To evaluate the clinical and radiological results of the surgical treatment of type III acromioclavicular dislocations using the Weaver–Dunn technique in the delayed phase.
Material and methodA non-randomised controlled retrospective observational study of 38 patients operated between January 2006 and December 2014. We excluded 10 patients due to death or non-localisation. We collected demographic data, time to intervention, complications, analysing the Visual Analogue Scale, DASH and Oxford Shoulder Score and the updated radiological result.
ResultsMean age of patients with right-dominant shoulder affected in 71% of cases predominantly by non-level falls was 35. 70% of the cases had subjective perception of both recovery of strength and disappearance of deformity. Full radiological reduction was observed in 95% of the cases with the appearance of mild osteoarthritis in 44% and moderate osteoarthritis in 5.6%. The results of the DASH presented values of 12.939 (±16.851) and the OSS of 42.736 (±7.794), indicating satisfactory articular function.
DiscussionThe data from this study shows similar results to previous studies regarding subjective recovery of strength, maintenance of anatomical reduction, functional test results and efficacy of the Weaver–Dunn technique.
ConclusionsThe modified Weaver–Dunn technique provided good clinical and radiological results with patient reincorporation to their usual activities and maintenance over time.
Valorar los resultados clínicos y radiológicos del tratamiento quirúrgico de las luxaciones acromioclaviculares tipo III mediante la técnica de Weaver-Dunn en fase diferida.
Material y métodoEstudio observacional retrospectivo controlado no aleatorizado de 38 pacientes intervenidos entre enero de 2006 y diciembre de 2014. Se excluyeron 10 pacientes por fallecimiento o no localización. Se recogieron datos demográficos, tiempo hasta la intervención y complicaciones, analizando la Escala visual analógica, DASH y Oxford Shoulder Score y el resultado radiológico actualizado.
ResultadosEdad media de los pacientes de 35 años con hombro derecho-dominante afectado en un 71% de los casos predominantemente por caídas no a nivel. El 70% de los casos tenían percepción subjetiva tanto de recuperación de fuerza como de desaparición de deformidad. Se objetivó reducción completa radiológica en un 95% de los casos, con aparición de artrosis leve en un 44% y moderada en un 5,6%. Los resultados del DASH presentaron valores de 12,939 (±16,851) y el OSS de 42,736 (±7,794), indicando una función articular satisfactoria.
DiscusiónLos datos de este estudio muestran similitud en cuanto a resultados de estudios anteriores en lo que respecta a la recuperación subjetiva de la fuerza, mantenimiento de la reducción anatómica, resultados de test funcionales y eficacia de la técnica de Weaver-Dunn.
ConclusionesLa técnica de Weaver-Dunn modificada aportó buenos resultados clínicos y radiológicos con reincorporación del paciente a sus actividades habituales y su mantenimiento a lo largo del tiempo.
Acromioclavicular joint injuries are relatively common, especially after sports shoulder trauma. Acromioclavicular dislocations account for about 12% of dislocations around the shoulder.1 The most common mechanism of injury is usually direct trauma.
Rockwood described 6 types of acromioclavicular dislocations. Types I and II 1 and 2 are incomplete injuries and are usually treated conservatively. There is consensus that types IV to VI should be treated surgically; however, there is controversy regarding the most appropriate treatment for type III. In Type III the coracoclavicular ligaments are completely torn and the deltoid and trapezium fascia are intact, which can cause the clavicle to displace upwards between 25% and 100% of the normal distance.2 Conservative treatment of this type of acromioclavicular dislocation can have good outcomes for some patients, causing them little pain, little functional impotence, and enable them to return to their usual activities. There is no evidence of predictive factors of a poor outcome of conservative treatment; age, dominance, level of activity and aesthetic deformity must be considered. Surgical treatment is clearly indicated in the case of panclavicular dislocation or floating clavicle.2
In 2014, the ISAKOS Upper Extremity Committee of experts proposed a modification to Rockwood's classification.3 They differentiated a type IIIA, or stable injury, without overriding of the clavicle on the cross-body adduction Basamania (Alexander) view and no scapular dysfunction: and a grade IIIB, or unstable, injury if evidence persists of an overriding clavicle and scapular dysfunction.
