To describe the orthogeriatric activity in the elderly with hip fractures in the Hospital Mancha Centro, based on the recommendations of the main guidelines.
Material and methodObservational prospective study, comprising all patients over 65 years of age admitted to the Traumatology Unit with a hip fracture between April 2015 and December 2015. Patients were admitted under the care of the Traumatology Unit with cross-consultation carried out with the Geriatrics Department, which then carried out a pre-operative geriatric assessment and the post-operative follow-ups.
ResultsThe mean pre-surgery waiting time was 48h and the overall time in hospital was 10.3±8.2 days. Patients who suffered from delirium (42.1%) did not improve as well, and were referred to nursing homes. Blood transfusions were received by 54.7% of the patients, despite 53.5% of them having received intravenous and/or oral iron after the surgery. Treatment with calcium and vitamin D was prescribed in 79% of the patients on discharge. The Rehabilitation Unit assessed 36% of the patients, with 4.8% fully, and 16.7% partially recovering their prior functional status. Upon discharge, 55% of the patients returned to their homes, and 22% were referred to short-term assisted living facilities.
DiscussionThis article describes how the main clinical problems are handled in the elderly with hip fractures in our hospital, based on recommendations of the main guidelines and publications.
ConclusionsOur hospital follows the recommended guidelines. Aspects for improvement include the management of anaemia during admission and rehabilitation.
Describir la actividad ortogeriátrica en ancianos con fractura de cadera en el Hospital Mancha Centro basándonos en las recomendaciones de las principales guías clínicas.
Material y métodoEstudio prospectivo observacional. Se incluyen todos los pacientes mayores de 65 años ingresados en traumatología con fractura de cadera desde abril de 2015 a diciembre de 2015. El paciente ingresa a cargo de traumatología y se interconsulta a geriatría, que realiza una valoración geriátrica preoperatoria y un seguimiento postoperatorio.
ResultadosLa estancia media prequirúrgica fue de 48h y la estancia media global de 10,3±8,2 días. Los pacientes que sufrieron delirium (42,1%) evolucionaron peor y se derivaron más a residencias. Se transfundieron el 54,7% de los pacientes a pesar de que el 53,5% recibieron hierro intravenoso y/u oral en el postoperatorio. Al alta se pautó calcio y vitamina D al 79% de los pacientes. Fueron valorados por rehabilitación el 36% de los pacientes, recuperando su situación funcional previa el 4,8% y parcialmente el 16,7%. Al alta, un 55% de los pacientes volvieron a su domicilio y un 22% fueron derivados a estancias temporales.
DiscusiónEn este artículo se detalla el manejo de los principales problemas clínicos en nuestro hospital en ancianos con fractura de cadera basándonos en las recomendaciones de las principales guías y resultados de publicaciones al respecto.
ConclusionesEn nuestro hospital se siguen las recomendaciones de las guías. Aspectos a mejorar son el manejo de la anaemia durante el ingreso y la rehabilitación.
Hip fracture (HF) is a serious problem in medical, healthcare, economic and social terms.
More than 85% of HF occur in patients older than 65 years old.1 In Spain from 50,000 to 60,000 HF occur per year. This incidence is rising and it is estimated that it will have doubled by 2050.2 In Castile-La Mancha the rate of incidence adjusted for both sexes stands at 734 per 100,000 inhabitants.3
The direct costs of treating each HF in Spain vary from 3000 to 5200 Euros, depending on hospital and autonomous region, and overall costs amount to 300–860 million Euros, without counting additional indirect expenses such as carers, old people's homes and rehabilitation.3
All of the guides analysed recommend that the geriatric and orthopaedic departments cooperate in treating the elderly with HF.3–7 This includes the acute phase during hospitalisation, rehabilitation, convalescence and support.
