While options for operative treatment of leg axis varus malalignment in patients with medial gonarthrosis include several established procedures, such as unicompartmental knee arthroplasty (UKA), total knee arthroplasty (TKA), or high tibial osteotomy (HTO), so far there has been little focus on a less invasive option introduced more recently: the UniSpacer™ implant, a modern, self-centring, metallic interpositional device for the knee. This study not only evaluates whether alignment correction can be achieved by UniSpacer™ arthroplasty but also evaluates alignment change in the first 5 postoperative years. Antero-posterior long leg stance radiographs of 15 legs were digitally analysed to assess alignment change: two relevant angles and the deviation of the mechanical axis of the leg were analysed before and after surgery. Additionally, the change of the postoperative alignment was determined one and five years postoperatively. Analysing the mechanical tibiofemoral angle, a significant leg axis correction was achieved, with a mean valgus change of 4.7±1.9°; a varus change occurred in the first postoperative year, while there was no significant further change of alignment seen five years after surgery. The UniSpacer™ corrects malalignment in patients with medial gonarthrosis; however, a likely postoperative change in alignment due to implant adaptation to the joint must be considered before implantation.
Aunque entre las opciones del tratamiento operatorio de la desalineación en varo del eje de la pierna en pacientes con gonartrosis medial se incluyan varios procedimientos consolidados como, por ejemplo, la artroplastia unicompartimental de rodilla (AUR), la artroplastia total de rodilla (ATR) o la osteotomía tibial valguizante (OTV), hasta ahora no se ha prestado demasiada atención a una opción menos invasiva de reciente introducción: el implante UniSpacer™, un dispositivo interposicional, autocentrador y metálico para la rodilla. En el presente estudio (14 pacientes, 15 rodillas) nos dedicamos a evaluar si es posible corregir la alineación realizando una artroplastia con el UniSpacer™, así como el cambio de alineación que se produce en los 5 años posteriores a la intervención quirúrgica. Se han analizado digitalmente las radiografías anteroposteriores en carga de 15 rodillas para calcular el cambio de alineación: se analizaron 2 ángulos relevantes y la desviación del eje mecánico de la pierna antes y después de la intervención quirúrgica. Además, se determinó el cambio de la alineación posoperatoria transcurridos entre uno y 5 años. Al analizar el ángulo tibiofemoral mecánico, observamos que se logró una corrección significativa del eje de la pierna, con una media de cambio en valgo de 4,7±1,9°. Durante el primer año posterior a la intervención quirúrgica se produjo un cambio en varo, aunque no se detectó ningún cambio adicional significativo de alineación durante los 5 años posteriores a la intervención quirúrgica. El UniSpacer™ corrige eficientemente la desalineación de algunos pacientes con gonartrosis medial. No obstante, antes de proceder a la implantación deberá tenerse en cuenta la posibilidad de que se produzcan cambios posoperatorios adicionales no inmediatos de la alineación como consecuencia de la adaptación del implante.
Osteoarthritis of the medial compartment of the knee is often associated with varus malalignment.1,2 The most frequently used options for the surgical treatment of knee osteoarthritis affecting only the medial compartment are high tibial osteotomy (HTO) and unicompartmental knee arthroplasty (UKA), especially in younger patients. Both procedures require resection of bone material and, in the case of UKA, it is also necessary to operate on the joint.3
A new and less invasive alternative to these established procedures has arisen in recent years: the UniSpacer™ implant (Zimmer, Inc., Warsaw, IN, USA), which essentially consists in a modern version of a metallic hemiarthroplasty, as described by McKeever4 or MacIntosh.5 Implementing this single-component, self-centring, interpositional device within the knee joint does not require any bone resection and can be performed through a minimally invasive intervention. In addition, it is available in various widths and is adapted to knee kinematics.6 Compared to the iForma™ knee implant introduced recently by ConforMIS,7 the UniSpacer™ is a self-centring device which is not fixed to any structure. This device is used to correct or minimise varus malalignment in cases of unicompartmental knee osteoarthritis, when no other methods are indicated (Fig. 1). The upper surface of the implant is adapted to the femoral condyle after the surgical intervention.8
The concept of a self-centring, movable component which corrects varus knees internally without the need to resect bone material has been, and still is, an interesting option.9
The aim of this study was to assess whether the implantation of a UniSpacer™ device could achieve a correct change of alignment, and whether such a change was correlated with the width of the implant used. In addition, the change in alignment in the 5 years after surgery was also examined.