A review of the literature found no unified consensus on the treatment indicated for type III AC dislocation, probably because the great majority of studies show a III or IV level of evidence, presenting retrospective, case-series studies that do not offer appropriate guidance in terms of therapeutic decision-making.4–8
Acute fixation of the joint produces excellent outcomes.9 Dislocation is considered chronic when more than 6 weeks have passed since the injury, since then there will have been partial or total reabsorption of the ligaments, which lose their capacity to heal, and therefore their repair is insufficient.10 The coracoclavicular ligament reconstruction technique most used is that described by Weaver and Dunn in 1972.11 Open reduction and internal fixation with Kirschner wires (early repair for acute injuries) and modified Weaver–Dunn technique (differed reconstruction in chronic injuries) are the 2 most used surgical procedures. Other surgical techniques, such as Bosworth screw fixation, suture anchors, hook plate and arthroscopy assisted surgery have been more widely used in recent years.11
The aim of this study was to assess the outcomes of surgical treatment for type III AC joint dislocation, treated in the chronic phase. Although the other surgical techniques mentioned (ORIF with wires, Bosworth) have been used in our environment, for a great many of our patients we opt for modified Weaver–Dunn reconstruction. We explain both treatment options to the patient. The patients who opt for conservative treatment are reviewed after 4–6 weeks, and if their pain or functional incapacity to return to work persist, we offer them a modified Weaver–Dunn reconstruction.
Material and methodsAn observational, retrospective, controlled, non-randomised study was undertaken on patients operated in the Hospital FREMAP Majadahonda using the modified Weaver–Dunn procedure after the first 6 weeks of type III AC dislocation.
The inclusion criteria were: patients of working age (18–65 years), type III AC dislocations treated conservatively from the start, no other disorders of the affected shoulder, time of onset over 6 weeks previously, persistence of pain or incapacity to return to work, and able to respond to the questionnaires. The study was approved by the institution's Clinical Research Ethics Committee.
The following variables were collected from the sample: age, sex, occupation, mechanism of injury, dominance, time interval from injury to surgery, and total duration of follow-up.
A retrospective search was performed of the hospital's clinical histories for patients operated from January 2006 to December 2014 who met all the inclusion criteria of the study.
Initially, 38 patients were included. Ten patients were excluded because they could not be located in person or by telephone, one case had died, 3 who were not Spanish nationals had possibly returned to their country of origin, and the telephone numbers of the remaining 6 were incorrect.
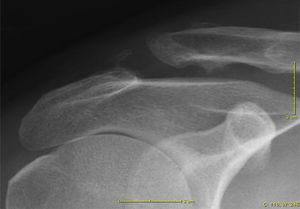
The results of the visual analogue pain scale before and after surgery, DASH and Oxford Shoulder Score (OSS) and postoperative functional tests, the subjective impression of recovery of strength and aesthetic appearance, and the employment outcomes were collected by telephone survey. A current X-ray was performed assessing the grade of reduction, arthritis, ossification of the CC ligaments and degree of osteolysis as described in the article by Calvo et al.12 (Fig. 1).