The most widespread model is currently to have a Consultant Geriatrician for hospitalised patients in orthopaedic beds. This co-working strategy has been shown to reduce hospital stay prior to surgery, reduce complications, improve functional results, reducing mortality and the duration of hospitalisation as well as treatment costs.8–11
A programme was established in our centre in 2008 for internal consultation with the Geriatric Department for all HF patients over the age of 65 years old. This coincided with the hospital contracting geriatricians.
In a study published in Spain, Sáez López et al. and the Orthogeriatric Working Group of Castile y León describe orthogeriatric working in the public hospitals of Castile y León, comparing it with the guides on clinical practice and other publications in this field. They conclude that orthogeriatric cooperation is a habitual practice, as is following the recommendations of clinical practice guides for treating HF in geriatric patients. They found that clinical care and rehabilitation were areas that should be improved.12
This work studies how the most common clinical problems are managed in elderly HF patients who are admitted to the Orthopaedic Department of our hospital in cooperation with the Geriatric Department. It is based on the recommendations of the main clinical practice guides3–7 and the results published in the relevant literature.
Material and methodsPatients and designThis study is descriptive and observational. All of the HF patients over the age of 65 years old admitted to the orthopaedic department and also seen by the geriatric department were included prospectively and consecutively, from April to December 2015.
The Mancha Centro Hospital is a general hospital located in Alcázar de San Juan, Ciudad Real. It has a total of 343 hospital beds for a catchment area of 125,610 inhabitants who live in 21 municipalities in the provinces of Ciudad Real, Cuenca and Toledo. This area contains 18 old people's homes.
Patients are admitted to the Orthopaedic Department from the A&E Department. Once in the ward they are evaluated by geriatricians in interconsultation. The geriatrician evaluates them and prepares a plan for care on admission, as well as for postoperative care after surgery. The orthopaedic surgeon and anaesthetist decide when to operate, depending on the availability of the emergency operating theatre and the clinical state of the patient, but always as soon as possible. Partial prostheses have been used for intracapsular fractures, together with intramedullary osteosynthesis or percutaneous extramedullary osteosynthesis for pertrochantheric fractures and intramedullary osteosynthesis for subtrochanteric ones.13 Evaluation for rehabilitation is decided on by the orthopaedic surgeon or geriatrician through interconsultation. When social resources are required, such as assisted homes or home-help, social workers are requested to intervene.
Description of variablesThe following data are recorded at admission: date of birth, sex, date and time of the first evaluation by the orthopaedic surgeon, previous Barthel score, Charlson score, history of cognitive deterioration, nutritional parameters (albumin, total protein, total cholesterol and number of lymphocytes), malnutrition according to the SENPE14 criteria, vitamin D level, number of drugs taken at admission and whether they include any psychiatric medication, previous ingestion of vitamin D, calcium or bisphosphonates, and fracture type.
The following data are recorded at discharge: date and time of the operation, delay (more than 48h after the first examination by the orthopaedic surgeon), cause of delay, type of anaesthesia, date and reason for discharge, medical complications during hospitalisation, whether treatment for osteoporosis is prescribed (calcium, vitamin D or bisphosphonates), whether the patient received iron treatment or a transfusion, if they received dietary supplements, if they were examined by the rehabilitation department, type of osteosynthesis used for the fracture, complications connected with surgery and destination on discharge (home, home with assistance, previously institutionalised, temporary stay).
We evaluate the actions taken to care for elderly HF patients based on the recommendations of the main clinical practice guides for this.3–7
Statistical analysisQualitative variables are described using absolute and relative frequencies, while quantitative ones are described using central tendency measures (average or mean) together with dispersion measurements (standard deviation or interquartile range) depending on whether variables are distributed normally or not. Comparative analysis is performed using Chi-squared tests (or Fisher's exact test when appropriate) for qualitative variables, and comparisons between groups are made using the Student's t test for quantitative variables. A level of significance of 0.05 was selected. All calculations were carried out using the SPSS v18 program.
Results773 patients were admitted to the orthopaedic surgery department during the period studied, of which 137 were HF cases, representing 18% of total admissions.
