Ankle fractures involving a posterior malleolar fragment are associated with worse clinical outcomes. The standard indication for its fixation is a displaced fragment that involves more than 25% of the distal articular tibia. The method of reduction and fixation of these fractures has not received much attention. The purpose of this paper is to describe the surgical technique and clinical results.
Material and methodsOver a 6year period 10 patients with an ankle fracture involving more than 25% posterior malleolus were admitted for surgery, which was performed by the first author. Postoperative management and complications were recorded, reduction accuracy evaluated in the first postoperative radiograph, and functional outcomes were measured using the American Orthopaedic Foot and Ankle Society (AOFAS) hind foot-ankle score and the modified Weber protocol. The surgical technique is described.
ResultsA total of 10 patients were included in the study; and the overall mean age was 53.8 (range: 19–82) years. With regard to complications, none of the 10 patients had any postoperative complication. No cases of reflex sympathetic dystrophy syndrome, superficial infection, iatrogenic lesion of the sural nerve or failure of internal fixation were recorded. One of them had screw and plate removal surgery. Clinical results were good; 9 patients regained their pre-injury activity level, with excellent or good results in both AOFAS and modified Weber protocol.
DiscussionGiven that posterior malleolus fractures are usually posterolateral, this approach allows perfect visualization of the fracture, articular anatomical reduction, and strong fixation. Clinical results obtained were at least equal to other case series published.
Las fracturas de tobillo que incluyen un fragmento posterior se asocian a un peor resultado clínico. Es comúnmente aceptada la indicación de reducción y síntesis del maléolo posterior cuando incluye más de un 25% de la línea articular en proyección lateral. El método de fijación de estas fracturas tiene poca repercusión en la literatura. El objetivo de este trabajo, es describir la técnica quirúrgica y los resultados clínicos obtenidos.
Material y métodosDurante un período de 6 años, 10 pacientes han sido intervenidos por el primer autor. Todos ellos presentaban fracturas que incluían un fragmento posterior mayor de un 25%. Se tomaron datos de la clasificación de la fractura, del manejo postoperatorio, calidad de la reducción postoperatoria en la radiología postoperatoria, así como de cualquier complicación postoperatoria. Todos los pacientes completaron 2 cuestionarios de valoración clínica: American Orthopaedic Foot and Ankle Society (AOFAS) y Weber modificado. Se describe en detalle el abordaje posterolateral del maleolo posterior.
ResultadosDiez pacientes con edades comprendidas entre 19 y 82 años fueron tratados con esta técnica. Todas las fracturas se redujeron anatómicamente. Los resultados son buenos, 9 pacientes obtuvieron un resultado excelente o bueno en las escalas de AOFAS y Weber modificada. No hubo pérdidas de reducción, infección, síndrome de distrofia simpático refleja o lesión iatrogénica del nervio sural. Una paciente precisó de la retirada del material de osteosíntesis por molestias de este. Todas las fracturas consolidaron.
DiscusiónDado que la fractura del maléolo posterior es casi siempre posterolateral, el abordaje descrito permite una excelente visualización de la fractura, lo que permite su reducción anatómica y síntesis con tornillos posteroanteriores. Los resultados obtenidos son al menos equivalentes a otras series clínicas.
Ankle fractures involving a posterior fragment have a worse clinical outcome and an increased risk of degenerative changes.1–7 The indication of reduction and the synthesis of the posterior malleolus are commonly accepted1,3,5,8–10 when it includes more than 25% of the joint in a lateral projection. The smaller fragments are not fixed, since, theoretically, they do not affect the biomechanical action of the joint. This posterior fragment is reduced by ligamentotaxis when the lateral malleolus is reduced, due to the traction exerted by the posterior inferior tibiofibular ligament (PITFL).11 At this time, if indicated, this fragment may be fixed with a screw inserted in an anterior to posterior direction, which could lead to an imperfect fixation,12 or else through a posterolateral approach.10,11
The method of reduction and fixation of fractures has been described in the literature, but has not received much attention and there are no clear treatment bases.13. The objective of this work is to analyse the proposed posterolateral approach and evaluate its effectiveness in the osteosynthesis of the posterior malleolus through the clinical and radiological assessment of a series of patients.
