Evaluate the enlargement effect of the tibial tunnel emergence of 2 different of anterior cruciate ligament reconstruction techniques: antero-medial portal (AMP) vs. transtibial (TT) technique.
MethodsA prospective, randomised controlled study was performed in 36 consecutive patients who underwent anterior cruciate ligament reconstruction with autologous hamstring tendon grafts employing the AMP and conventional TT techniques. Lateral and antero-posterior radiographs were obtained for each patient at 6 weeks and 12 months postoperatively. The sclerotic margins of the tibial tunnels were measured at the widest dimension of the tunnel as well as the diameter of the tibial emergence and were compared with the initially drilled tunnel size after correction for radiographic magnification. Statistical analysis was performed to compare the 2 groups by use of the independent-samples t test, with significance set at .05.
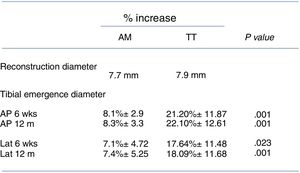
ResultsThe mean percentage increase in the diameter of tibial tunnel emergence at 6 weeks after surgery was 8.1%±2.9 for the PAM technique and 21.20%±11.87 for the TT technique on the anteroposterior X-ray view. However, the mean percentage increase in the diameter of the tibial tunnel emergence on the lateral view was 7.1%±4.72 for the medial portal technique and 17.64%±11.48 for the transtibial technique. This difference was statistically significant on both anteroposterior and lateral views.
ConclusionsThe diameter of the tibial tunnel emergence for hamstring autologous anterior cruciate ligament reconstructions was significantly lower for the medial portal technique when compared with the conventional TT technique.
Evaluar el diámetro de la emergencia del túnel tibial con relación a la técnica de reconstrucción del ligamento cruzado anterior, empleando isquiotibiales autógenos, y comparar las técnicas a través del portal anteromedial (PAM) y la convencional transtibial (TT).
MétodosEstudio prospectivo, aleatorizado y comparativo de 36 pacientes diagnosticados con insuficiencia del ligamento cruzado anterior, intervenidos en forma sucesiva mediante reconstrucción primaria, con las técnicas de reconstrucción a través de PAM (16 pacientes) y la TT convencional (20 pacientes) con isquiotibiales autógenos. Todos los pacientes fueron evaluados radiológicamente, con valoración del diámetro de emergencia tibial en los planos anteroposterior y lateral a las 6 semanas y a los 12 meses del procedimiento quirúrgico respecto al tamaño de la plastia utilizada en la cirugía. Se realizó un análisis estadístico comparando ambos grupos mediante la t de Student con un valour de significación de 0,05.
ResultadosEl diámetro de la emergencia tibial con relación al tamaño de la plastia utilizada, obtenido a las 6 semanas en la proyección anteroposterior, manifestó un incremento del 8,1%±2,9 con la técnica PAM y del 21,20%±11,87 con la técnica TT, mientras que en la proyección lateral fue de 71%±4,72 y del 17,64%±11,48, respectivamente. Las diferencias fueron estadísticamente significativas tanto en el plano anteroposterior como en el lateral.
ConclusionesEl diámetro de la apertura tibial mostró ser significativamente mayor con la técnica TT a las 6 semanas y a los 12 meses de seguimiento radiológico tanto en la proyección anteroposterior como en la lateral.
