respectively).19
In this study, when we chose 10mm as the critical value, TT–TG distance was predictive of PFP in 70% of the cases. However, this cut-off value was only 53.3% specific and 51.61% sensitive for the presence of anterior knee pain.
A modified angle of Laurin <8° has high specificity and sensitivity for anterior knee pain in complete extension CAT scans (90% and 96% respectively)20 and MRI examinations (70% and 93% respectively).19
Our results show that this angle measured in MRI at 20° flexion, when taking <8° as the cut-off value, was predictive for the presence of PFP in 77.78% of the cases, with specificity of 92% and sensitivity of 28%.
We documented that a trochlear angle greater than 144° was predictive of PFP in 87.51% of cases, with specificity of 96% and sensitivity of 24%. As far as we know, this is the first study to demonstrate a correlation between this angle and PFP.
It is likewise important to emphasize the great number of chondral lesions in the group of patients with PFP compared with the control group. The detection of these lesions may be the main advantage of MRI vs. CAT scan in patients with anterior knee pain. Using MRI can even, in some cases, modify treatment as well.
The weaknesses of our study were that the subjects in the control group did not have completely normal knees and that there was a lack of comparison with CAT scan (which is the gold standard imaging test in the diagnosis of PMA). Consequently, this study should be continued with a larger number of cases and correlating our results with CAT scan, which might help to validate our measurements.
In conclusion, we can say that the use of MRI at 20° flexion can confirm the diagnosis of PMA in patients with PFP.
The determinations based on the MRIs of the lateralization of the tibial tubercle using TT–TG distance, alterations in patellar tilt (modified angle of Laurin), and trochlear angle are positively correlated with the clinical diagnosis of anterior knee pain. This suggests that the pain is caused by mild PMA. However, it is important to point out that it is necessary to fine tune the cut-off points for the measurements established. This is because the sensitivities, specificities, and predictive values obtained were not ideal in all of the cases.
A significant advantage of the MRI over the CAT scan in this type of patients is that the former makes it possible to assess accompanying lesions, especially chondral lesions in the patellofemoral compartment.
Level of evidenceLevel of evidence 4.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments on human beings or animals were performed for this research.
Data confidentialityThe authors declare that they followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their informed consent in writing to participate in this study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects mentioned in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Figueroa D, Novoa F, Meleán P, Calvo R, Vaisman A, Figueroa F, et al. Utilidad de la resonancia magnética en la evaluación del mal alineamiento patelar. Rev Esp Cir Ortop Traumatol. 2014;58:19–23.