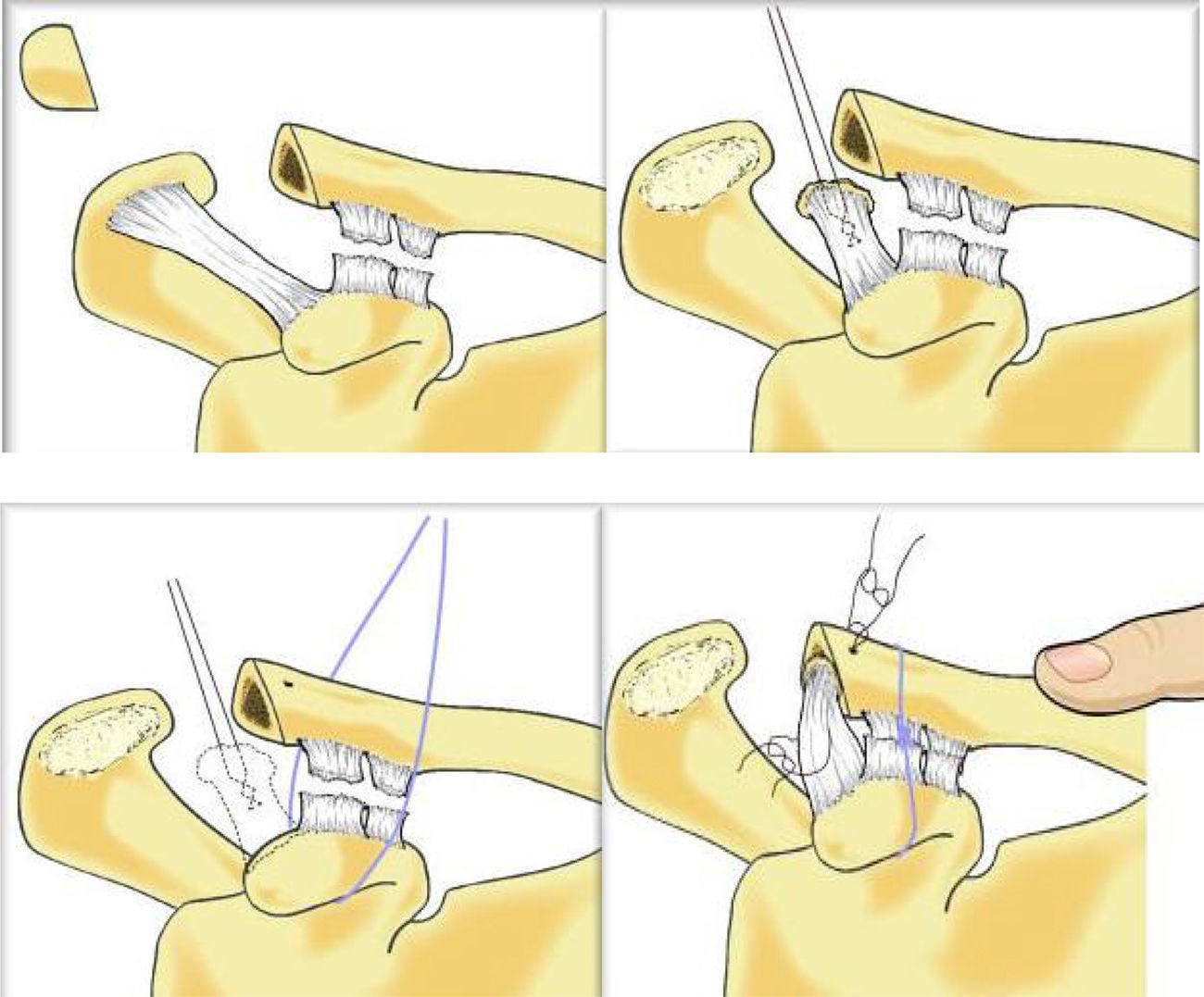
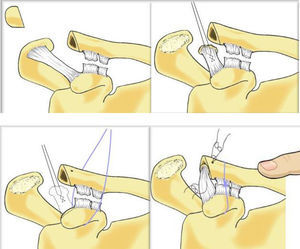
All the patients underwent the modified Weaver–Dunn technique described by Copeland in 1995.13 A strap incision of about 5cm was made at 1cm medial to the AC joint. The coracoacromial ligament of the acromial insertion was disinserted and dissected maintaining the insertion in the coracoid. Resection was performed 1cm from the distal end of the clavicle, the joint was reduced with traction to the ligament to calculate the appropriate length to maintain this reduction. The proximal end of the ligament was sutured with nonabsorbable suture. Two orifices were created in the upper cortical bone of the clavicle and the ligament inserted through the medullary canal taking the sutures out through the upper cortical bone to tie them while the joint was reduced. Copeland describes reinforcing the repair with PDS sutures around the clavicle and below the coracoid (Fig. 2). In our cases, various methods of reinforcement were used to maintain the reduction: coracoacromial loop, Dog Bone Button system, Kirschner wires, etc.