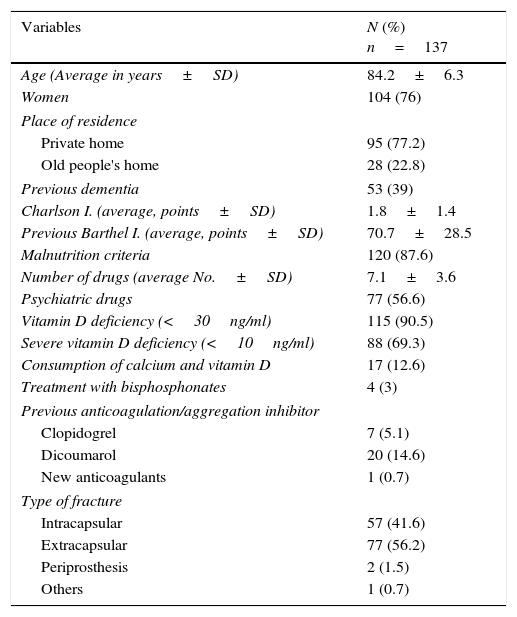
Table 1 shows the main characteristics of the patients at the moment of admissions. They had a high average age (84.2±6.3 years old) and were mainly women (76%). They had a mild level of functional dependency on the Barthel index and low comorbidity measured using Charlson's scale. A high proportion of the patients presented cognitive deterioration in their medical history. Their consumption of several types of medication stands out (more than 7 drugs on average per patient), and 56.6% of the patients were taking psychiatric medication. Those patients who were taking more than 6 drugs prior to admission were found to progress significantly less favourably (dying or being transferred to another department due to complications) (27.4% vs. 11.9%, P=.028). More than 90% of the patients presented vitamin D deficit, and less than 20% received calcium and vitamin D treatment. More than 20% were taking anticoagulant pharmaceuticals and aggregation inhibitors, while the analytical data of more than 80% showed signs of malnutrition according to the standard SENPE14 criteria. The majority of our patients originate in the community. Extracapsular fractures were the most frequent type (56.2%) and of these, pertrochanteric fractures were the most common (46% of the total).
The main patient characteristics at admission.
| Variables | N (%) n=137 |
|---|---|
| Age (Average in years±SD) | 84.2±6.3 |
| Women | 104 (76) |
| Place of residence | |
| Private home | 95 (77.2) |
| Old people's home | 28 (22.8) |
| Previous dementia | 53 (39) |
| Charlson I. (average, points±SD) | 1.8±1.4 |
| Previous Barthel I. (average, points±SD) | 70.7±28.5 |
| Malnutrition criteria | 120 (87.6) |
| Number of drugs (average No.±SD) | 7.1±3.6 |
| Psychiatric drugs | 77 (56.6) |
| Vitamin D deficiency (<30ng/ml) | 115 (90.5) |
| Severe vitamin D deficiency (<10ng/ml) | 88 (69.3) |
| Consumption of calcium and vitamin D | 17 (12.6) |
| Treatment with bisphosphonates | 4 (3) |
| Previous anticoagulation/aggregation inhibitor | |
| Clopidogrel | 7 (5.1) |
| Dicoumarol | 20 (14.6) |
| New anticoagulants | 1 (0.7) |
| Type of fracture | |
| Intracapsular | 57 (41.6) |
| Extracapsular | 77 (56.2) |
| Periprosthesis | 2 (1.5) |
| Others | 1 (0.7) |
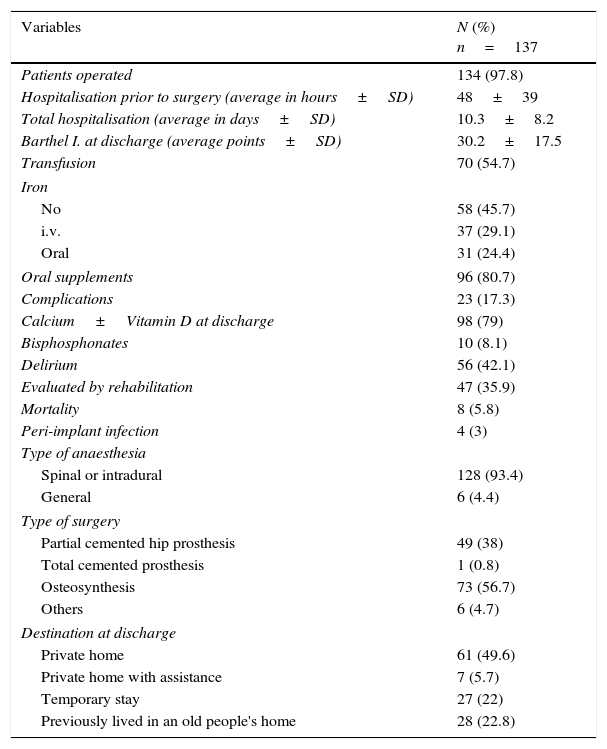