Many studies have supported the efficacy of anterior cruciate ligament (ACL) reconstruction in re-establishing normal knee movement and joint function.1–3
Nevertheless, single-bundle transtibial reconstruction does not seem to completely re-establish joint stability, as although it would give rise to sagittal (antero-posterior) plane stability, it would not make it possible to achieve rotational stability.4,5
With the aim of reproducing the anatomy and re-establishing knee rotational component stability, anatomical reconstruction techniques have emerged using an independent portal such as the antero-medial portal (AMP). In spite of the numerous studies that prove the advantages of reconstruction using an independent portal,6,7 some publications evaluate the clinical results of AMP and conventional transtibial (TT) techniques, showing that there is no significant difference between them.8,9
There is still controversy regarding reconstruction technique and fixing method. When soft tissue grafts are used, attachment close to the joint interline seems to give rise to greater rigidity and a reduction in the frequency of tunnel widening.10–12
The causes of bone tunnel widening following ACL reconstruction are multifactorial, and mechanical and biological factors are the most common. Tunnel widening occurs in the immediate postoperative period, followed by a gradual increase over weeks and months.13,14 In spite of this, there is no correlation between the degree of tibial tunnel widening and clinical results after ACL reconstruction.15–18
However, tunnel widening leads to more demanding revision surgery, so that in the most severe cases of widening reconstruction has to take place in 2 stages.
The aim of this work is to evaluate the increase in the diameter of the tibial tunnel emergence after reconstruction of the ACL with hamstrings using AMP and conventional TT techniques, in terms of the diameter of the tunnel created by the surgical procedure in the immediate postoperative period after 6 weeks and 12 months of follow-up.
Material and methodsThis prospective, randomised and comparative study is based on 36 patients diagnosed with ACL failure. They were treated consecutively using primary reconstruction of the ACL with autogenous hamstrings. The patients were operated in the period from July 2012 to July 2013. All of the surgical procedures were performed by the same surgeon (JS). The following data were recorded: the injury mechanism and data from the surgical procedure: the diameter of the graft used, the drilling diameter of the tibial tunnel, the type of femoral attachment and the tibial interference screw used.
Study designThe patients who were operated for primary ACL reconstruction with autogenous hamstrings took part in this study with a follow-up of at least 2 years.
The inclusion criteria were that only patients with ACL injury operated using autogenous hamstring graft surgery were included. The exclusion criteria were: (1) Patients with radiological signs of arthrosis at the time of ACL reconstruction. (2) Patients with a history of ACL reconstruction. (3) Associated ligament injuries (TCL, CML or PCL) at the time of reconstruction, and (4) the presence of genu recurvatum (as this is considered to be a hyperlaxitude criterion).
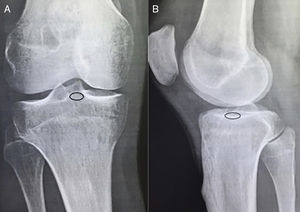
The patients were distributed at random and divided into 2 groups, according to the surgical technique used. The first group was composed of 16 patients who had been subjected to anatomical reconstruction of the ACL using AMP technique and femoral cortical attachment. Those in the second group, which was composed of 20 patients, were operated using conventional TT technique with transversal femoral attachment.
The same rehabilitation protocol was used in both groups. A graduated knee bandage was used during the 6 weeks after the surgical procedure in all of the patients. From the seventh day after surgery onwards the emphasis was on achieving complete extension and isometric quadriceps exercises. Flexion was gradual until 90° was completed at 4 weeks. After this time there was a gradual increase until the knee bandage was removed. Crutch-assisted standing was commenced gradually after the second week, while independent walking commenced after the 6th week. After the 8th week the patients commenced exercises for propioception, quadriceps muscle tone and walking. Recreational sports activities commenced after the 4th month, while competitive sports activity was authorised after the 8th month.
Radiological evaluationAll of the patients were evaluated using an antero-posterior (AP) X-ray taken at maximum extension, where the kneecap was located in the centre of the distal end of the femur and the head of the fibula was partially hidden by the proximal end of the tibia,19 together with another lateral (Lat) X-ray with the knee flexed at approximately 30°, showing the superimposition of the femoral condyles.
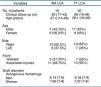
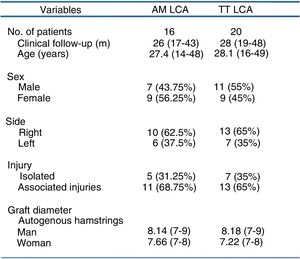
The sclerotic lines of the tibial tunnel were marked in both projections, as was the diameter of the tibial emergence. Both marks were made by a radiological doctor (ARO) and a knee surgeon (JS). Digital radiology was used to evaluate the diameter of the tibial tunnel emergence (Fig. 1).
