Post-polio patients present problems such as small and deformed bones, with narrow intramedullary canal and osteoporosis, affecting surgical treatment. The aim of this article is to describe the main preoperative and intraoperative complications of the surgical treatment of fractures in this population.
Material and methodsA retrospective analysis was conducted between 1995 and 2014. Data obtained from the medical records included patient age, fracture pattern (AO/OTA), device used, technical aspects of the surgery that changed compared to a standard procedure, and the presence of intraoperative skeletal complications.
ResultsSixty-four patients with 78 fractures were included in the study. Forty-seven percent of the fractures were at the proximal femur. The main complications of hip arthroplasty (14 patients) were absent hip abductors and intraoperative instability (3), bad cup fixation (3) and intraoperative periprosthetic fracture (2). The main problems of intramedullary nailing were due to a narrow canal and previous bone deformity. Main problems reported when plating included difficulty to fit a precontoured plate, and oversized hardware.
ConclusionGiven the large number of intraoperative complications, in preoperative planning we must include nails of small diameter and length, locking plates and external fixators, and, in the case of hip arthroplasty, long and thin stems and restrictive or dual mobility acetabular systems.
El paciente con secuelas de poliomielitis presenta con frecuencia huesos osteoporóticos, pequeños, deformados, con un canal intramedular estrecho, afectando todo esto al tratamiento quirúrgico. El objetivo de este artículo es describir las principales complicaciones preoperatorias e intraoperatorias del tratamiento quirúrgico de estas fracturas.
Material y métodosSe realizó un análisis retrospectivo entre 1995 y 2014. Los datos obtenidos de las historias clínicas incluyeron la edad del paciente, el patrón de fractura (AO/OTA), el implante utilizado, los aspectos técnicos de la cirugía que cambiaron en comparación con un procedimiento estándar y la presencia de complicaciones intraoperatorias.
ResultadosEn el estudio se incluyeron 64 pacientes con 78 fracturas. El 47% del total fueron fracturas de fémur proximal. Las principales complicaciones de la artroplastia de cadera (14 pacientes) son la ausencia de abductores de cadera y la inestabilidad intraoperatoria (3), la mala fijación del componente acetabular (3) y la fractura periprotésica intraoperatoria (2). Los principales problemas del enclavado son la dificultad debido a un canal medular demasiado estrecho y las deformidades previas. Los principales problemas de la osteosíntesis con placas son la dificultad para ajustar las placas preconformadas y la sobredimensión de las placas.
ConclusiónDado el gran número de complicaciones intraoperatorias, dentro de la planificación preoperatoria debemos incluir clavos de pequeño diámetro y longitud, placas bloqueadas y fijadores externos; y en el caso de realizar una artroplastia de cadera, vástagos largos y finos y sistemas acetabulares restrictivos o de doble movilidad.
Poliomyelitis (polio) is a human infection caused by the poliovirus, a single-stranded RNA enterovirus orofaecally transmitted. The great majority of individuals infected remain asymptomatic. However, in approximately 1% of cases, the virus crosses the haematoencephalic barrier, invades the central nervous system and selectively destroys the motor neurons inside the marrow bone, which leads to a flaccid paralysis of the skeletal muscles.1
Poliomyelitis was prevalent in certain parts of the world during the 1950s,2 and we are now facing the orthopaedic sequelae of this disease. These sequelae appear as a consequence of the neuromuscular paralysis which caused skeletal deformities, joint contractures, joint restriction, insufficient growth of the affected limb and osteoporosis.3,4
Osteoporosis and a higher frequency of falls in polio patients than in the general population leads to greater probability of fractures.3–5 Surgical treatment for these fractures may be difficult due to the before-mentioned osteoporosis, the fact that bones are small in size and occasionally deformed, the existence of sequelae from previous fractures or previous surgery, a narrow intramedullary canal or the absence of strength in the abductor muscles of the hip. Despite these unique characteristics and the complications of their treatment, there are few publications in the literature regarding the treatment of these fractures.
The aim of this article is to describe the key aspects of the surgical treatment of fractures in this population group, which the surgeon should consider to minimise the possible complications during their treatment.
Patients and methodsA descriptive study was made from the data of patients who underwent surgery for limb fractures with poliomyelitis sequelae in our hospitals between January 1995 and December 2014. Inclusion criteria included all fractures of lower limbs with poliomyelitis sequelae surgically treated during the study period. The exclusion criteria included pathological fractures with tumours, fractures of the lower limbs which had been conservatively treated, even when reduction had been performed under anaesthesia.
Data obtained included patient age, location of the fracture, the fracture pattern according to the AO/OTA6 classification system, the type of device used, the treatment methods, the technical aspects of the surgery planned which were altered from the standard procedure and the presence of intraoperative skeletal complications. Imaging studies included plain radiographs of all affected joints. The prosthetic femoral fractures were classified according to the Vancouver system.7
Intraoperative difficulties relating to the orthopaedic procedure in all these groups is described below:
- •
Osteoporosis is defined as a reduction in the trabecular density microscopically assessed which had an effect on surgery, and increased intraoperative complications.
- •
Small or deformed bones are defined when compared with the unaffected contralateral extremity and lead to difficulties in implantation (intramedullary screw or precontoured plate).
- •
A narrow intramedullary canal is defined as lower than 7mm in size measured by standard radiograph, which impedes intramedullary screwing or the insertion of a standard sized femoral stem during hip arthroplasty.