Material and methodOver a period of 6years, between January 2006 and June 2010, 10 patients diagnosed with trimalleolar fracture were operated on by the first author. All suffered ankle fractures with a posterior malleolar fragment representing more than 25% of the joint line.
Data collected during postoperative management included complications, quality of articular surface reduction and functional results assessed using the scale of the American Orthopaedic Foot and Ankle Society14 (AOFAS) and the modified Weber protocol.1,15,16
The AOFAS scale classifies the functional result into 4 categories according to a score out of a maximum of 100 (excellent: >92; good: 87–91; average: 65–86, and poor: <65). The modified Weber protocol evaluates subjective outcomes (pain and occupational or recreational activity), objective results (ankle mobility and walking skills) and radiographic changes, with a maximum score of 20. The final result is obtained by adding the scores for each category: 5 points: excellent; 6 points: good; 7 points: regular, and over 7 points: poor.
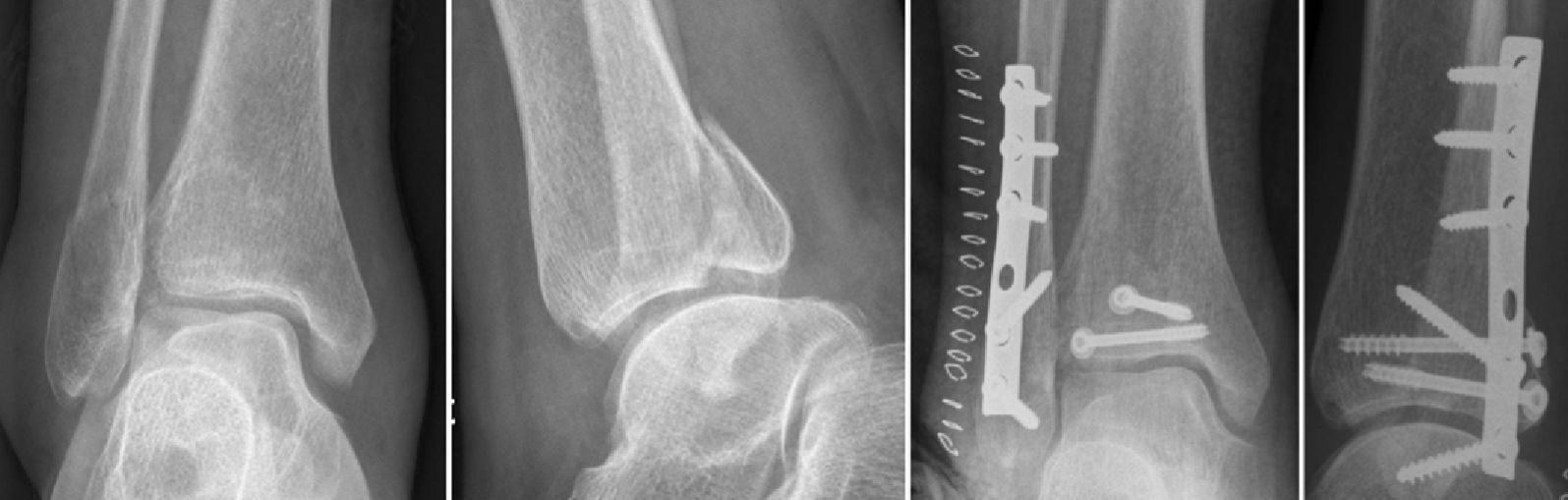
Radiographically, fractures were classified according to the Danis–Weber classification.17 The quality of articular surface reduction was assessed in the first postoperative radiograph; a displacement of the posterior fragment under 2mm was recorded as an anatomical reduction. We also noted the presence or absence of degenerative changes in the ankle joint.
Surgical techniqueSurgery was usually performed in the prone position, although patients could lie on their sides if the medial malleolus was not fractured. In the case of elderly patients who could not tolerate surgery in the prone position, they started surgery in a lateral position and subsequently the brackets were removed and they were changed to the supine position for the synthesis of the medial malleolus. The foot was left hanging at the end of the table in order to allow dorsiflexion.