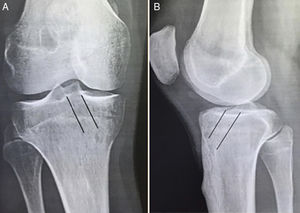
Radiological examinations took place at 6 weeks and 12 months after surgery to evaluate the diameter of the tibial tunnel emergence. Digital radiology was used to evaluate the diameter of the tibial tunnel emergence. The average percentage of widening of the tibial tunnel emergence is given by the ratio of the tibial emergence diameter at 6 weeks and one year after the surgical procedure and the diameter of the reconstructed part (Fig. 2).
Graft usedAutogenous hamstrings were used in all of the reconstructions, configured in 4 bundles with independent ends.
The diameter of the autogenous grafts was similar in both groups (P .005). In group I (AMP), the average diameter of the graft was 8.14mm (range 7–9) in the men and 7.66mm (range 7–8) in the women, while in group II (TT) it was 8.18mm (range 7–9) in the men and 7.22mm (range 7–8) in the women.
Statistical methodThe tibial emergence in the antero-posterior and lateral planes in both groups was compared by independent tests using Student's t-test with the parameter of .05. Inter-observer variability was determined by using the correlation coefficient scale between measurements.
ResultsThe study sample was composed of 18 male patients and 18 female patients. The average age was 26.4 years old (ranging from 14 to 49 years old). The average time lapse between the injury and surgery was 3.9 months (range 2–14 months). The right knee was involved in 23/36 cases (64%), while associated lesions to the meniscus and cartilage were present in 24/36 cases (67%). The demographic distribution is shown in Fig. 3.
There was no significant difference in average age or sex distribution between both surgical techniques (P .51 and P .530, respectively).
In all cases the sclerotic edges of the tunnel and its tibial emergence (Fig. 4) were present and clearly defined in the antero-posterior and lateral X-rays. The emergence diameter was significantly smaller in the AMP reconstruction technique, with an increasing in the tibial emergence in AP projections at 6 weeks of 8.1% and 8.3% at 12 months, while in lateral projection at 6 weeks it was 7.1% and at 12 months it was 7.4%. With the TT technique in AP projection at 6 weeks it was 21.20% and at 12 months it was 22.10%, while in lateral projection it was 17.54% at 6 weeks and 18.09% at 12 months (P .001 and P .001, respectively).
The inter-observer variability when evaluating the emergence of the tibial tunnel was excellent, with a coefficient of 0.77 and 0.80 for the antero-posterior and lateral projections, respectively.
DiscussionOur results show that the increase in the diameter of the tibial emergence is significantly smaller with the anatomical technique through the AMP. This is so in the period immediately after surgery as well as at one year afterwards in both planes, antero-posterior and lateral.
New modifications in reconstruction of the ACL using the TT technique have been described. They have the aim of re-establishing a better positioning of the tibial tunnel and reproducing the anatomical track of the femoral insertion of the ACL. Howell et al.20 showed the importance of horizontality in the coronal plane of the tibial tunnel to achieve suitable obliquity of the graft. On the other hand, Chhabra et al.21 analysed the starting point of the tibial tunnel to obtain the necessary obliquity of the tunnel. Respecting the femoral track when using the TT technique, in 2014 Lee et al.22 modified this technique by a manoeuvre that combines anterior translation, adduction and external rotation of the tibia. This has the aim of obtaining a positioning that is lower and posterior in the medial wall of the lateral condyle.