- •
The absence of hip abductors, defined as the presence of macroscopic fatty degeneration in one or more abductor muscles of the hip observed during surgery, which led to a certain level of instability of the hip arthroplasty not connected to the positioning of the implants.
- •
Acetabular dysplasia is defined as an acetabular depth (acetabular width/depth ratio) under 38%.
- •
Difficulty in using precontoured plates is defined as the inability or difficulty in inserting a specific precontoured plate into its appropriate anatomical location.
- •
Intraoperative periprosthetic fracture was defined as any fracture of the femur identified intraoperatively.
Medical or infectious complications were not taken into consideration for the analysis.
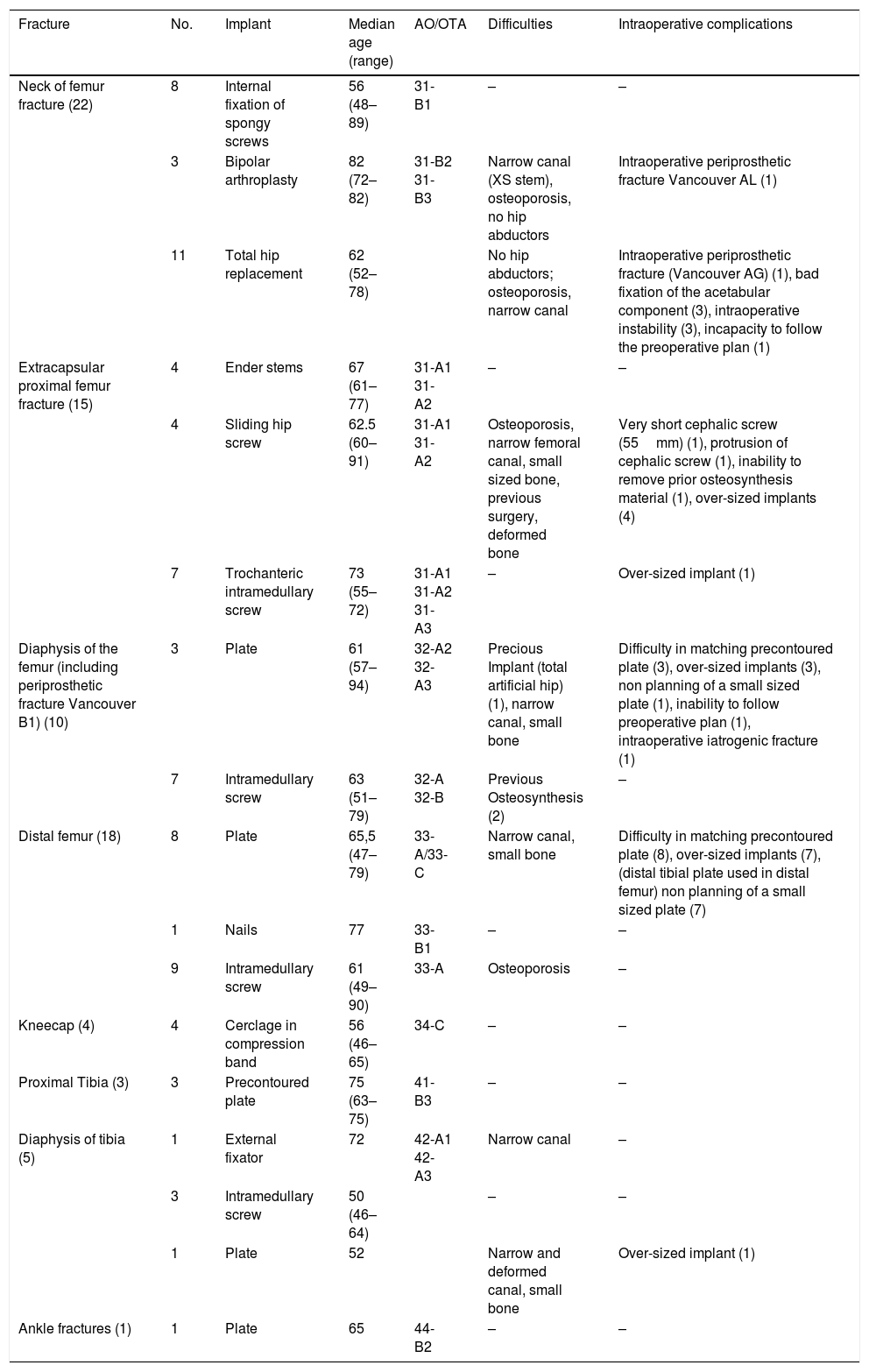
ResultsSixty-four patients were included in the study with 78 fractures of the lower limbs who met with the inclusion criteria. The general results are listed in Table 1. The specific preoperative difficulties and intraoperative complications are described.