Weaver–Dunn tecnique.15
Anteroposterior X-rays of the clavicle and at 20° cephalic tilt were taken for the postoperative study and the criteria of Calvo et al.,12 were used in the radiological assessment:
- -
In assessing the degree of reduction of the AC joint, it was considered reduced when there was no separation between the ends; considered partially dislocated if there was displacement of less than 50% of the joint surface and dislocated if the displacement was greater than 50% of the joint surface.
- -
No signs of arthritis were considered no arthritis (Fig. 3), narrowing in the joint space with subchondral sclerosis was considered mild arthritis, moderate arthritis if there were osteophytes, and severe arthrosis if there was major deformity in the joint.
- -
Any calcium deposits along the course of the coracoclavicular ligaments were assessed as ossification of the coracoclavicular ligaments.
- -
Evidence of areas of demineralisation in varying degrees in the distal end of the clavicle was recorded as osteolysis.
SPSS 20.0®was used for the statistical analysis. The qualitative variables were presented with absolute frequencies and percentages, and mean and standard deviation for the quantitative variables. Wilcoxon signed-rank and the student's-t test were used for the comparative variables. Results with a p value <.05 were considered statistically significant.
ResultsOf the 28 patients in the study, 24 were male (85.7%) and 4 female (14.3%), with a mean age of 34.96 years (±9.682 years) and range of 41 years, the minimum age was 18 and the maximum 59 years, all were of working age.
The right-dominant shoulder was affected in the majority (71.4%).
The patients’ follow-up was a mean of 73 months (6.1 years (±32.12 months), with a range of 109 months (126 months–17 months), the longest follow-up was 126 months (10.65 years) and the shortest follow-up was 17 months (1.5 years).