Table 2 shows the results of the variables recorded at discharge. The majority of patients were operated in the first 48h (64.9%) after being examined by the orthopaedic surgeon, and the average hospitalisation before surgery was 48±39h. The most frequent cause of delayed surgery (>48h) was the consumption of oral anticoagulants (3.6±1.2 days) and secondly taking Clopidogrel (5±1.6 days). The patients who underwent longer admission prior to surgery (>48h) presented more medical complications that led to their transfer to another department, although this difference was not significant (21.3% vs 14.3%, P=.288). The type of anaesthesia used the most widely was spinal or intradural anaesthesia in 93.4% of patients, and no epidural technique was used. 53.5% of the patients received i.v. or oral iron after the operation, and even so more than 50% of them received a transfusion. The average total duration of admission was 10.3±8.2 days. 17.3% of the patients operated were transferred to another department due to medical complications. Of these, the most frequent complications were pneumonia (21.4%), heart failure (17.3%) and respiratory failure (8.9%). 42.1% suffered delirium or confusional syndrome, above all among patients with cognitive deterioration (64.7%) with which the association was significant (P<.001). Delirium was found to be more strongly associated with a worse functional situation on admission (Barthel < 60) compared to those patients with a better functional situation (58.5% vs 33.3%; P=.007). Delirium was significantly associated with increased patient transfer to temporary stay facilities (P=.04). It was also associated (although not significantly so) with more medical complications that led to transfer to another department, a longer period of hospitalisation and greater functional deterioration at discharge. Intrahospital mortality was 5.8%. The causes of death were: heart failure (n=4), kidney failure (n=1), pneumonia (n=1), bronchoaspiration (n=1) and diverticulitis (n=1). More than 80% of the patients were given dietary supplements during their stay, and the majority were prescribed calcium and vitamin D at discharge. Fewer than 40% of the patients were evaluated by the rehabilitation department. Only 4.8% of patients regained their previous functional situation after discharge (5 points less than their previous Barthel score), while 16.7% did so partially (20 points less than their Barthel score at admission). 55% of the patients returned to their home at discharge, while 22% were sent to a temporary stay facility.
Description of the main orthogeriatric activity variables at discharge.