Specific difficulties and complications in poliomyelitis patients.
| Fracture | No. | Implant | Median age (range) | AO/OTA | Difficulties | Intraoperative complications |
|---|---|---|---|---|---|---|
| Neck of femur fracture (22) | 8 | Internal fixation of spongy screws | 56 (48–89) | 31-B1 | – | – |
| 3 | Bipolar arthroplasty | 82 (72–82) | 31-B2 31-B3 | Narrow canal (XS stem), osteoporosis, no hip abductors | Intraoperative periprosthetic fracture Vancouver AL (1) | |
| 11 | Total hip replacement | 62 (52–78) | No hip abductors; osteoporosis, narrow canal | Intraoperative periprosthetic fracture (Vancouver AG) (1), bad fixation of the acetabular component (3), intraoperative instability (3), incapacity to follow the preoperative plan (1) | ||
| Extracapsular proximal femur fracture (15) | 4 | Ender stems | 67 (61–77) | 31-A1 31-A2 | – | – |
| 4 | Sliding hip screw | 62.5 (60–91) | 31-A1 31-A2 | Osteoporosis, narrow femoral canal, small sized bone, previous surgery, deformed bone | Very short cephalic screw (55mm) (1), protrusion of cephalic screw (1), inability to remove prior osteosynthesis material (1), over-sized implants (4) | |
| 7 | Trochanteric intramedullary screw | 73 (55–72) | 31-A1 31-A2 31-A3 | – | Over-sized implant (1) | |
| Diaphysis of the femur (including periprosthetic fracture Vancouver B1) (10) | 3 | Plate | 61 (57–94) | 32-A2 32-A3 | Precious Implant (total artificial hip) (1), narrow canal, small bone | Difficulty in matching precontoured plate (3), over-sized implants (3), non planning of a small sized plate (1), inability to follow preoperative plan (1), intraoperative iatrogenic fracture (1) |
| 7 | Intramedullary screw | 63 (51–79) | 32-A 32-B | Previous Osteosynthesis (2) | – | |
| Distal femur (18) | 8 | Plate | 65,5 (47–79) | 33-A/33-C | Narrow canal, small bone | Difficulty in matching precontoured plate (8), over-sized implants (7), (distal tibial plate used in distal femur) non planning of a small sized plate (7) |
| 1 | Nails | 77 | 33-B1 | – | – | |
| 9 | Intramedullary screw | 61 (49–90) | 33-A | Osteoporosis | – | |
| Kneecap (4) | 4 | Cerclage in compression band | 56 (46–65) | 34-C | – | – |
| Proximal Tibia (3) | 3 | Precontoured plate | 75 (63–75) | 41-B3 | – | – |
| Diaphysis of tibia (5) | 1 | External fixator | 72 | 42-A1 42-A3 | Narrow canal | – |
| 3 | Intramedullary screw | 50 (46–64) | – | – | ||
| 1 | Plate | 52 | Narrow and deformed canal, small bone | Over-sized implant (1) | ||
| Ankle fractures (1) | 1 | Plate | 65 | 44-B2 | – | – |