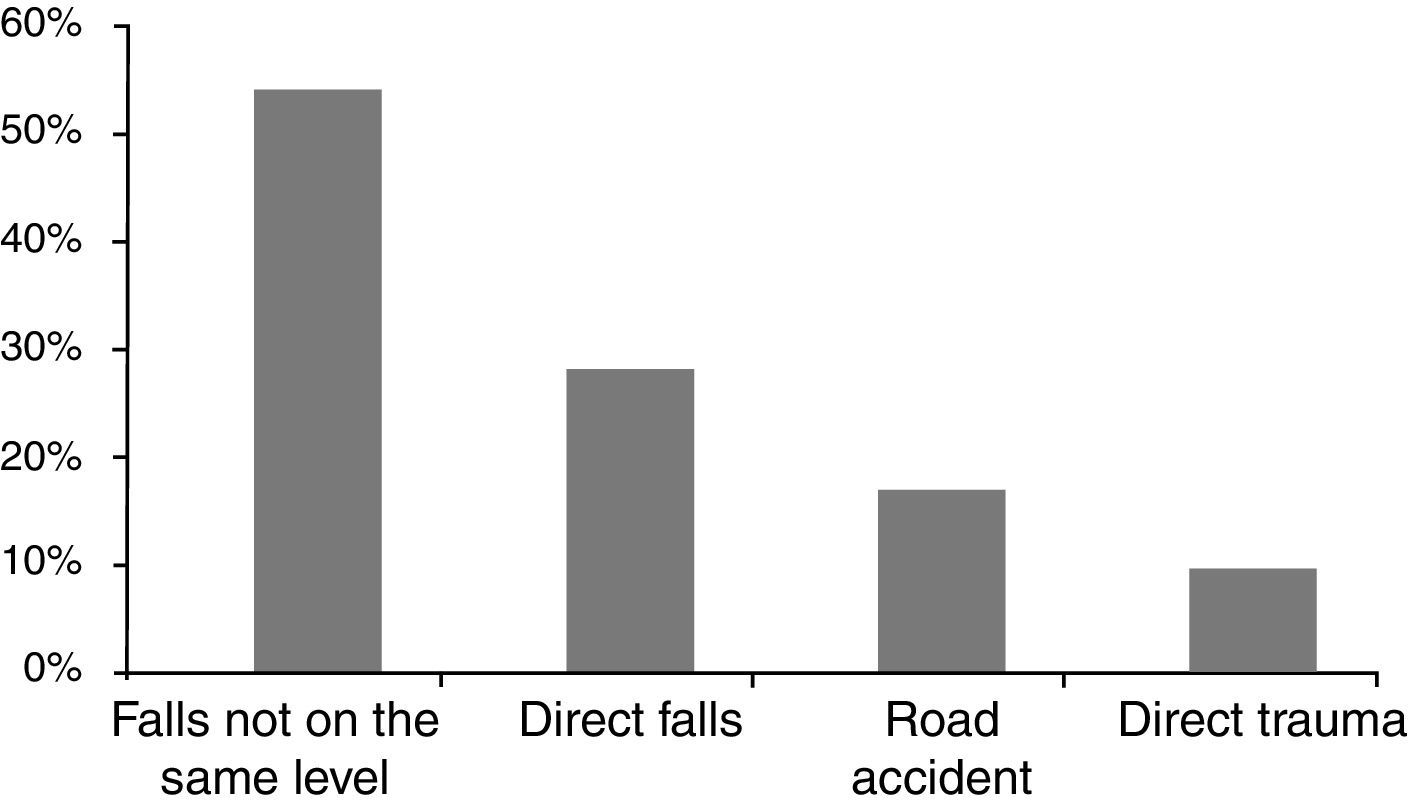
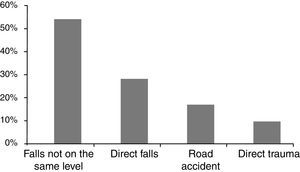
The acromioclavicular injuries were predominantly a result of falls not on the same level (51.9%). They were caused by falls on the same level in 7 (25.9%), by a road traffic accident in 4 cases (14.8%) and by direct trauma in 2 patients (7.4%) (Fig. 4).
The waiting time until surgery from the time that the injury occurred was a mean 18.54 weeks (±21.48 weeks), with a range of 84 weeks, the longest waiting time was 88 weeks and the shortest was 6 weeks.
Twenty-one patients had no complications (75%), only 7 of the patients had complications (25%), 3 of whom had superficial infections (10.7%) that resolved completely with antibiotherapy, 2 patients had plate migration (7.1%), with no symptoms and therefore the plate was not removed. Two patients had to be reoperated due to pain and instability of the wrist, one patient with coracoacromial reinforcement with semitendinosus, and the other with palmaris longus and 2 Kirschner wires.
In the subjective recovery of strength prior to surgery, 19 patients (67.9%) perceived that they had recovered strength, whereas only 9 did not (32.1%). In the subjective perception of elimination of deformity after the surgery, 20 patients perceived their joint as reduced (71.4%), whereas 8 did not (28.6%).
All the patients returned to their previous jobs, except one who had a total permanent disability.
The radiological results were complete reduction for 17 patients (94.4%) and only one patient had partial dislocation of the joint (5.6%) with subjective perception of complete reduction.
Nine patients had no arthritis (50%), 8 patients had mild arthritis (44.4%) and only one patient had moderate arthritis (5.6%).
Ossification of the coracoclavicular ligaments was observed in 6 patients (33.3%) and signs of osteolysis in 5 (27.8%), and both appeared concomitantly in one patient (3.6%).