Our hypothesis was that a significant correction of the leg axis can be expected after implantation of the UniSpacer™ device, and that this implant efficiently corrects malalignment in patients with medial knee osteoarthritis.
Materials and methodsThis retrospective case series (level IV) assessed 14 patients (15 knees) with symptoms of isolated medial knee osteoarthritis, who had undergone a hemiarthroplasty with a UniSpacer™ implant between 2002 and 2004 (implant width: 2, 3 or 4mm). One patient underwent a bilateral implant. In total, 8 right knees and 7 left knees were treated. The mean age of patients (9 males and 5 females) at the time of surgery was 60.8 years (range: 48–72 years).
Inclusion criteria were patients with medial compartment degeneration, with minimal degeneration of the patellofemoral compartment according to grades 2 and 3 in the Kellgren and Lawrence scale. Absolute contraindications for implantation were inflammatory arthritis, instability due to lack of integrity of the medial collateral ligament and knee flexion over 15°.
Radiographs were obtained in an anteroposterior standing position, before surgery and at 3 weeks, 1 and 5 years thereafter, using a standardised technique.10 These images were digitally analysed to assess the change in alignment. Furthermore, a standard protocol was followed to ensure inclusion of the coxofemoral, knee and metatarsal joints while patients were in a vertical position and the patellas were frontally aligned.
The digitised radiographs were evaluated using Medicaid® (Hectec GmbH, Niederviehbach, Germany), a surgical planning software which can also be used for biometric purposes. We measured the mechanical tibiofemoral angle (mTFA) (the angle between the mechanical axes of the femur and tibia) and also the anatomical tibiofemoral angle (aTFA) (the angle between the anatomical axes of the 2 bones). In addition, we determined the location of the mechanical axis of the leg, or load bearing axis, with respect to the centre of the tibial plateau, as established by Kennedy and White11: zones 1 and 2 were in the medial side, zones 3 and 4 were on the side of the tibial prominence, and zone C was the centre of the tibial plateau.
By convention, varus angles were established as negative and valgus angles as positive.1 In order to evaluate the change in alignment achieved through surgical intervention, we determined the difference between the values of each angle before and after surgery by subtraction. We used the corresponding postoperative values to evaluate the change detected in the first year after surgery and 4 years thereafter.
For the purposes of descriptive statistics, we determined the mean value, standard deviation and median of the measured angles and their differences.
We used the Wilcoxon sign test to evaluate the significance of the change in alignment.
The correlation between the correction of alignment and the corresponding implant width was calculated using the Pearson product-moment correlation, while the relevance of the calculated correlation was determined using the Wilcoxon sign test.
ResultsThe leg axis was corrected from a mean preoperative value of −5.1°±3.0° to −0.4°±2.3° after surgery (mTFA). This amounts to a mean correction of 4.7°±1.9° (P=.001).
One year after surgery, the mean mTFA value was −1.5°±1.7°. The mean change in aTFA during the first postoperative year was −1.1°±1.5° (varus) (P=.023).
Five years after surgery, the mean mTFA value was −0.7°±1.6° (mTFA). The mean aTFA change was 0.9°±1.1° (P=.019). In this case we could only evaluate 11 legs because 4 patients had undergone a review total knee arthroplasty (TKA) or UKA as a result of continuous pain. Thus far, there have been no reports of joint displacement.