Twenty-two patients presented with an intracapsular fracture of the femur. These fractures were treated with internal fixation in 8 patients and joint replacement in 14, with the decision being personalised and based on the fracture line and the patient's age.
When the joint was replaced, the decision to perform partial or total arthoplasty was taken by the practising physician individually based on patient age and the degree of functional deficit of the affected limb. Thus, 3 bipolar arthroplasties and 11 total arthroplasties were performed.
In the preoperative study, the presence of a narrow canal and osteoporosis (in accordance with the established definitions in the section relating to methods) were the main characteristics observed in the majority of patients. This poor bone quality, together with a certain level of acetabular dysplasia presented complications in achieving stability of the acetabular component in 3 patients, with the use of 3 or more screws required for fixation.
In turn, on the femoral side, this poor bone quality led to the appearance of both periprosthetic intraoperative fractures in 2 patients, one at greater trochanter level with (Vancouver AG) and another at calcar level (Vancouver AL), both of which were treated using cerclage.
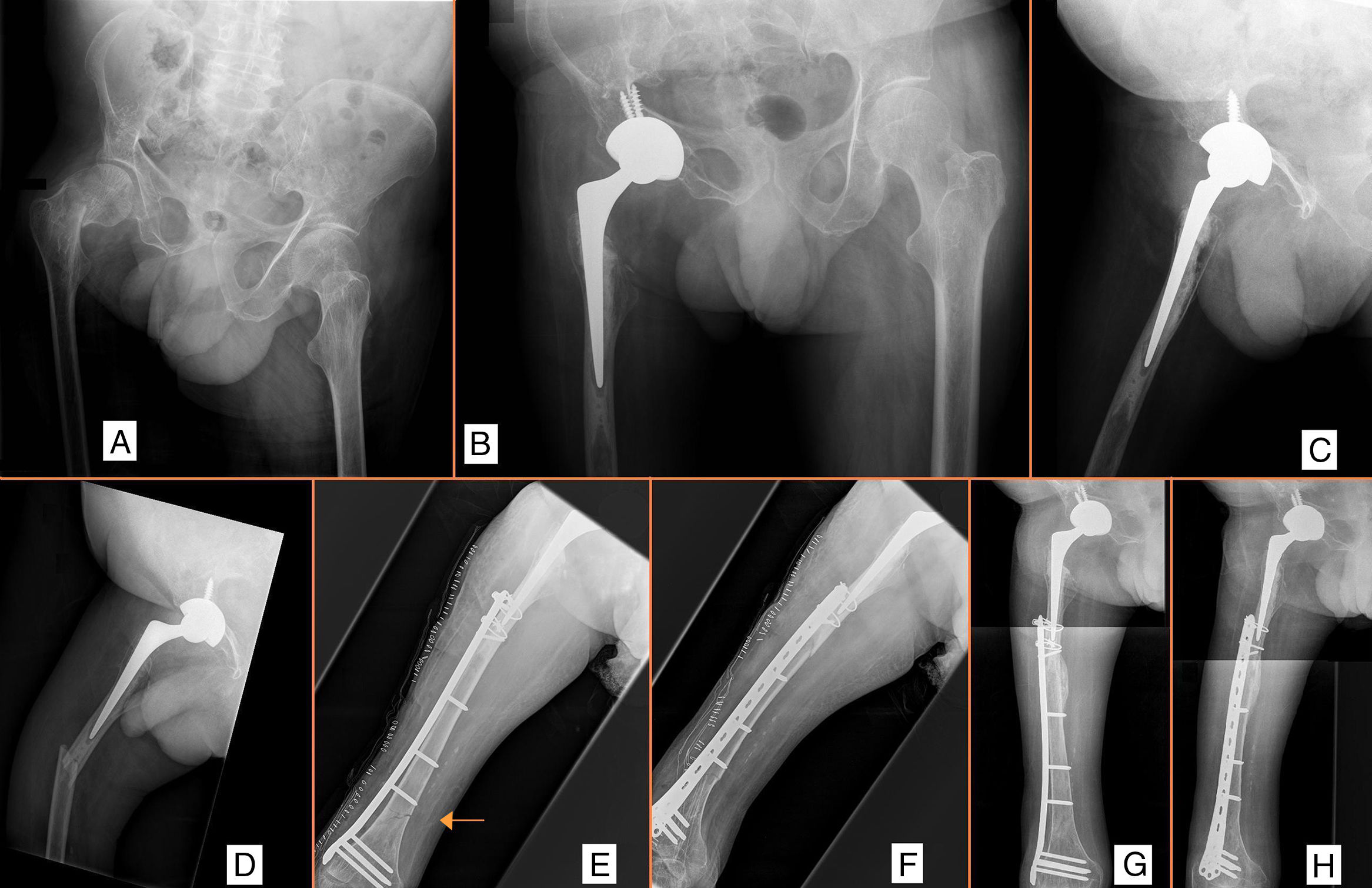
The presence of weakened hip abductors (fatty degeneration) produced a certain degree of intraoperative instability in 3 patients. In one of them, after the reduction of the trial implant, clear instability was observed on insertion of the stem in its anatomical position. In the preoperative planning neither a long stem nor a restrictive implant was included, resulting in the femoral stem being cemented into a higher position to obtain greater tension of the soft tissues and a stable reduction (Fig. 1A–C).
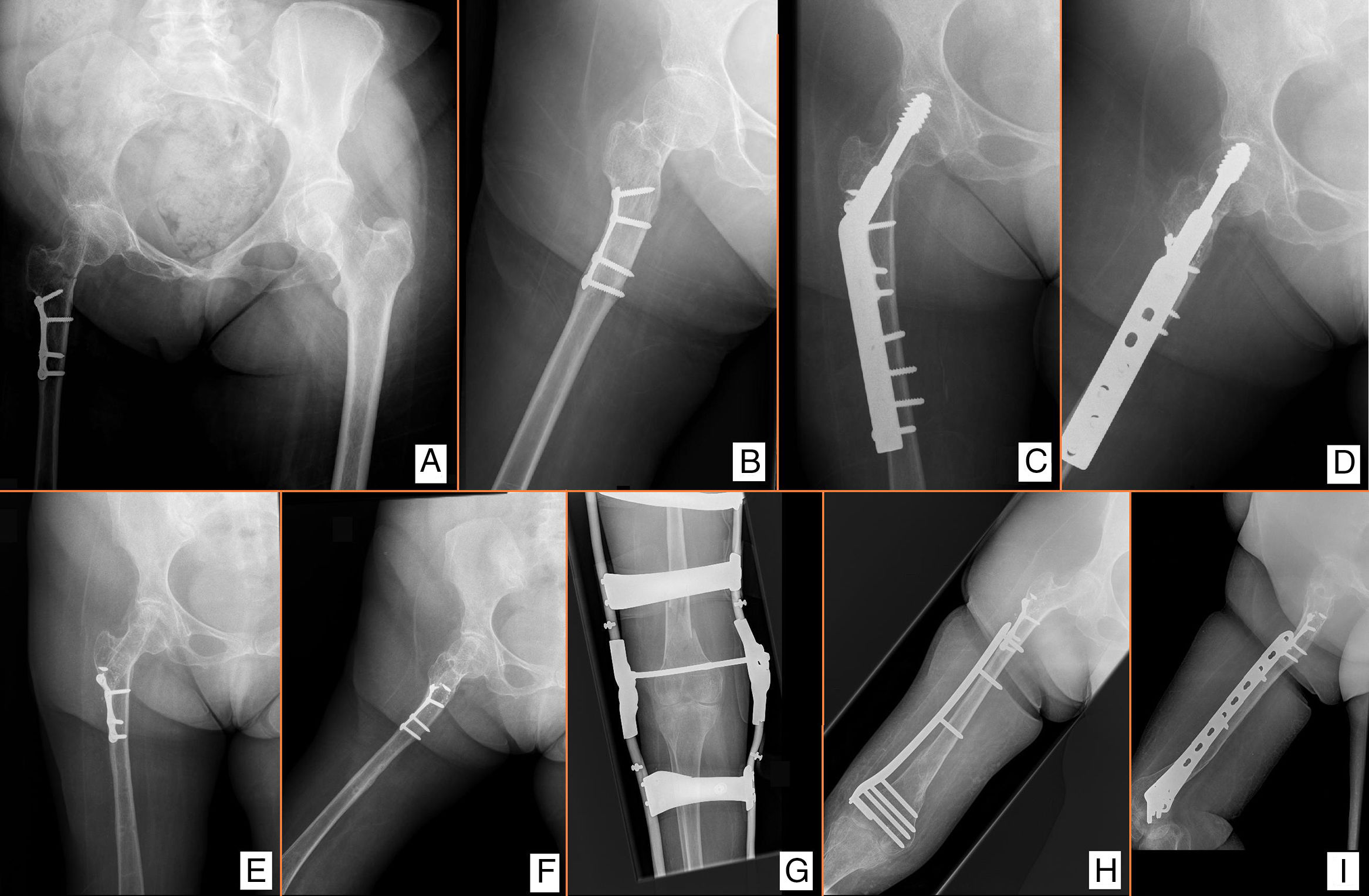
Extracapsular fracture of the proximal femur (AO/OTA 31-A)Fifteen patients suffered from an extracapsular fracture of the proximal femur (five 31-A1, nine 31-A2 and one 31-A3). Extramedullary fixation was chosen for 4 patients, either due to preoperative observation of a narrow canal or the presence of a previous implant which made pinning impossible. In all of them a plate with a sliding hip screw was used, and in all of them the implant was larger than the bone size. The main intraoperative complications recorded were the need for a very short cephalic screw (55mm), the protrusion of the cephalic screw and the inability to remove prior osteosynthesis material (Fig. 2A–F).