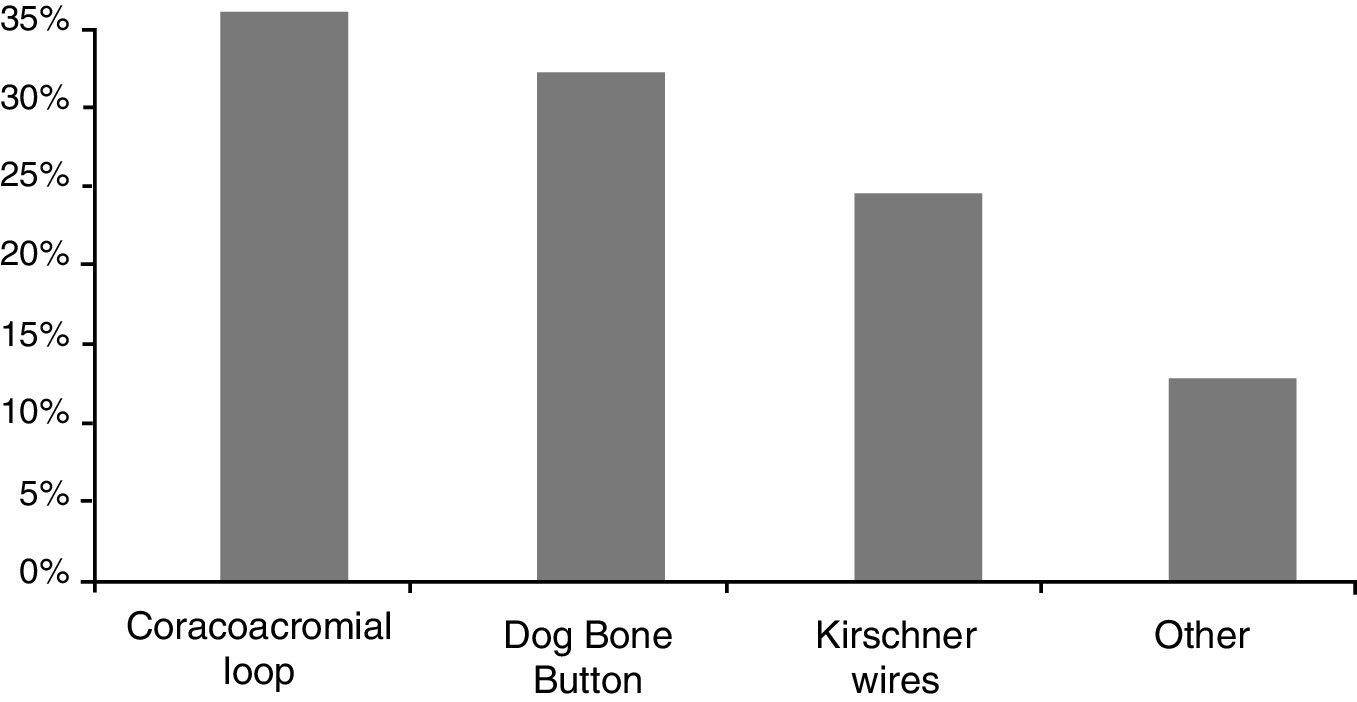
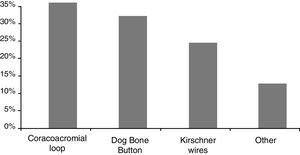
Coracoacromial reinforcement was used as fixation in 9 patients (34.6%), the Dog Bone Button was used in 8 of the patients (30.8%), Kirschner wires were placed in 6 (23.1%) and other fixation systems were used in 3 patients (11.5%) (Fig. 5).
Coracoacromial loop was performed using different types of suture (parenchyma suture, Fibre, Tape, Safil, Vicryl). Coracoclavicular screw, the MINAR® system and Endobutton® were other fixation systems used.
The mean of the postoperative DASH test was 12.939 (±16.851) and the postoperative OSS test produced a mean value of 42.736 (±7.794).
The VAS pain scale before the surgery was taken from the clinical history (6.89), and the value after treatment (1.79); the results were statistically significant (p<.001).
The Dog Bone Button fixation system was compared and the others in the functional tests (VAS, DASH or OSS), there were no statistically significant results between the 2 groups (previous VAS p=.345, current VAS p=.793, DASH p=.860, OSS p=.989).