During the TT technique and with the aim of reproducing a more anatomical orientation of the femoral tunnel, eccentric tibial drilling takes place that creates a larger tibial emergence than the initial tibial emergence. This technical detail could explain the significant difference found in the increase in the diameter of the tibial tunnel when TT technique is used (21.20% and 17.64% in the antero-posterior and lateral projections, respectively) in comparison with the AMP technique (8.1% and 7.1% in the antero-posterior and lateral projections, respectively) in the X-ray check-up at 6 weeks in this study. We believe that this finding had been present from immediately after the operation, and that it is connected with the technical details intrinsic to the TT technique and not with early-onset instability. Bedi et al.23 reported a 38% increase in the antero-posterior diameter of the tibial tunnel with the TT technique in comparison with the AMP technique. This is similar to the increase found in our study.
In the radiographic imaging tests at one year of follow-up we found a gradual increase in the diameter of the tibial emergence in both techniques. It was significantly larger in the lateral projection in cases of TT technique than it was in those where the AMP technique had been used. Ayala-Mejias et al.14 showed progression in the growth of the tibial tunnel in their series with a follow-up of at least 18 years, and they found a direct relationship between verticality and the progressive expansion of the tibial tunnel. The author postulates that a tibial tunnel close to a position of 90° in the coronal plane generates greater stress on the reconstruction and gradual widening of the tibial tunnel. As was the case for this author, we found that with the TT technique the orientation of the tibial tunnel was more vertical in the coronal plane. This may explain the significant increase in the diameter of the tibial tunnel emergence.
On the other hand, and in spite of the numerous biomechanical studies that have described the anatomical track of the formal insertion of the ACL, controversy still exists regarding the ideal position of the femoral tunnel and the impossibility of creating an independent femoral tunnel using the TT technique. A vertical positioning of the femoral tunnel does not re-establish rotational stability.24,25 Dargel et al.26 reported a more anterior and vertical positioning of the femoral tunnel when it was perforated from the tibial tunnel. Nevertheless, Miller et al.27 reported a more posterior positioning of the emergence of the femoral tunnel with the AMP technique, while other studies6,23 have shown a suitable positioning in the centre of the native femoral track of the ACL using the AMP technique.
In spite of this ongoing debate, no significant relationship has been proven to exist between the gradual widening of the tibial tunnel and progressive instability after 5 years’ evolution.28 However, gradual changes in osteoarthrosis have been associated with progressive increases in the diameter of the tibial as well as the femoral tunnel,14 so that it is necessary to attempt to understand and achieve the ideal positioning of the tibial and femoral tunnels to give better long-term results.
This study has a series of limitations. (1) The expansion of the tibial and femoral tunnels was not evaluated, as the aim of this study was to evaluate the diameter of the emergence of the tibial tunnel. (2) No three-dimensional radiological study was performed of the location of the tunnels in the bone used in ACL reconstruction. However, the study in the antero-posterior and lateral planes is sufficiently useful to allow surgeons to carry out intra- and postoperative studies of ACL reconstructions. (3) Another weak point is the method used to measure the tunnels and the tibial emergence, due to the subjective factor when setting the parameters for digital measurement. Notwithstanding this the inter-observer variability was found to be excellent after determining the correlation coefficient between measurements. (4) Lastly, and even though this study was solely radiological, the patients were not evaluated using objective clinical evaluation scales before or after surgery.
ConclusionsThe diameter of the tibial emergence was found to be significantly larger with the TT technique at 6 weeks and 12 months of radiological follow-up in the antero-posterior as well as lateral projections.
Level of evidenceLevel of evidence I, a prospective, randomised and comparative study.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments with human beings or animals have been performed while conducting this investigation.
Confidentiality of dataThe authors confirm that in this article there are no data from patients.
Right to privacy and informed consentThe authors confirm that in this article there are no data from patients.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Silberberg Muiño J, Nilo Fulvi A, Vera G, Gutiérrez García JL, Giménez Salvay M, Maroa Salvucci M, et al. Valoración de la apertura del túnel tibial tras la reconstrucción del ligamento cruzado anterior empleando isquiotibiales autógenos: Estudio comparativo entre la técnica de portal anteromedial y la técnica transtibial convencional. Rev Esp Cir Ortop Traumatol. 2018;62:190–196.