Petrochanteric fracture (A, B). The problems observed were: deformity secondary to osteotomy of the proximal femur (B, I), presence of an implant (A, B), suprachondylar osteotomy (G), and osteoporosis (A), small bone (observe over dimension of the implant) (C, D, H, I). Posterior suprachondylar fracture (G–I).
Of the 11 patients treated with the intramedullary implant, we used Ender screws in 4 and intramedullary screws in the remaining 7. Fracture 31-A3 was fixed with a long intramedullary screw after removal of a short supracondylar screw implanted for a previous supracondylar fracture. There were no intraoperative complications in the group of endomedullary screwing, although slightly over-sized implants were observed.
Diaphyseal fracture of the femur (AO/OTA 32)This was present in 10 patients, with pinning as the treatment of choice in 7 cases with a normal diameter of the intramedullary canal, although 2 patients required a prior implant to be removed (short supracondylar screw and proximal femur screw) before surgery.
The plate was the implant of choice in 3 patients, either due to the existence of a previous implant (hip arthoplasty in one patient), or the existence of too narrow a canal.
In the first, a periprosthetic femoral fracture (Vancouver B1) required fixation with a long precontoured plate. A complication occurred as during handling of the limb an iatrogenic transversal fracture presented, bridged by the plate (Fig. 1D–H).
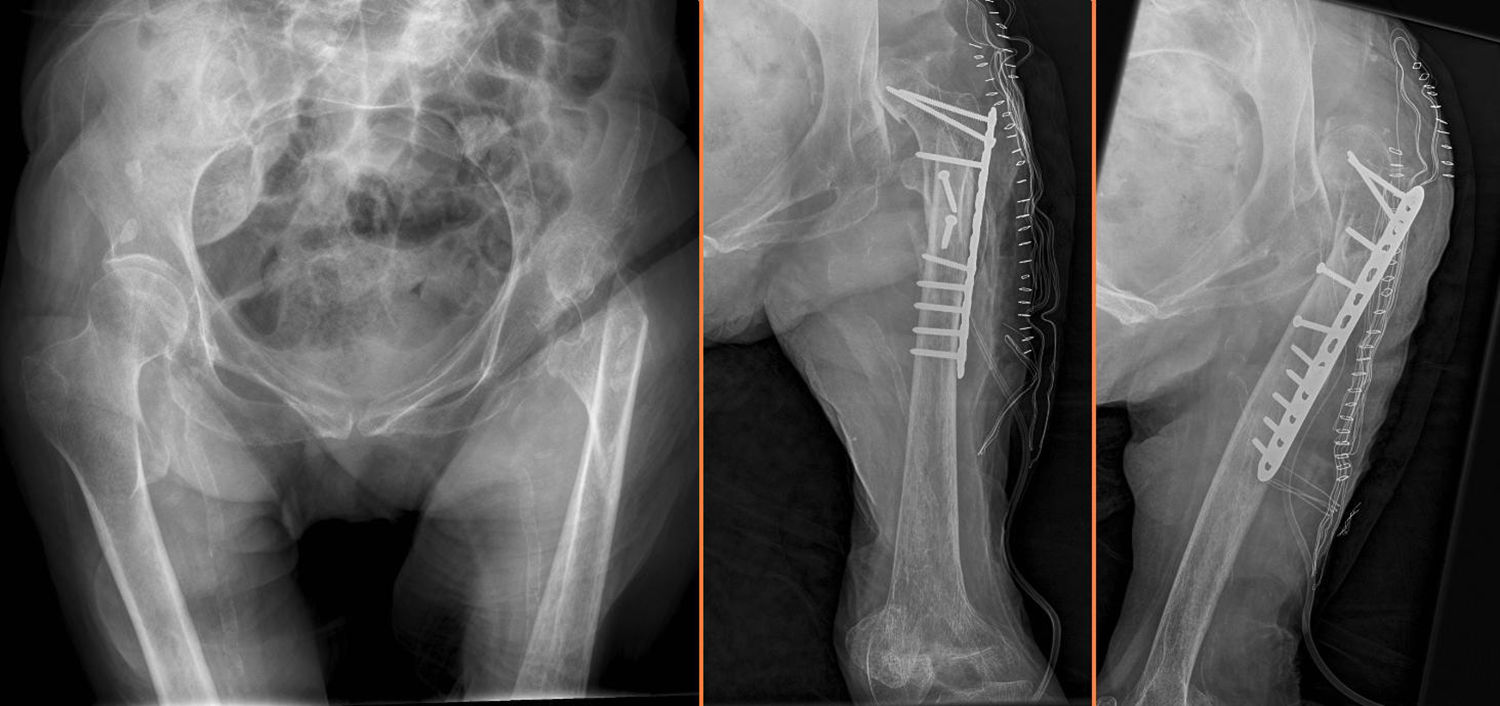
In 2 patients with diaphyseal fractures with too narrow a canal for pinning a sliding screw hip plate was chosen as treatment. In one of them a highly flat, slim femur prevented the use of a sliding screw hip plate or a long screw and a standard 3.5 locking plate was used (Fig. 3).