| Variables | N (%) n=137 |
|---|---|
| Patients operated | 134 (97.8) |
| Hospitalisation prior to surgery (average in hours±SD) | 48±39 |
| Total hospitalisation (average in days±SD) | 10.3±8.2 |
| Barthel I. at discharge (average points±SD) | 30.2±17.5 |
| Transfusion | 70 (54.7) |
| Iron | |
| No | 58 (45.7) |
| i.v. | 37 (29.1) |
| Oral | 31 (24.4) |
| Oral supplements | 96 (80.7) |
| Complications | 23 (17.3) |
| Calcium±Vitamin D at discharge | 98 (79) |
| Bisphosphonates | 10 (8.1) |
| Delirium | 56 (42.1) |
| Evaluated by rehabilitation | 47 (35.9) |
| Mortality | 8 (5.8) |
| Peri-implant infection | 4 (3) |
| Type of anaesthesia | |
| Spinal or intradural | 128 (93.4) |
| General | 6 (4.4) |
| Type of surgery | |
| Partial cemented hip prosthesis | 49 (38) |
| Total cemented prosthesis | 1 (0.8) |
| Osteosynthesis | 73 (56.7) |
| Others | 6 (4.7) |
| Destination at discharge | |
| Private home | 61 (49.6) |
| Private home with assistance | 7 (5.7) |
| Temporary stay | 27 (22) |
| Previously lived in an old people's home | 28 (22.8) |
The type of osteosynthesis used the most often was intramedullary osteosynthesis (43.5%), followed by cemented partial prosthesis (38%) and percutaneous extramedullary osteosynthesis (13.2%).
Peri-implant infections occurred in 3% of the patients (2 partial cemented prostheses, one intramedullary pin and one plate). Mortality in patients with a peri-implant infection was 50%.
DiscussionGeneral dataIn line with Ministry of Health and Consumption data, our HF patients had an average age above 80 years old, and they were mainly women.2
A finding that stands out in comparison with other studies is that in spite of the advanced age of the patients and a high proportion of cognitive deterioration, they had low rates of comorbidity and dependency. These data agree with the fact that the majority of the patients here were from the community, while other studies include more patients who were previously institutionalised and therefore more dependent and with greater comorbidity.8,11
The average length of hospitalisation in our study was 10.3 days, which is shorter than the national average, which varies from 12 to 24 days.2
Intrahospital mortality in our hospital among HF elderly patients is 5.8%. This is within the average rage in Spain, which stands at 5% and varies from 2–3% to 7–8%.2
Preoperative careThe time for surgeryAll of the guides recommend prompt surgery, some in the first 24h,4,5 from 24 to 36h3 or at 48h.6 As is the case in a recent study,15 the most frequent cause of delayed surgery in our hospital was that the patient was taking oral anticoagulants and aggregation inhibitors such as Clopidogrel at admission. Even so, the average duration of hospitalisation prior to surgery in our study is 48h. In agreement with other studies,16 patients who were hospitalised for more than 48h prior to surgery went on to suffer more postoperative complications, although the differences were not significant.
Recommendations for anticoagulated patientsWhen patients have been taking vitamin K antagonist oral anticoagulants (VKA) the guides recommend delaying surgery until their INR<1.5 for surgery under general anaesthetic or an INR≤1.3 for neuroaxial anaesthesia.17 The SIGN recommends withdrawing VKA and reversing the anticoagulation with i.v. vitamin K after the diagnosis of the fracture to prevent delaying surgery.4 In patients with high risk of thrombosis (<3 months after a cerebrovascular accidents, valve prosthesis or serious thrombophilia) bridging therapy is recommended using low molecular weight heparin (LMWH).18
When patients are taking one of the new direct action oral anticoagulants (DAOA), and considering that HF surgery is urgent and delayable, surgery should be delayed if possible by at least 24–36h after the administration of the last dose of the same. This is specifically equivalent to 2 half-lives in each case: from the 27h for Rivaroxaban, to the 36h for Apixaban and the 48h for Dabigatran in patients with functioning kidneys. The systematic prophylactic administration of haemostatic drugs is not recommended.19
Recommendations for patients taking aggregation inhibitor drugsAccording to current guides, elderly patients with HF and taking aggregation inhibitor drugs, 100mg/d acetylsalicylic acid (ASA) or 300mg/d triflusal do not contraindicate surgery, while 300mg/d ASA is substituted by 100mg/d and no delay in surgery is required. Clopidogrel will be suspended 3–7 days before surgery, depending on the risk of thrombosis or haemorrhaging. Aggregation inhibitor treatment will be resumed as soon as possible after the operation, once haemostasis has been ensured (6–48h): aspirin can be given 6h after the end of surgery, while Clopidogrel can be given in the first 24h afterwards. ASA and triflusal do not contraindicate neuroaxial anaesthesia. Clopidogrel will be suspended 7 days before surgery, although recent evidence indicates that 5 days may be sufficient. Evaluate the substitution of Clopidogrel with 100mg/d ASA if there are no contraindications.3,20
In our sample patients with Clopidogrel as aggregation inhibitor treatment waited for 5±1.6 days before surgery, which is in line with the recommendations of the guides.