We also wanted to assess whether the patients with the poorest subjective outcomes (recovery of strength and subjective appearance) were the same as those with poor outcomes in the functional tests or whether there really was no correlation between the subjective and the objective; no statistically significant differences were shown in the VAS (p=.051) or the DASH (p=.076) test.
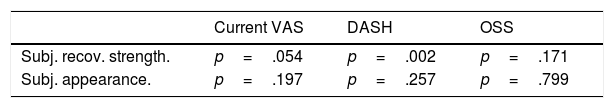
Recovery of subjective strength and subjective appearance was analysed in relation to the functional tests (Table 1); statistically significant differences were only observed between the subjective recovery of strength scores on the DASH (p=.002).
The correlation between the degree of radiological reduction and the subjective appearance of reduction was analysed and there were no statistical differences (p=.582).
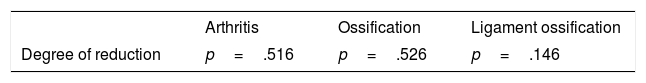
This degree of reduction correlated in turn with the appearance of arthritis, osteolysis and ligamentous ossification; no statistically significant results were shown (Table 2).
DiscussionThis study shows the retrospective outcomes of patients operated for chronic type III AC injuries. These dislocations constitute around 12% of dislocations around the shoulder1 and the most common mechanism of injury is direct trauma.14 These data are not corroborated in this study, since we found that only 7.4% of the cases were caused via this mechanism. Conservative treatment of type III AC dislocation has good outcomes, little pain, little functional impotence and patients are able to resume their usual activities. In fact, it is the treatment of choice for many experts.15 If, 3–6 weeks from the injury, there is no pain or functional alteration, conservative treatment is complete (type III A). If pain or scapular dysfunction persists, radiographic images in the Alexander (Basamania) view are taken, and if there is overriding of the clavicle on the acromion, it is classified as a type III B and surgery is indicated. This approach might be very useful in future practice, however, since our paper was retrospective and included patients who had been treated before this publication, we have no data on this classification in our series, but this can undoubtedly be considered in future studies.
Conservative treatment and surgical treatment with the modified Phemister technique in these types of dislocations have shown good clinical outcomes.12 However, given that surgery increases the risk of arthritis and does not guarantee better functional outcomes or complete reduction, the authors recommend conservative treatment.
As we are in an occupational accident insurance company system, the outcome in terms of return to work are very important in our environment. All the patients were able to return to work with the one exception that resulted in total permanent disability.
The data presented are similar to those published by Chaudhary et al. who, after performing an arthroscopic reconstruction, presented 2 patients with partial reduction loss and one patient with suture breakage at 6 months’ follow-up, the remainder had satisfactory clinical outcomes.16 Kumar et al., also in a series of 55 patients, had good clinical outcomes, except in 3 patients in the group operated using the Weaver–Dunn technique and one patient in the group operated using the Surgilic stabilisation technique with persistent pain and functional deficit.17 In another study by Wang et al., on a series of 33 patients, all the patients returned to their work or sporting activities at 3.7 months postoperatively.18 Defoort et al., with a series of 16 patients, obtained complete radiological reduction in 10, 5 had stable residual subluxation and only one patient required reoperation.19
Subjective recovery of strength correlated with the subjective perception of elimination of deformity, but this subjective perception of reduction did not correlate with the reduction seen on X-ray, since 4 of the patients (14.3%) did not perceive their joint as reduced, this loss of reduction was not visible on X-rays, these data are similar to those of Defoort et al.19 Maintenance of anatomical reduction does not seem to be a requirement for recovering adequate shoulder strength, data similar to those of Vascellari et al.5 Barth et al., with a series of 140 patients, observed radiological complications in 33% at one year's follow-up, although 91% of the patients returned to work.20 The study by Pavlik et al. showed in a series of 17 patients that 6 had a mild loss of reduction (35.3%) and 2 had partial loss of reduction (11.7%).21 However, there are studies, such as that by Boileau et al., in which none of their 10 patients had loss of reduction.22
We looked for statistically significant differences between recovery of subjective strength and subjective appearance and the results of the functional tests carried out (Table 1). In terms of recovery of subjective strength and VAS, no statistically significant differences were found between the patients who did and those who did not, but these data show a clear tendency for the patients who did to have a lower VAS score than those who did not (p=.054). In other words, the subjective impression of recovery of strength might impact on obtaining lower VAS scores. The DASH values behaved in the same way with better scores for those who subjectively recovered strength, and were statistically significant (p=.002). This behaviour was not seen with the OSS (44,137; 39,778) (p=.171).