Distal femur fracture (AO/OTA 33)Eighteen patients presented with a distal femur fracture. One unicondylar fracture (AO 33-B1) was treated with cannulated spongy screws.
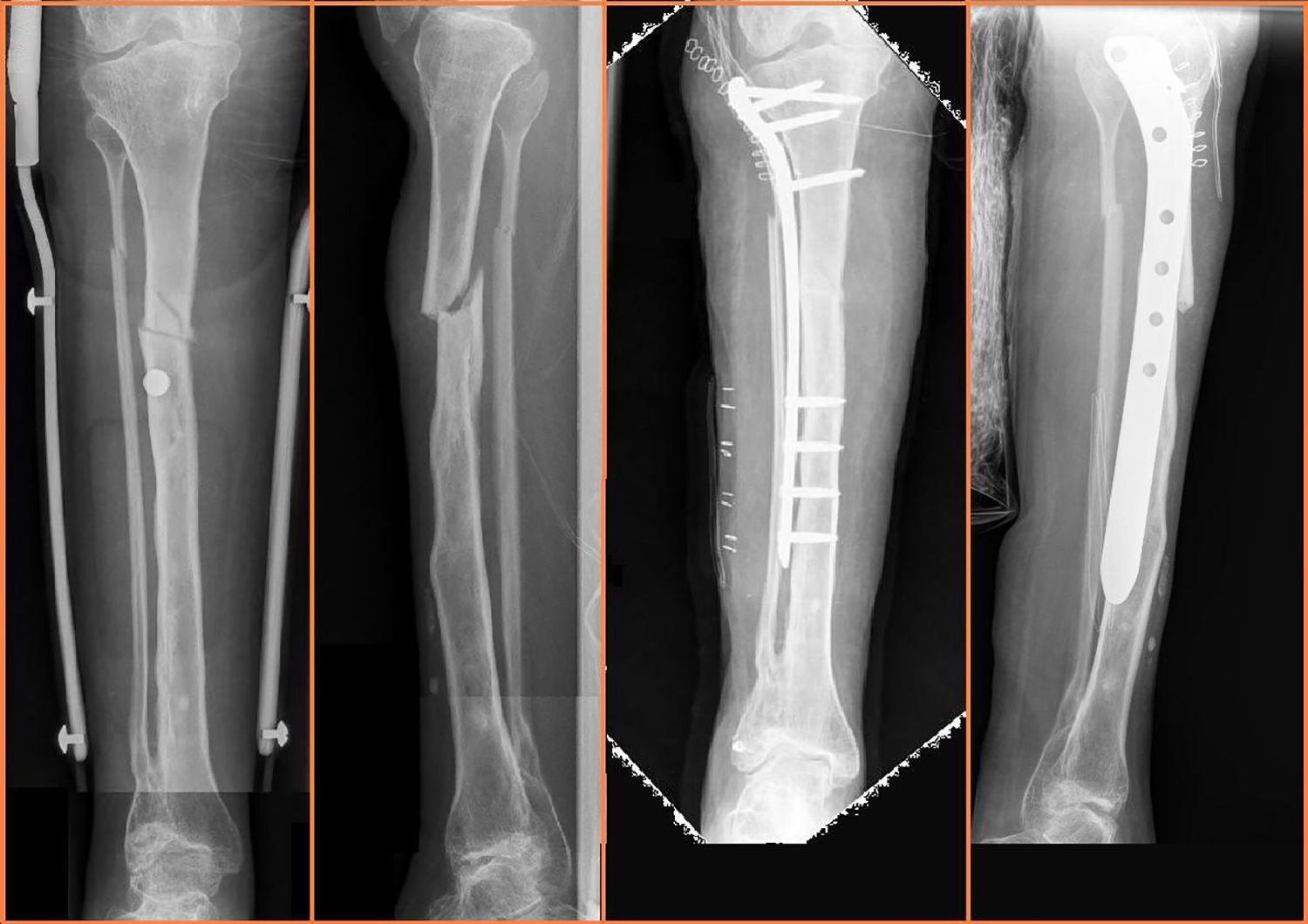
Nine supracondylar fractures (AO 33-A1 and AO 33-A2) were treated with the use of supracondylar retrograde screws and 8 supracondylar and supraintercondylar fractures (AO/OTA 33-A and 33-C) were treated with locking plates. In7 patients precontoured distal femur locking plates were used, over-sized in all cases, which led to postoperative irritation of soft tissues (Fig. 4, left). Due to the failed adaptation of the distal femur plate and its large size, in one case a recontoured plate of distal tibia was used in the distal lateral femur. This enabled better adaptation in the small bone, whilst the locking screws enabled sound fixation in the osteoporotic bone (Fig. 4, right).
Proximal fracture of the tibia (AO/OTA 41-B3)Three patients were treated with standard locking plates, and there were no intraoperative complications.