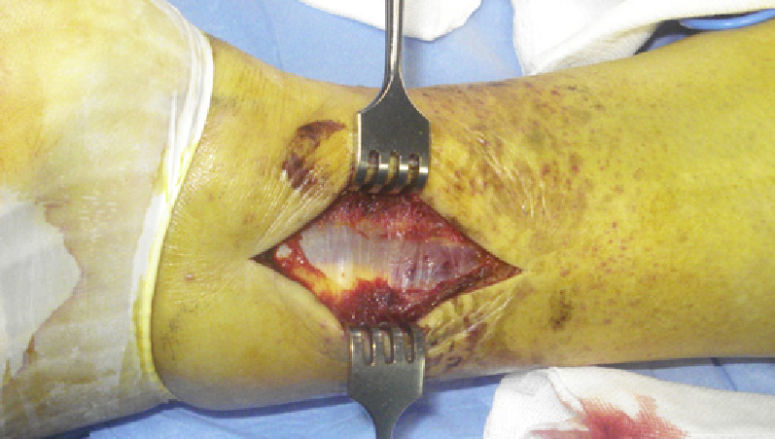
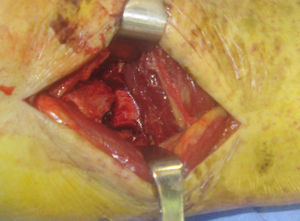
The skin incision was made between the lateral edge of the Achilles tendon and the fibula (Fig. 1). Dissection in the subcutaneous plane was performed with great care in order to respect the sural nerve, which has a variable anatomy.18,19
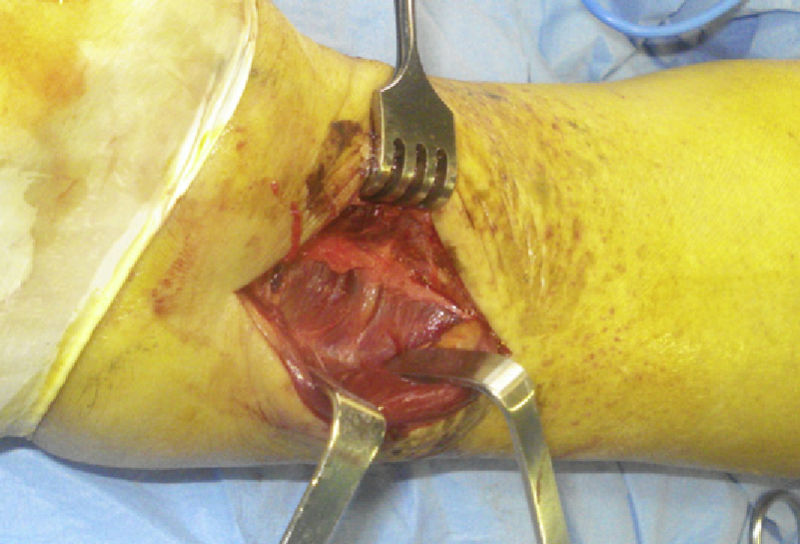
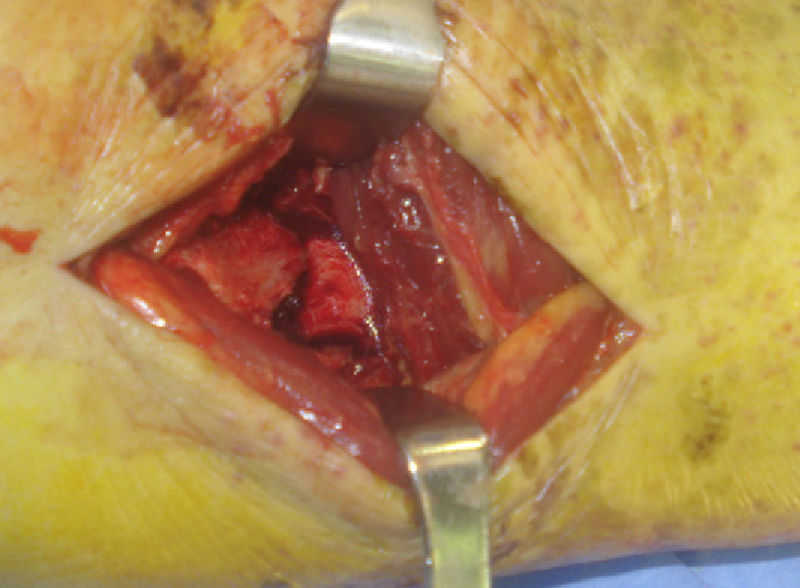
The peroneal fascia (Fig. 2) was opened longitudinally, exposing both tendons. These were separated laterally in order to allow access to the fascia of the flexor hallucis longus (Fig. 3), which was also displaced longitudinally in order to subsequently lift the muscle from the interosseous membrane and the tibia distally from the external side. Special care was employed in the management of the peroneal artery and its side branches, especially the transverse communicating branch. At this point, it was possible to identify the PITFL, which was usually intact and should be respected.
