To evaluate the results obtained with percutaneous or minimally invasive treatment of displaced fractures of the proximal humerus in a series of patients of working age and with good bone quality.
Material and methodsThe retrospective study included 90 subjects treated in our hospital. The fractures were distributed, according to the Neer classification, into 21 fractures in 2 parts, 44 in 3 parts, and 25 in 4 parts. Five of the subjects had an associated joint dislocation. The fractures in 2 and 3 parts were impacted in valgus and some were in varus. All the cases were resolved with percutaneous or minimally invasive surgery by manipulation of the fragments and stabilizing with Kirschner wires and/or cannulated screws.
ResultsThe evaluation was performed using the Constant test, with a mean result of 77. A total of 15 (17%) patients suffered complications, the most frequent being avascular necrosis in 4 patients (4%).
ConclusionWe believe that percutaneous treatment of these fractures young subjects of working age is a reliable treatment method, achieving a 92% return to work in our series and with few complications.
Valorar los resultados obtenidos con el tratamiento percutáneo o mínimamente invasivo de las fracturas desplazadas de húmero proximal en una serie de pacientes en edad laboral y buena calidad ósea.
Material y métodosEl estudio retrospectivo incluye 90 sujetos tratados en nuestro hospital. Las fracturas se distribuyeron, según la clasificación de Neer en 21 fracturas en 2 partes, 44 en 3 partes y 25 en 4 partes. En 5 sujetos hubo luxación asociada. Las fracturas en 3 y 4 partes lo fueron impactadas en valgo y algún caso en varo. Todos los casos se resolvieron mediante cirugía percutánea o mínimamente invasiva, por manipulación de los fragmentos y estabilización con agujas de Kirschner y/o tornillos canulados.
ResultadosLa valoración se realizó mediante el test de Constant con un resultado promedio de 77. Sufrieron complicaciones 15 pacientes (17%), siendo la más frecuente la necrosis avascular con 4 pacientes (4%).
ConclusiónCreemos que en sujetos jóvenes y en edad laboral el tratamiento percutáneo de estas fracturas constituye un método de tratamiento fiable, consiguiéndose en nuestra serie un 92% de reincorporaciones laborales y con escasas complicaciones.
Proximal humerus fractures account for 5% of all fractures, and their incidence is expected to increase markedly over the coming decades, as the population ages and osteoporosis become more prevalent.1,2
Most of these fractures are non-displaced or slightly displaced,3 but displaced fractures and the candidates for surgical treatment, such as 3- and 4-part fractures, that, historically, represented only 15% of the total1,4 have reached 51% in recent epidemiological studies with large numbers of cases.5,6 The results obtained depend upon factors such as fracture geometry; the patient's age, bone quality, and functional requirements; the surgical technique used; and a specific rehabilitation program.
Treatment modalities for these fractures include conservative treatment, closed reduction with percutaneous osteosynthesis, open reduction with internal fixation, and hemiarthroplasty.
Open reduction and internal fixation, even using the new implants such as LCP systems, are not showing the convincing results that would enable this procedure to be standardized.7 Moreover, osteoporosis can cause the anchorage of osteosynthesis materials to fail, and there is a greater risk of osteonecrosis of the humeral head.
On the other hand, proper reduction using closed methods and stable percutaneous osteosynthesis would permit early, passive mobility with less compromise of the blood supply to the humeral head.
Given these considerations, we proposed to evaluate the results of proximal humerus fractures at our Centre that were treated by closed reduction using indirect reduction techniques and percutaneous osteosynthesis. As a working hypothesis, our assumption was that, in young patients and those of working age (who have significant functional demands and good bone quality), this treatment would stabilize the fracture well enough to initiate functional recovery early and obtain good final results with few complications.
Material and methodsA retrospective review was completed of the results for 90 displaced fractures of the proximal humerus in patients of working age and treated by closed reduction and percutaneous osteosynthesis at our Centre between 1999 and 2009.
The inclusion criteria were 2-, 3-, and 4-fragment fractures, valgus- or varus-impacted (Fig. 1), with or without associated dislocation, that were treated percutaneously.
Patients underwent the procedures and follow-up after an informed consent was obtained.
Among those evaluated were 57 males (63%) and 29 females (37%), and there were 49 left-sided fractures (55%) and 41 right-sided fractures (45%).
The mean age was 46 years (24–68), and the mean follow-up period was 3.5 years (1–8).