AnaesthesiaWithin neuroaxial anaesthesia, spinal anaesthesia tends to be selected for elderly HF patients. This is associated with a lower rate of mortality 1 month after surgery, and also with fewer cardiovascular complications than is the case with general anaesthesia.21 According to the recommendations of the guides, spinal anaesthesia must be considered for all HF patients unless it is contraindicated.3–5 In our hospital more than 90% of the elderly HF patients are operated with spinal anaesthesia, and only 4.4% are operated under general anaesthetic.
Although spinal haematoma after spinal anaesthesia is a rare complication, antithrombotic drugs may increase the risk of haemorrhage in the spinal canal, so that if this technique is used in patients taking aggregation inhibitor drugs, we will follow the recommendations given in the previous section.
The treatment of habitual clinical problemsDeliriumOne of the most common complications during hospitalisation for HF is the appearance of delirium or acute confusional syndrome, which is associated with a worse prognosis. The guides recommend prevention and early treatment of its causes, together with hydration and suitable oral ingestion and the control of symptoms to reduce its incidence and severity.4,5,22
The incidence of delirium in our hospital was 42.1%, which is a similar value to those published by other authors in our country (34.6–45.2%).10,15 As in other studies, we found that predisposing factors to delirium include cognitive deterioration and a poorer functional situation at admission.23 Delirium is significantly associated with increased transfer to temporary stay facilities. A higher frequency of medical complications is also observed, although this was not significant, as well as longer hospitalisation and greater functional deterioration.
AnaemiaAccording to studies, around 50% of HF patients require a postoperative blood transfusion.24 In our hospital 54.7% of elderly HF patients receive a transfusion after the operation. In accordance with the recommendations of the majority of guide, in our hospital a transfusion is indicated when haemoglobin (Hb) levels are <8g/dl or from 8g/dl to 10g/dl if the patient has cardiorrespiratory or cerebrovascular pathology.4,25
In some studies HF patients benefit from treatment with i.v. iron, reducing the rates of transfusion and postoperative morbimortality.26
In the updated version of the Seville Consensus Document non-anaemic HF patients or those with a subcapital fracture, the preoperative administration of i.v. iron is a grade 2B recommendation (moderate quality evidence). In anaemic HF patients the combined administration of i.v. iron and recombinant human erythroprotein (a dose of 40,000UI) seems more effective in reducing the rate of transfusions than only i.v. iron. Postoperative treatment with i.v. iron is a 2C recommendation (low quality evidence). There is no recommendation to give oral iron in the postoperative period (grade 1B).27 A guide for the clinical management of anaemia in HF patients could be: at admission if Hb<13g/dl and ferritin<100, unless there is a contraindication, administer parenteral 20mg/kg i.v. iron up to a maximum o f 1000mg if it is a carboximaltose or isomaltose iron preparation, as these make it possible to give high doses, and 12mg i.v. calcium folinate plus 1mg intramuscular cyanocobalamin (if levels are low or have not been measured). 200mg of sacarose iron may be given every 48h as an alternative to i.v. iron, as due to its stability it is possible to give high doses, without surpassing 600mg/week.28
We found no differences in our study in the percentage of postoperative transfusions between patients who had received i.v. iron and those who received oral iron or no treatment. This could be explained by the lack of a protocol for managing anaemia in elderly HF patients.