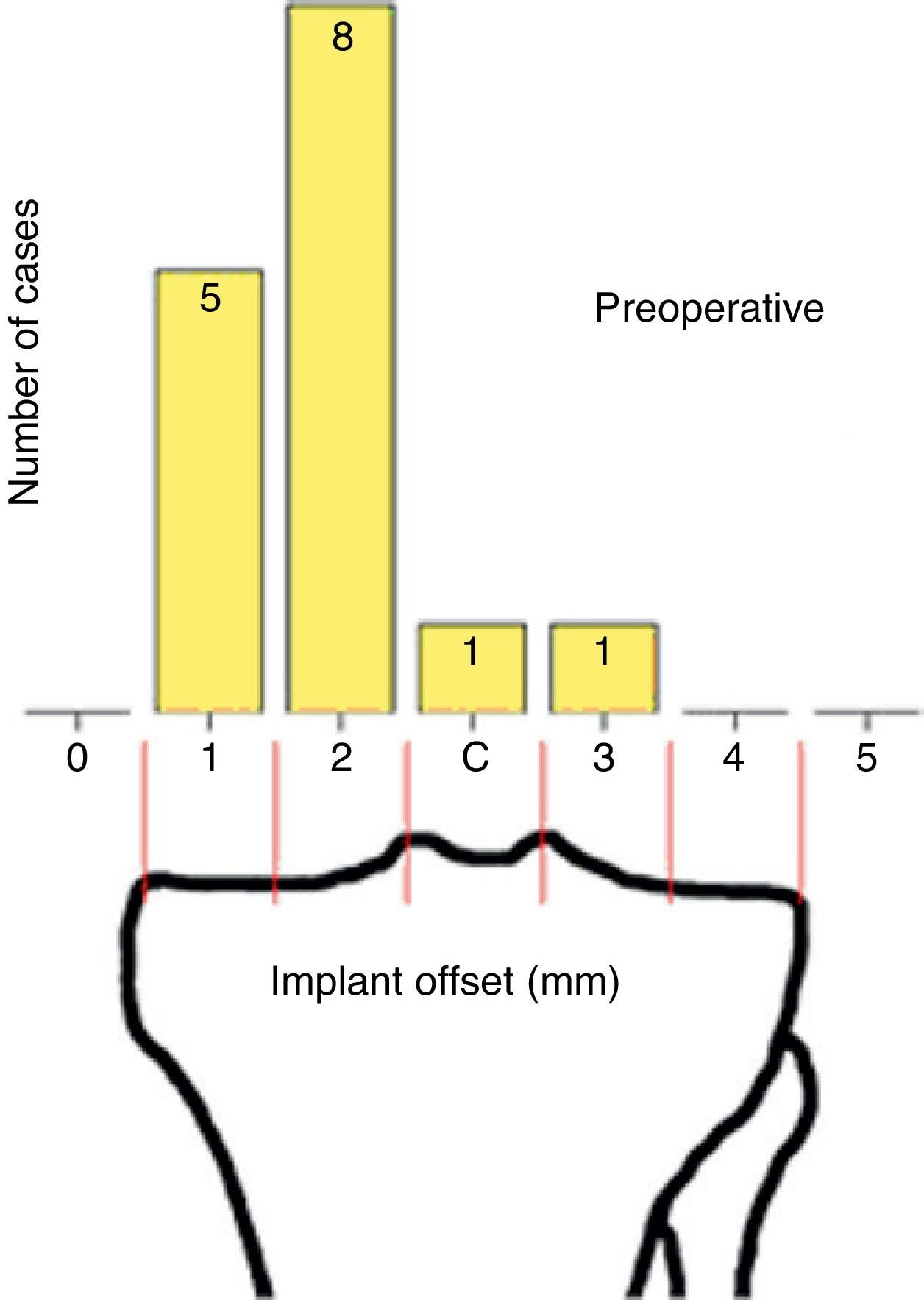
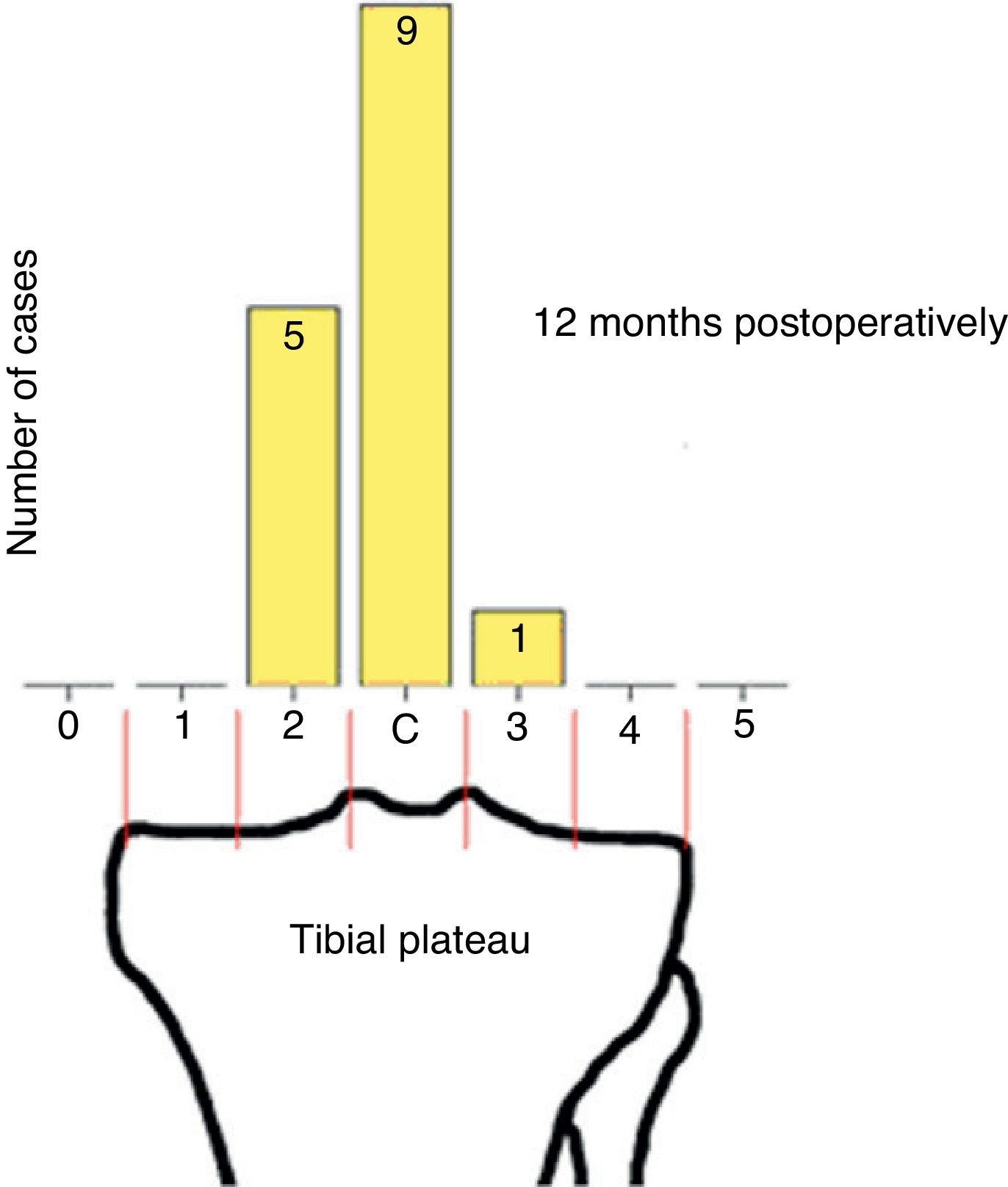
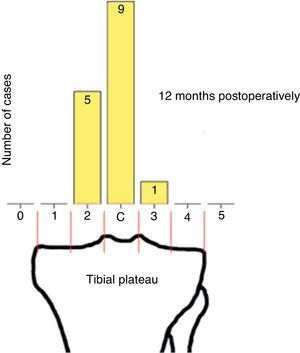
As for the location of the mechanical axis of the leg relative to the tibial plateau, prior to surgery, zone 1 was represented in 5 cases, zone 2 in 8 cases, and zones C and 3 were represented in 1 case each (Fig. 2). After surgery, zone 2 was represented in 4 cases, zone C in 9 cases and zone 3 in 2 cases (Fig. 3). This implies that the location of the load-bearing axis (in areas of the tibial plateau) was not affected by surgery in 3 cases, while in the remaining 9 cases there was a lateral change of 1 zone and in 3 cases there was a lateral change of 2 zones. One year after surgery, we did not detect any additional changes in 9 legs, in 4 cases we detected a medial change of 1 zone and in 2 cases we detected a lateral change of 1 zone (zone 2: 5 cases; zone C: 9 cases; zone 3: 1 case; Fig. 3). Five years after surgery, the axis had returned to zone C in 2 of the 4 prior cases, thus there were only 3 legs with a load-bearing axis located in zone 2, while the majority (8 legs) were in zone C.