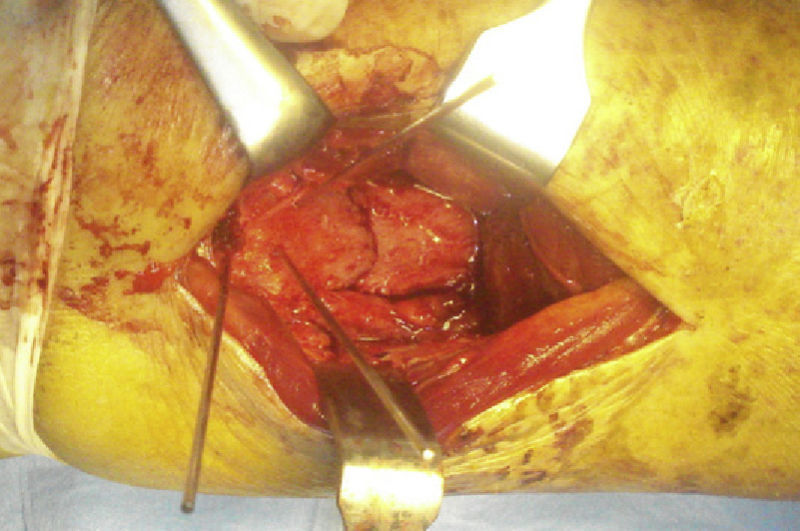
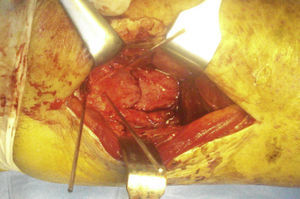
The fracture was traced using the periostotome (Fig. 4). The posterior malleolus was usually displaced laterally and proximally. It is generally useful to set the posterior malleolus before the fibula, as this enables greater mobilization for its reduction and, therefore, fibular osteosynthesis does not preclude verification of a correct joint reduction with fluoroscopy, as would be the case if the plate was placed laterally on the fibula first.
After reduction, the fracture was secured with Kirschner wires (Fig. 5). Reduction was verified with fluoroscopy and the fragment was fixed with 2 cancellous, partially threaded screws, in a posterior to anterior and slightly lateral to medial position, perpendicular to the fracture line. In case of osteoporotic bones, osteosynthesis could be supplemented with non-sliding plates.
Once the posterior fragment was secured, the fibular fracture was exposed through the same incision, either medially or laterally to the peroneal tendons, following the fracture line. They were generally displaced medially to obtain good exposure of distal fractures and to allow placement of lateral or posterolateral plates.
The fixation of the medial malleolus was more complicated in the prone position, but could be performed correctly when the knee was flexed and rotated internally or else bent at 110°. Closure was performed in the usual manner.
ResultsA total of 10 patients were included in the study. All were female, with a mean age of 53.8years (range: 19–82years). In total, 7 of these fractures were classified as type B and 3 as type C of the Danis–Weber classification. In 9 cases, the posterior fragment was fixed with 2 screws and in 1 case with a non-sliding plate.
Postoperative management consisted in immobilization via a cast for 3weeks (mean: 3.2; range: 2–8weeks) and load discharge for 6weeks (mean: 6.3; range: 6–8weeks).