The most common mechanism of injury was a fall on the same level in 40 cases (45%), followed by traffic accident in 29 cases (32%); fall from a height in 18 cases (20%); direct contusion in 2 cases (2%); and, in 1 case (1%), overexertion on lifting a motorcycle from the ground. The mechanism was considered to be high-energy in 47 cases (52%) and low-energy in 43 cases (48%).
To classify the fractures, we followed the classification proposed by Neer.8 Of the fractures documented, 21 were 2-part fractures: 16 of the surgical neck and 5 of the greater tubercle. The 3- and 4-part fractures totalled 69, of which 44 were in 3 parts and 25 in 4 parts. There were 66 valgus-impacted and 3 varus-impacted fractures.
The imaging studies done were simple X-ray in antero-posterior and scapular profile projections. There was a CT scan in all cases and, in the last 4 years, 3D reconstructions.
Surgical intervention was done with the patient in “beach chair” position, with the extremity free, and under image amplification control.
Once the surgical neck fracture was reduced using indirect manoeuvres, 2-part fractures were stabilized using Kirschner wires direct from diaphysis to humeral head or using the Kapandji technique9 via the deltoid V. Fractures of the greater tubercle were stabilized using threaded Kirschner wires or cannulated screws.
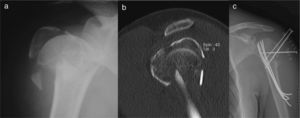
For 3- and 4-part fractures, we used the technique described by Resch et al.10: manipulation and indirect reduction of the fragments through small cutaneous portals using spatulas and hooks (Fig. 2). Once reduction was achieved, the cephalic fragment was stabilized using Kirschner wires direct from diaphysis to head or the Kapandji technique, and the tubercles were stabilized using threaded Kirschner wires or cannulated screws (Fig. 3).
Post-operatively, the extremity was immobilized in a sling for 3 weeks, and an attempt was made to initiate physical therapy in 24–48h through passive and assisted exercises, if stability of the osteosynthesis and the patient's condition allowed this.
The simple Constant scale was used to assess the results.11 Cases were evaluated upon returning to work, and those cases ongoing for more than 4 years were given an appointment for re-evaluation. For measuring strength, we used the multi-function electronic dynamometer linked to computer application Ned/IBV, version 3.0, and we took various measurements until there were 3 consecutive readings with a difference of 20% between values.
Statistical analysis was performed by creating an Excel database and using the SPSS program, v. 13, to analyse the statistical data. Quantitative variables (age, work time lost, initiation of rehabilitation, and final score) and qualitative variables (type of fracture, mechanism of injury, presence of dislocation) were used. The Pearson correlation scale was used for the statistical analysis.
ResultsAssociated injuries were found in 24 patients (27%): of these associated injuries, there were 12 in the same extremity, 3 in the opposite extremity, 6 in the lower extremities, 3 acetabular fractures, 3 chest injuries, 3 facial injuries, and 1 axillary nerve injury.
The mean wait time for surgical intervention was 3.5 days (0–17), those waiting the longest being patients with associated injuries.
Two-part fractures of the surgical neck were stabilized with Kirschner wires direct from diaphysis to humeral head in 3 instances (19%) and using the Kapandji technique, entering via the deltoid V, in 13 instances (81%). Of the greater tubercle fractures, 3 were stabilized with Kirschner wires (60%) and 2 with cannulated screws (40%).
For the 3- and 4-part fractures, the Kapandji method with threaded pins in the greater tubercle was used in 40 cases (57%) and percutaneous Kirschner wires alone in 18 cases (26%). In 6 cases (9%), percutaneous Kirschner wires with cannulated screws in the greater tubercle were used and, in 5 cases (7%), only the Kapandji method was used.
The mean time to initiation of rehabilitation was 17 days (1–60). Of the 90 cases, 40 began physical therapy within the first week; 10 between the first and second week; 12 between the second and third week; 15 between the third and fourth week; and 13 after more than 4 weeks.
The mean length of hospital stay was 14 days (2–90). The highest values for initiation of rehabilitation and length of hospital stay correspond to those cases with associated injuries.
The wires were removed at an average of 14 weeks (4–156), and in 3 patients the materials were not removed.
There were complications in 15 patients (17%): 4 cases of avascular necrosis, confirmed on MRI; 3 malunions due to poor positioning of a fracture fragment; 3 cases of wire migration; 3 cases of adhesive capsulitis; 1 case of incomplete healing; and 1 case of iatrogenic radial nerve injury.
Of the cases of avascular necrosis, which occurred in 4% of all cases, 1 was in a 3-part fracture (2.2%) and 3 were in a 4-part fracture (12%). If only the 3- and 4-part fractures (69 cases) are considered, the incidence of avascular necrosis rises to 5.7%.