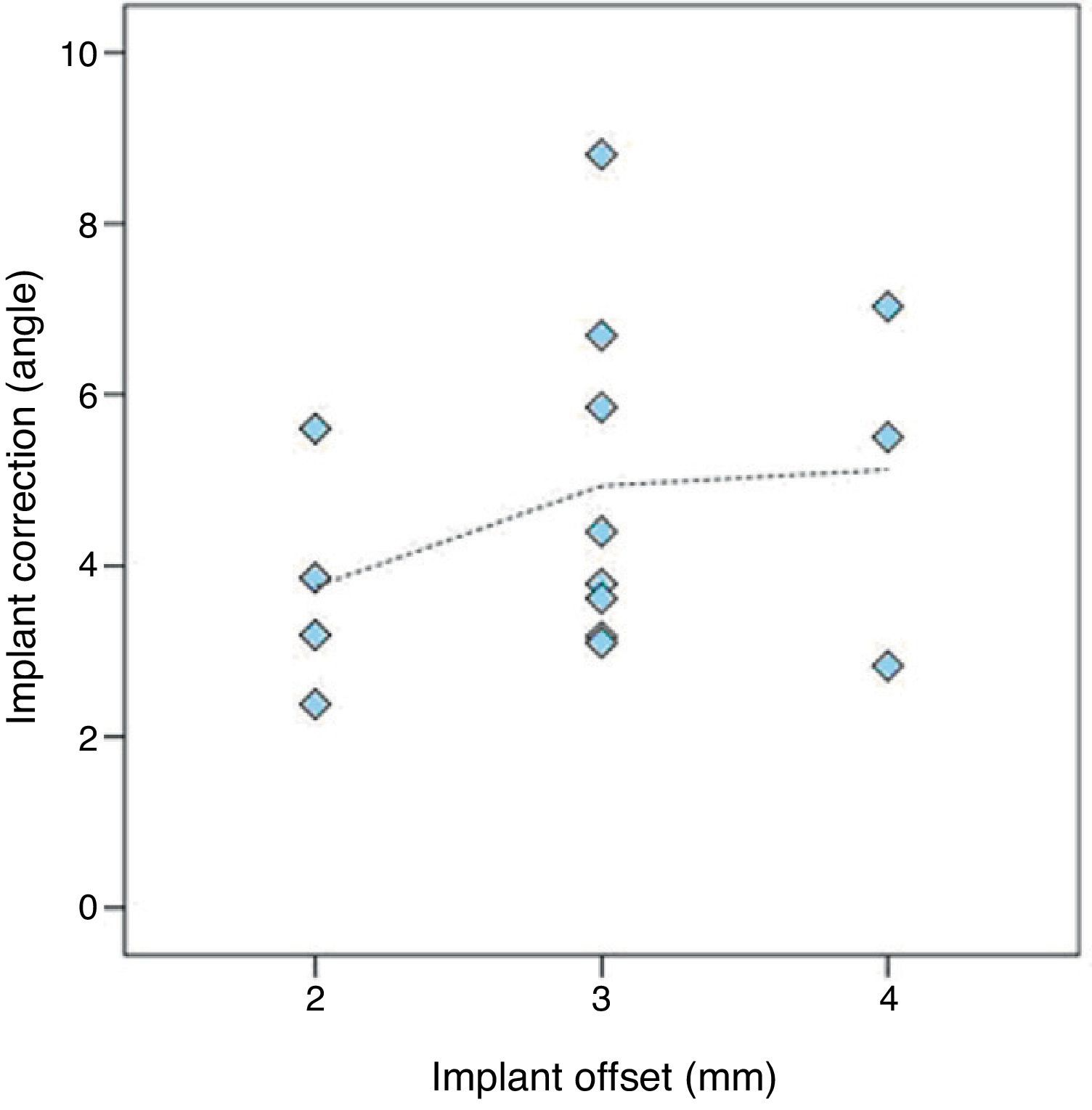
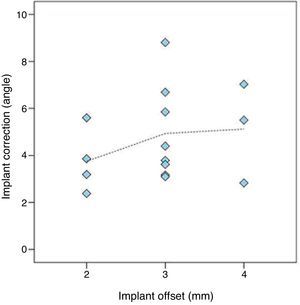
We calculated the correlation coefficient r between the amplitude of the change in alignment (mTFA) and the width of the implant to be 0.274 (Fig. 4). The precision with which the axis correction by surgery with UniSpacer™ was related to the width of the implant used was not significant (P=.162).
DiscussionThe main findings of this study revealed that the axis of the leg was corrected from a mean preoperative value of −5.1°±3.0° to −0.4°±2.3° after surgery (mTFA).