In relation to possible complications, none of our patients presented any postoperative complications (reflex sympathetic dystrophy syndrome, superficial or deep infection, iatrogenic injury of the sural nerve or loss of reduction). One patient required removal of the osteosynthesis material due to discomfort.
The clinical and radiological evaluation was performed at the end of the follow-up period (mean: 3.7years of evolution; range: 1–6years). At this point there were no signs of arthritis on plain radiographs, with all patients presenting radiographically normal joints. Clinical results showed an excellent or good result on the AOFAS scale in 9 out of 10 patients and an excellent or good result in the modified Weber scale in 9 out of 10 patients.
DiscussionAnkle fractures including a posterior fragment have a worse prognosis than bimalleolar fractures.1–7 Larger fragments imply a worse clinical outcome than smaller ones, but the quality of the reduction also influences the final outcome, with better results being obtained if a good reduction is achieved, regardless of size.1,12 However, while there is consensus in the literature on this fact, other aspects remain to be clarified. In a recent review of published literature, van den Bekerom13 emphasized the importance of computed tomography (CT) for an accurate measurement of fragment size20 and surgical planning. Moreover, he noted that joint stability was provided by the medial and lateral stabilizers, rather than the articular surface.8,9
The posterolateral approach offers numerous advantages, such as a single incision to approach both fractures, in the fibula and tibia, the possibility of a performing a direct and anatomical reduction (Fig. 6) and increased coverage of soft-tissues. When clinical outcomes are worse in these fractures it becomes necessary to perfectly reduce both the medial and lateral malleoli, as well as the posterior articular surface and the syndesmosis.
The intra-articular component may be one of the factors worsening the prognosis, even when the fragment size is less than 25%. Therefore, the joint surface should be reduced anatomically, following the basic principles of joint fracture treatment. The posterior malleolus is usually displaced proximally and laterally21 and the periosteum and callus may be interposed in the fracture, so indirect reduction is complicated. In his study, Huber22 demonstrated that the anatomical reduction of the joint surface is easier to achieve through a direct approach than through an indirect reduction and anteroposterior fixation. Anteroposterior fixation with partially threaded screws may be defective due to the passage of windings through the fracture site which would prevent compression of the fracture.12 This approach enables a more stable osteosynthesis because the screw is inserted in a posterior to anterior direction. In addition, it also enables osteosynthesis to be supported with non-sliding plates.
Joint stability is secured with a perfect reduction and fixation of the medial and lateral malleoli, rather than reduction of the posterior fragment, as demonstrated by Raasch8 and Fitzpatrick et al.9 The same approach enables fixation of both the posterior fragment and the fibula. Non-sliding plates in the fibula offer certain advantages over the lateral plate, such as stronger fixation,23 less need for removal of material and less wound dehiscence.24 However, they also have some disadvantages, mainly fibular tendinopathy,25 which is more frequent when the plate is placed in a very distal position.
Syndesmosis lesions are classically associated with type C fractures, although they may occur in other types of fractures where this fragment represents an avulsion of the posterior syndesmosis. In syndesmosis injuries, a residual displacement of the distal fibula over 2mm entails worse results,26 so it should be reduced perfectly. These lesions are commonly treated through trans-syndesmotic fixation, which has several disadvantages, including a relatively high rate of incorrect reductions assessed by CT,27 the need for a second operation for removal, breakage of the screw or tibiofibular synostosis.28 However, in selected patients, stability of the syndesmosis can also be achieved by fixing the posterior fragment. This procedure has been proven to provide a biomechanically stronger fixation,29 at least equivalent to syndesmotic screws regarding functional outcome.30
One of the complications inherent to the posterolateral approach is sural nerve injury. Nevertheless, this complication was not observed in our series.
Despite being a short series, the clinical results obtained both clinically and radiologically were at least equal to those of other series. The posterolateral approach enabled us to achieve an anatomical reduction of the joint surface with stable fixation, good coverage of soft tissues and anatomical reduction of the syndesmosis. This could improve the functional outcome for patients suffering similar fractures.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Mingo-Robinet J, et al. El abordaje posterolateral en las fracturas trimaleolares de tobillo. Técnica quirúrgica. Rev Esp Cir Ortop Traumatol. 2012;56:313–8.