Diaphyseal fracture of the tibia (AO/OTA 42)Of the 5 patients who presented with a diaphyseal fracture of the tibia, pinning was used in 3 of them, with no intraoperative complications. In the other 2, the main problem was a narrow, deformed canal bone from previous fractures, which forced us to use a monolateral external fixator in one patient and a precontoured proximal tibia plate in the other (Fig. 5).
Fracture of the kneecap and the ankle (AO/OTA 34-C and 44-B2)These were treated with standard procedures and there were no intraoperative complications.
DiscussionThe World Health Organisation has eradicated poliomyelitis from the majority of countries in the world following its eradication programme which was initiated in 1988. However, in some developing countries this was only recently achieved (South East Asia has been considered polio free since March 2014), and endemic transmission continues in Pakistan and Afghanistan. As a result, up to 200,000 new cases may occur every year worldwide.8
As patients with polio sequelae age, osteoporosis, partial paralysis of the limbs and mobility limitations predispose them to more frequent falls and fractures in the affected limb. Recent publications report fall rates of 64–74% in the year prior to the fracture and up to 35% of these patients have a history of previous fractures resulting from a fall.3–5 Most treatment for these fractures is conservative, since the benefits of surgical treatment may be low due to the pre-existing functional deficit of the affected limb. However, when performed, internal fixation in these patients may be difficult due to the special considerations of the bone, which may be small, extremely osteoporotic and deformed resulting from previous fractures or operations during childhood (Fig. 2B and I).
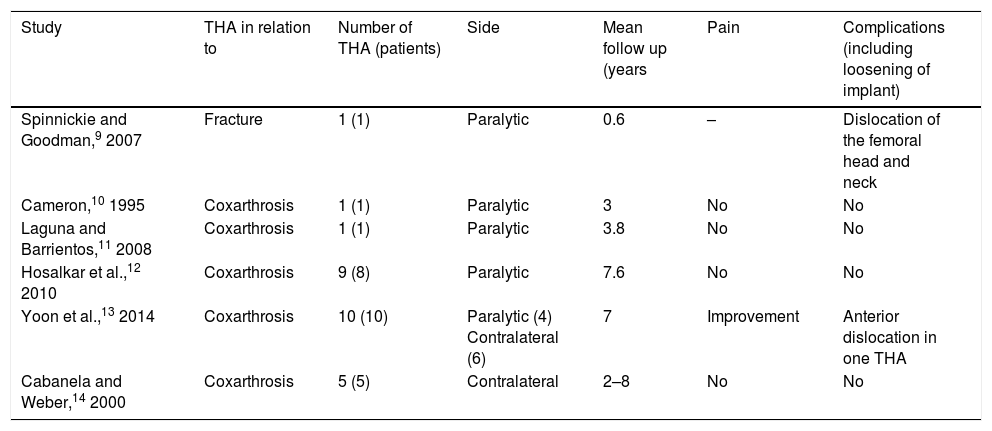
Intracapsular fractures of the proximal femurVery few studies have been published on total hip arthroplasty (THA) in patients with poliomyelitis. Available evidence is limited mostly to small series and isolated cases.9–14 However, in one of the largest studies on THA in patients with post polio syndrome,12 the authors recorded the data of 8 patients prospectively with 9 THA; there were no dislocation episodes and no significant changes were mentioned regarding postoperative muscular strength.
Table 2 summarises the available data published on THA in patients with residual poliomyelitis. Current evidence reports a lower complication rate than expected.
Total hip replacement studies in patients with poliomyelitis sequelae.
| Study | THA in relation to | Number of THA (patients) | Side | Mean follow up (years | Pain | Complications (including loosening of implant) |
|---|---|---|---|---|---|---|
| Spinnickie and Goodman,9 2007 | Fracture | 1 (1) | Paralytic | 0.6 | – | Dislocation of the femoral head and neck |
| Cameron,10 1995 | Coxarthrosis | 1 (1) | Paralytic | 3 | No | No |
| Laguna and Barrientos,11 2008 | Coxarthrosis | 1 (1) | Paralytic | 3.8 | No | No |
| Hosalkar et al.,12 2010 | Coxarthrosis | 9 (8) | Paralytic | 7.6 | No | No |
| Yoon et al.,13 2014 | Coxarthrosis | 10 (10) | Paralytic (4) Contralateral (6) | 7 | Improvement | Anterior dislocation in one THA |
| Cabanela and Weber,14 2000 | Coxarthrosis | 5 (5) | Contralateral | 2–8 | No | No |
In our series, instability is the main complication, and was observed in 3 of 11 patients, together with intraoperative periprosthetic fractures. Current evidence reports that modular, constricted or dual mobility implants, associated with liberation from soft tissues when appropriate must be considered for these patients.14
Extracapsular fractures of the proximal femurThe main problem found on treating fractures of the peritrochanteric region was the presence of a very narrow canal, which prevented the use of a proximal femoral screw. To resolve this problem treatment of these fractures has been described in the references, both with plates and external fixation. Catagni et al.15 defended the benefits of external fixation as a fixation option in proximal femur fractures in patients with polio. The main advantage is the possibility of inserting Schanz screws at different angles and number, depending on the width of the femoral neck and the width of the canal. The main disadvantage in this specific group is the potential interference when the patient is a regular use of orthotics (Fig. 2G).
There are several authors16 who defend the use of locking compression plates in these fractures, since they may be adjusted to the shape of the bone and are indicated in osteoporotic bone.