The use of HTO for the treatment of symptomatic malaligned varus knees has become extended and has been well documented for decades: it is an established treatment option. UKA has recently attracted new interest due to improved techniques and prostheses. Numerous reports have shown good long-term results for these 2 methods. However, both methods may cause various problems for patients over time. UKA may result in a loss of bone mass in the medial compartment and, when a conversion to TKA is required, increases the demand for bone grafts or metal wedges.12 HTO affects ligamentous tension and the kinematics of the joint, which may cause difficulties for review TKA: these complications arise most often in a TKA following HTO than in a primary TKA.13 It has been demonstrated that osteoarthritis progresses more rapidly in the contralateral compartment following HTO.14 Moreover, after performing UKA, osteoarthritis progression in the contralateral compartment only takes place in a reduced number of cases.15
Despite having been described over half a century ago, hemiarthroplasty by insertion of a metallic interpositional device is currently experiencing a resurgence as a treatment option for varus unicompartmental osteoarthritis. The aim is to provide a means of treatment which minimises the disadvantages of other procedures. This technique is mainly employed in those cases where the use of HTO is contraindicated or in patients who are too young to undergo TKA. At present, there are very few publications on hemiarthroplasty. The iForma™ device produced by ConforMIS, which is based on the ideas of MacIntosh and McKeever, namely functional attachment of the device to the tibial surface, has received a favourable review in a recent article.7 In general, there are still very few reports which examine the use of the self-centring UniSpacer™ device in medial knee osteoarthritis. There is only 1 study that addresses the issue of correction of malalignment.16 However, its results were based on 40cm radiographs rather than on standing anteroposterior radiographs and, therefore, were not entirely reliable.10,17 The use of the UniSpacer™ device in unicompartmental osteoarthritis was not recommended initially for young and active patients.16 The indication for this procedure is not yet entirely clear because it is only recommended for a small proportion of patients (1%).6 In addition, there are some reports reflecting poor results after surgery due to implant displacement (up to 16%).18
Regarding the level of correction desired, the objective of overadjustment in valgus alignment has been considered desirable for HTO in varus medial gonarthrosis.19,20 The optimum level achieved by UKA is still being investigated,15,21 resulting in most cases in overall mechanical alignment of the knee through the centre of the tibial plateau (zone C), as established by Emerson et al.22 There is hardly any data available on interpositional hemiarthroplasty. The study carried out by Koeck et al. on the iForma™ implant7 showed a mean postoperative alignment (mTFA) of 0.9° and a mean correction of 3.8°. Furthermore, it showed a significant correlation between the level of correction and the width of the implant.
In their study, Cooke et al. described a mean knee alignment (mTFA) of −1.0°±2.8° in normal patients,23 while Moreland considered a mean value of −1.3°±2.0° as normal.10 According to these values, patients treated with UniSpacer™ in our study presented greater correction.
A review rate of 4 out of 15 UniSpacer™ implants within the first 5 years after surgery appears less unfavourable than the results obtained by other studies.8,18 Moreover, we cannot confirm that these reviews were due to a high rate of displacement, as described in these studies, but rather to continuous pain.
We suggest adopting an approach for the evaluation of knee geometry similar to that employed by Emerson et al. in their study of the Oxford prosthesis22 (analysis of the load bearing axis in relation to the tibial plateau), which was fast and well standardised. This would make it easier to prove than with the exclusive use of angles.
Our study has limitations because we analysed a rather limited number of cases (14 patients, 15 knees). Additionally, ligamentous reducibility, factors such as body mass index or limb morphometry were not analysed. However, we have been able to demonstrate a significant and overadjusted correction of moderate varus alignment by arthroplasty with UniSpacer™, which was not correlated with the width of the implant used. During the first year after surgery, we observed a change in varus to a more neutral position which is probably due to the adaptation of the implant to the joint. This effect became partially reversed in subsequent years by another slight change in valgus, which, 5 years after surgery, resulted in a mean leg axis close to that obtained with the initial UniSpacer™ implantation.
ConclusionsThe results of the present study suggest that arthroplasty with UniSpacer™ can achieve realignment in some cases of isolated medial knee osteoarthritis with varus malalignment. This change is independent of the implant used and is maintained over time (5 years). Considering the results obtained, it seems reasonable to perform a slight overcorrection of about 0.5° in order to obviate postoperative adaptation of the implant to the joint.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that the procedures followed were in accordance with the ethical guidelines on responsible human experimentation, with the World Medical Association and with the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Seeger JB, et al. UniSpacer™: corrección de la desalineación en varo en la gonartrosis medial. Resultados preliminares. Rev Esp Cir Ortop Traumatol. 2013;57:15–20.