Of the 3 malunions due to poor positioning, 2 involved the greater tubercle and 1 the lesser tubercle, and the incomplete healing involved the surgical neck, with 2/3 of it not healed; all these cases required surgical intervention.
The mean time until patient returned to work was 27 weeks (6 months). There were 16 patients who were delayed 40 weeks or more in returning to work, the causes analysed being associated injuries in 5 cases and complications in 9 cases; in the remaining 2 cases, there was nothing to account for it. If we do not count these cases delayed more than 40 weeks, the mean time until patient returned to work was 22 weeks (5 months).
Eighty-three patients were reinstated in their jobs (92.2%). Forty-three patients went to court for assessment of sequelae (47.7%), with 7 being granted work disability (7.7%).
According to the Constant scale, the mean overall result for all the fractures was 77. For the 2-part fractures it was 76.2; among those, the mean Constant for neck fractures was 77.1 and for greater tubercle fractures 75.4. For 3-part fractures it was 80, and for 4-part fractures it was 75.
Statistical analysis revealed that there was a statistically significant correlation between fracture type and mechanism of injury (χ2P=.020), with 3-part fractures predominating in falls on the same level and 2-part fractures in falls from a height, while 3- and 4-part fractures were equal in traffic accidents.
There was no significant correlation between fracture type and final Constant score, the results being homogeneous with only minor differences.
The correlation of work time lost with final Constant score was statistically significant (Pearson P=.006), the best results corresponding to the least work time lost. There were no significant differences in the correlation between work time lost and fracture type, with more work time lost for 4-part fractures and less for 2-part fractures of the greater tubercle. There were also no significant differences for the correlation between age and type of injury.
The coexistence of glenohumeral dislocation, depending on the type of injury, was statistically significant (χ2P=.001), with dislocation predominantly in 2-part fractures. Coexistence of dislocation with the final result was not significant, nor was initiation of rehabilitation with the final result.
DiscussionIn the literature, there are not many series with proximal humerus fractures in patients under 60 years of age; this explains our interest in reviewing the percutaneous intervention we performed on our patients and comparing the results with other series. Our setting—a work accident insurance company—explains the mean age of 46 years, the predominance of male patients, and the higher energy of the mechanisms of injury. These were patients with good bone quality and, therefore, candidates for percutaneous or minimally invasive intervention.
In valgus-impacted and, less frequently, varus-impacted fractures,12 the cephalic fragment rotates and impacts upon the surgical neck, and one or both tubercles are situated outside their lodging. The greater tubercle maintains its relationship to the rotator cuff, proximally, and to the periosteum, distally, which favours the cephalic fragment returning to its natural lodging, once reduced. These fractures will be difficult to reduce using simple manipulation manoeuvres and will require surgical intervention.
Surgical treatment of displaced proximal humerus fractures can be either a percutaneous or an open surgical procedure. The difficulty lies in setting the limits of the indications for one or the other of these surgeries.
Percutaneous surgery requires (1) careful selection of cases, with conditions such as good bone quality and very little comminution of the tubercles; (2) preservation of the medial cortex with its periosteum; (3) that a stable, closed reduction be achieved; and (4) that the patient be cooperative.1
Another subject of debate is the stability of the osteosynthesis and the characteristics of its mounting. Percutaneous fixation is less stable, obviously, than a plate or an endomedullary nail, but it should not hinder the initiation of early mobility with non-taxing, passive, and assisted exercises, and it should have a good movement arc when active mobility is initiated.
In evaluating and following these cases, we were able to notice that, depending on the fracture line, wires pointed directly at the humeral head follow a very horizontal trajectory, remaining in the lowest portion of the head far away from the calcar support area; thus, they fail to provide adequate stability, which favours valgus tilt of the fracture again.
For this reason, we mounted the Kirschner wires in the shape of a palm tree per the Kapandji technique, which increases stability of the cephalic fragment and corrects the longitudinal (varus–valgus) alignment. The tubercles were stabilized using threaded Kirschner wires, which offer stronger fixation and carry less risk of migration than plain wires; they are also easier to remove than the screws (Fig. 4).
The cutting-edge discussion is centred on 4-part fractures, for which some authors recommend an open surgical procedure while others advocate percutaneous intervention—and results are good, even with severe lateral displacement.13
While some authors consider open surgery with plating to be superior to a percutaneous procedure, it is possible, with proper selection of cases and meticulous surgical technique, to obtain good results with few complications.