The relationship between the functional tests and the existence or otherwise of subjective appearance was analysed (Table 1). In this comparison, no statistically significant differences were seen between the functional tests and subjective appearance, in the VAS (p=.197), the DASH (p=.257) or the OSS (p=.799).
The correlation between subjective appearance and the degree of real reductions yielded no statistically significant values (p=.582), which shows that complete radiological recovery has no effect on the subjective perception of reduction.
No statistically significant differences were observed between the degree of reduction and the onset of arthritis (p=.516), osteolysis (p=.526) and ligament ossification (p=.146). Therefore, we cannot conclude that a lack of reduction affects the onset of these radiological signs, even with a long follow-up period.
Although various reinforcement systems were used, the Arthrex® Dog Bone Button system was used in 30% of the fixations. Faggiani et al. compared the Minar® technique with the Dog Bone Button technique and found that the return to work was better after the Minar technique than the Dog Bone Button system (p<.001), but the Constant scale in follow-up was better in the Dog Bone Button group (p<.05).7
In the data from the functional tests, we found statistically significant differences between the preoperative VAS score (6.89) and the postoperative VAS score (1.79) (p<.001). These data coincide with those of Wang et al. (4.7 and 1.2) in their follow-up of a series of 22 patients.18 The study by Defoort et al. also showed that the VAS in follow-up at 17 months had a mean value of .82 in their series of 16 patients.19 We can only refer to the postoperative DASH value obtained, with 12.939 (±16.851), which are the most functional values the closer we get to zero value (0–100). Some authors23 found statistically significant differences in the pre- and post-operative DASH scores. Defoort et al. took the DASH score when follow-up ended, with a value of 2.29 (range .5–83),19 indicating a better result than ours, although with a follow-up of only 17 months. Vitali et al.24 show DASH results at 15 months’ follow-up with a mean of 37. We can also only refer to the postoperative value obtained from the OSS test, at 42.736 (±7.794), corresponding to satisfactory joint function, scores between 40 and 48 being the best functional results of the scale, which is very similar to the data found by Faggiani et al., whose OSS score was 46.19 (range 42–48). In the study by Kumar et al., the OSS of 28 (±11) was in the Weaver–Dunn group, a statistically lower value than the patients operated using the Surgilic technique (p=.008).17
This study has several limitations: the first is that it is retrospective, which reduces the level of scientific evidence and the number of information biases entered in the data is not inconsiderable. Another limitation is that the study is a series of chronic cases, comparison with acute phase treatment was not possible. The third limitation is the lack of functional tests, since we had no preoperative DASH or OSS values to establish a comparison. The fourth limitation is that the functional test surveys were carried out by telephone, due to the inclusion of information biases. The fifth limitation is the size of the sample presented in the study, only 28 patients, which provides data that are not sufficiently robust to draw powerful conclusions. Nonetheless, there are several studies with a sample size that is no larger than ours.5,14,16
To conclude, treating type 3 acromioclavicular dislocation by modified Weaver–Dunn technique provides excellent clinical and radiological outcomes with low morbidity. The good clinical outcomes, even in patients that did not achieve optimal radiological outcomes, should be highlighted and the fact that they were maintained over a mean follow-up period of 73 months (6.1 years).
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Data confidentialityThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: López-Alameda S, Fernández-Santás T, García-Villanueva A, Varillas-Delgado D, Garcia de Lucas F. Resultados del tratamiento quirúrgico de las luxaciones acromioclaviculares tipo III mediante técnica de Weaver-Dunn modificada. Rev Esp Cir Ortop Traumatol. 2018;62:93–99.