Malnutrition and the use of nutritional supplementsMany authors describe a high prevalence of malnutrition among HF patients, at from 31% to 88%, depending on the criteria used.29,30 Almost all guides recommend the use of nutritional supplements to reduce mortality, the appearance of complications and the average duration of hospitalisation.4–6 In our hospital a very high percentage of elderly HF patients suffer malnutrition on admission (87.6%). More than 80% of patients are prescribed oral nutritional supplements before and after surgery.
PolypharmacyPolypharmacy stands out in our study, and this increases the possibility of interactions between drugs during surgery. Patients who consume more than 6 pharmaceuticals at admission evolve less favourably. Additionally there is high consumption of psychiatric drugs, and this increases the risk of falls and fractures.31
OsteoporosisThe treatment of osteoporosis using calcium and vitamin D with antiresorptive medication is supported by current scientific evidence.32
Data in our study show that only 19.3% of the elderly patients who were admitted to our hospital due to HF had previously been treated for osteoporosis. When patients are discharged they are usually prescribed calcium and vitamin D. The fact that bisphosphonates are rarely prescribed is probably due to the lack in our hospital of a treatment protocol for osteoporosis. There is also a certain reluctance to prescribe bisphosphonates because of their side effects33,34 (maxillary osteonecrosis and atypical fractures), as well as the need to monitor and re-evaluate the patients treated with these drugs.35
RehabilitationAll of the guides underline the importance of rehabilitation to achieve the functional recovery of patients, shortening their hospital stay and preventing medical complications and institutionalisation.3–5
In other studies 73–92.7% of patients treated by the orthopaedic surgery department received rehabilitation in the acute phase of HF, recovering their previous functional situation partially or fully at discharge in 62–74.3% of cases. 22% of patients are discharged to their home, 20% to functional recovery units and 51% to homes or long stay units.8,10,16
The percentage of patients who receive rehabilitation in the acute phase of HF in our hospital is low (36%) in comparison with other hospitals, and only 21.5% of patients recover their previous functional situation partially or completely. This low percentage may be connected with the fact that in our hospital HF is managed as a condition that is basically acute.
One limitation of our study is the lack of standardised protocols in our centre for the treatment of elderly patients with HF. However, in spite of this and according to the data shown, these patients are treated according to the recommendations of the main guides in this field. Another limitation is that patients were not followed-up over time after discharge from hospital, so that we cannot add results on mortality and functioning over the longer term to compare them with other studies. Respecting delay to surgery, organisational factors such as the availability of operating theatres were not recorded. Nevertheless, the average length of stay prior to surgery fits the recommendations of the guides.
ConclusionsThe majority of the elderly patients admitted to our hospital due to HF live in the community and present low levels of comorbidity and dependency. They stand out for a high level of polypharmacy and malnutrition, together with vitamin D deficit. The overall average duration of hospitalisation and stay prior to surgery are relatively short in comparison with other studies in our country. Delirium is common and is associated with worse evolution and a higher likelihood of being discharged to a temporary stay facility. In general the recommendations in guides to clinical practice are followed in the treatment of elderly HF patients. The areas for improvement are the management of anaemia and rehabilitation during admission. Treatment of osteoporosis using bisphosphonates on discharge should be considered. The creation of a protocol should be considered for the management of the main problems which elderly HF patients may present on admission to our hospital, with the aim of improving these deficient areas.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of people and animalsThe authors declare that no experiments took place in human beings or animals for this research.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work governing patient data publication.
Right to privacy and informed consentThe authors declare that no patient data are shown in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the Admissions Department and Archive and Clinical Documentation Unit for their help in undertaking this study.
Please cite this article as: Fernández-Ibáñez JM, Morales-Ballesteros MC, Crespo-Romero E, Gómez-Gómez S, Fraga-Fuentes MD, Cruz-Tejado J, et al. Actividad ortogeriátrica en un hospital general de Castilla-La Mancha. Rev Esp Cir Ortop Traumatol. 2017;61:88–95.