Current evidence17 supports the use of sliding screw hip plates for fixing the most common extracapsular hip fractures. In our experience, the main problem for use is the discrepancy in size between the femur and plate and the need for shorter than usual cephalic screws. Since one of the most common problems is this discrepancy, internal fixation devices designed for the paediatric patient could be included in the preoperative planning. In this way, several plates designed for paediatric hip surgery available in different angulations (from 100° to 140°), would be a good treatment option for internal fixation of extracapsular hip fractures in these patients.18
Intramedullary screwingAlthough intramedullary screwing was possible in our series for the majority of patients, it may be technically impossible or contraindicated in this population due to the presence of previous deformities or a narrow canal. In these cases, excessive reaming intended to make the standard femoral screw smaller may lead to heat-induced necrosis of the bone.19
In these cases, paediatric screws, designed for use in teenagers and adult patients small in stature, may be recommended.20
When these paediatric screws are not available, the new generations of intramedullary screws with multiple locking options in different planes in the proximal and distal end may be indicated in selected cases. Lee et al.21 reported the use of a tibia screw as a treatment option for femur fractures with a narrow medullary canal, highlighting the importance of a preoperative assessment of the medullary canal.
In cases of extremely narrow canals, Gupta et al.22 match the long bones of the patient with polio to long paediatric bones, and describe the use of elastic endomedullary nailing systems in the femur as a reasonable option in these patients.
Osteosynthesis with platesAlthough osteosynthesis with minimally invasive precontoured locking plates in a patient with too narrow an intramedullary canal has gained popularity in recent years with satisfactory clinical results,23,24 in our experience, the main problem is the adaptation of the plate to the bone. The plates precontoured for an anatomical region are generally too large for these patients, and surgeons are forced to use smaller non-specific plates and to contour them. Wang et al.25 describes a series of 19 patients treated with precontoured locking plates, with no major complications. El-Sayed Khalil,16 in a series of 13 patients, describes complications to adapt the plates. In 6 cases, the small size of the femur only permitted the use of straight locking plates instead of those specifically designed for the proximal or distal femur, and in 6 cases the plate had to be moulded to fit around the bone shape.
Although osteosynthesis with a plate is technically more demanding than screwing, due to these problems, it has to be considered as a viable alternative in all of these patients if screwing is not possible.
Our study had several limitations. Firstly, it was a retrospective descriptive study, with no group control, and our results would need confirming through a more extensive series. Secondly, the sample of each fracture types is small, due to the low rate of these fractures. However, compared with the current literature this series was large, and met its objective in describing the main complications of surgical treatment of fractures in this population group.
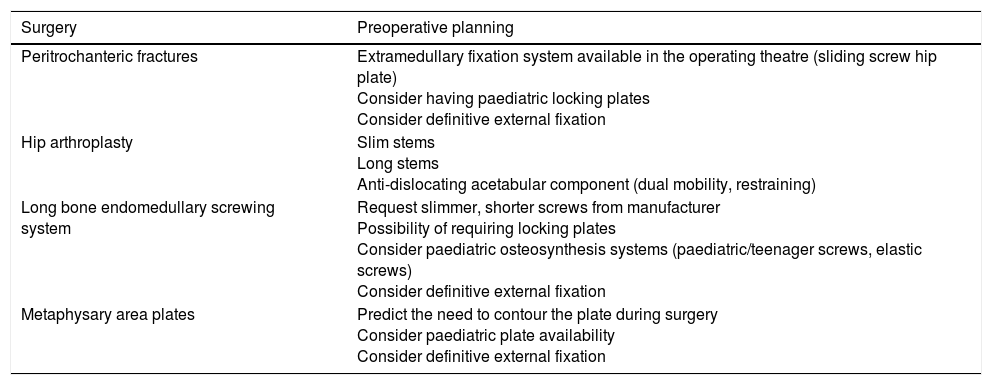
ConclusionSurgical treatment of fractures of lower limbs in patients with poliomyelitis sequelae presents with a large number of complications, and good surgical planning is therefore essential (Table 3).
Preoperative planning.
| Surgery | Preoperative planning |
|---|---|
| Peritrochanteric fractures | Extramedullary fixation system available in the operating theatre (sliding screw hip plate) Consider having paediatric locking plates Consider definitive external fixation |
| Hip arthroplasty | Slim stems Long stems Anti-dislocating acetabular component (dual mobility, restraining) |
| Long bone endomedullary screwing system | Request slimmer, shorter screws from manufacturer Possibility of requiring locking plates Consider paediatric osteosynthesis systems (paediatric/teenager screws, elastic screws) Consider definitive external fixation |
| Metaphysary area plates | Predict the need to contour the plate during surgery Consider paediatric plate availability Consider definitive external fixation |
Possible intraoperative problems in surgery need to be anticipated. Several osteosynthesis systems need to be made available in the operating theatre to resolve possible problems with the planned system, such as screws which are small in diameter and length, locking plates and external fixators, as well as preparing double and/or implant plates in unusual places. When performing a hip arthoplasty, long, slim stems and restrictive or dual mobility acetabular systems should be included in preoperative planning.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments have been conducted on humans or animals for this research study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Mingo-Robinet J, Alonso JA, Moreno-Barrero M, González-García L, Garcia-Virto V, Aguado HJ. Aspectos técnicos y complicaciones en el tratamiento de las fracturas de los miembros inferiores con secuelas de poliomielitis. Rev Esp Cir Ortop Traumatol. 2018;62:257–266.