Resch recommends open surgery when there is marked lateral displacement.14 Other authors recommend arthroplasty, in patients 50–80 years of age, for fractures of the cephalic cap that are displaced or have associated dislocation.13,15
In young patients, percutaneous intervention enables the humeral head to be preserved, with good results, as Resch reports.16
We believe that the choice between percutaneous surgery and open surgery depends on how good a reduction can be achieved with a closed procedure. Percutaneous synthesis should not be permitted over a poor reduction—in those cases, open surgery should be chosen.
In our review of 90 cases with a mean age of 46 years, we obtained a Constant score of 77—close to the scores obtained by various authors who reported that the younger the patient, the better the results.10,16–20
The mean time until patient returned to work was 27 weeks (6 months); without taking into account those cases with associated injuries or complications, however, the actual healing time for these fractures was 5 months.
With regard to complications (17%), we make reference to 2 cases of secondary displacement that required further surgery, also percutaneous; 3 cases of wire migration (described by some authors1,18); and a screw coming loose, removal of which was not required (Fig. 5). These migrations and displacements may be related to different variables, such as wire diameter, the length of the threaded portion, the layout of the wiring on the humeral head (including its orientation, its distribution on the head, and the number of wires), or a combination of these variables.1 The palm-tree-like wiring lends support across the entire surface of the head, which makes it far less likely to collapse.
Robinson21 attributes this to the loss of metaphyseal bone substance and recommends open reduction and filling with a bone substitute.
Avascular necrosis—another complication caused by a lack of blood supply in a bony segment—appears between the first and second year and typically starts in the upper outer quadrant of the humeral head, where the mechanical demands are greater (Fig. 6).22
Authors are in agreement that open surgery—and extensive exposures, in particular—promotes it15,22,23 because this destroys the capsular and periosteal bridges and the musculo-tendinous insertions that irrigate the head. The incidence reaches 13–34%. With regard to its prevention, reference is made in the literature to the importance of preserving the medial periosteum and the vessels that run in this area.3,5,15,23,24
Thus, marked displacement of the internal cortex of the diaphysis indicates disruption of the periosteum and its vascular network, with increased risk of necrosis. Preservation of the periosteum will also facilitate manipulation and reduction of the cephalic fragment by serving as a hinge, which enables the fragment to be rotated back to its original position, thereby preventing lateral displacement.14
Percutaneous access carries a lower risk of necrosis (3–14%).23 Therefore, we propose percutaneous or minimally invasive intervention for fractures in young patients, where indicated. In the literature, its incidence varies from 3% to 14% in 3-part fractures and from 13% to 34% in 4-part fractures.9,10,16–20,25
CT and 3D may help to determine the prognosis.24 In our review, we arrived at the diagnosis for these cases after clinical and X-ray suspicion was confirmed on MRI. The incidence of necrosis was 2.2% for 3-part fractures and 12% for 4-part fractures, and it was not seen in 2-part fractures, which would mean a total of 69 fractures (5.7%). These figures may be low because of the strict selection of cases and meticulous surgical technique, which prevents injury to the delicate blood supply.
We had 3 malunions (3%), compared to 11.4% cited in the literature.13 We had no calcifications or infections; it should be pointed out that, in the literature, the incidence of infections is very low, these being, typically, superficial, circumscribed infections at points insertion for the Kirschner wires.1,26
The statistical analysis shows the correlation between mechanism of injury and fracture type. In falls on the same level, 3-part fractures predominated; in falls from a height, 2-part fractures predominated; and in traffic accidents, there were an equal number of 3- and 4-part fractures. There is a correlation between work time lost and the Constant score: the less work time lost, the better the results. The most work time lost corresponded to 4-part fractures and the least to 2-part fractures of the greater tubercle. Coexisting dislocation did not impact the final result, nor did the point in time at which physical therapy was initiated.
ConclusionsThe results obtained in this study suggest that closed reduction and percutaneous osteosynthesis for displaced fractures of the proximal humerus in this particular population (young people of working age) constitute a reliable treatment method; in our series, there were few complications, and 92% of our patients was reinstated in their jobs.
Although this technique may appear to be simple, it is difficult and demanding, requiring that special care be taken in choosing the indications and that the surgeon performing it has sound knowledge of the technical considerations.27
Evidence levelEvidence Level IV.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Montiel-Giménez A, et al. Resultados del tratamiento percutáneo de las fracturas proximales del húmero en pacientes jóvenes en edad laboral. Rev esp cir ortop traumatol. 2011;55(6):446–453.