The aim of the present study is to analyze the factors associated with mortality and the capacity to perform daily life activities (DLA) in patients with surgically treated proximal humeral fractures.
MethodsA retrospective study was conducted on 94 patients with a surgically treated proximal humeral fracture, with a mean follow-up of 8 years (2–12 years). A correlation analysis was performed to determine the relationship between the type of fracture, surgical technique, comorbidities and mortality and DLA. The Student's t test was used for statistical analysis.
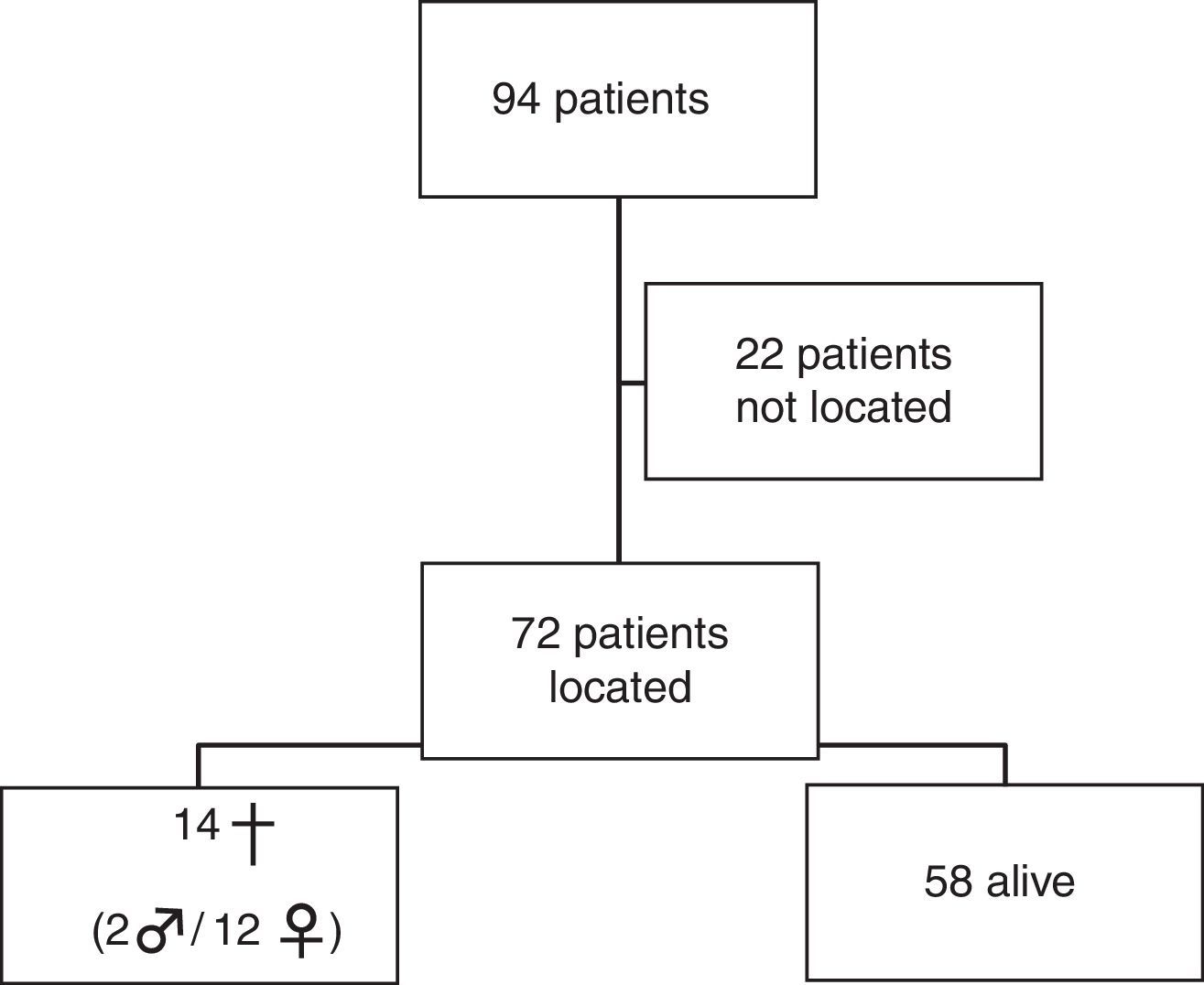
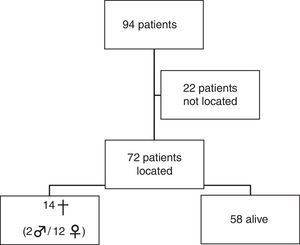
ResultsA total of 72 patients were identified, 18.6% of them died during follow-up, all diagnosed with some comorbidity. There was no correlation between mortality, type of fracture or the technique used.
Most of the patients (85.4%) had comorbidities, and 79.5% were completely independent for DLA. Although there was no relationship with the type of fracture, there was a significant reduction in the performing of DLA in patients treated with hemiarthroplasty, and in patients with neurological disorders.
ConclusionsThere was a mortality of 18.6% among patients with surgically treated proximal humerus fractures.
The majority of surgically treated patients were fully independent for DLA at long-term follow-up.
El objetivo de este estudio es analizar los factores que se correlacionan con la mortalidad y la capacidad para realizar actividades de la vida diaria (AVD) en las fracturas de húmero proximal tratadas quirúrgicamente.
MétodosSe estudiaron retrospectivamente a 94 pacientes con fractura de húmero proximal intervenidas quirúrgicamente con un seguimiento medio de 8 años (2-12 años). De la muestra, se estudió el tipo de fractura, el tratamiento aplicado y sus comorbilidades. Se correlacionan los parámetros con la mortalidad y el nivel de las actividades de la vida diaria.
ResultadosSe localizaron a 72 pacientes, de los cuales el 18,6% habían fallecido. Un 85,4% de los pacientes presentan comorbilidades. El 79,5% de los pacientes eran totalmente independientes para las actividades de la vida diaria. No encontramos correlación entre la mortalidad, el tipo de fractura y el tratamiento aplicado.
No se encontró relación significativa entre las AVD y las comorbilidades con el tipo de fractura, pero sí que se encontró una reducción significativa de la función de las actividades de la vida diaria en pacientes tratados con hemiartroplastia y en pacientes con trastornos neurológicos.
ConclusionesEncontramos una mortalidad del 18,6% en los pacientes con fractura de húmero proximal tratada quirúrgicamente.
La mayoría de los pacientes intervenidos son totalmente independientes para las actividades de la vida diaria, con un seguimiento a largo plazo.
Proximal humerus fractures have increased dramatically in the last 30 years. Not only has the total number of fractures risen, but also the mean age of patients has gone from 73 years in 1970–1978 years in 2002. Even the complexity of the fracture patterns has increased over this period.1,2
Despite the fact that most of these fractures are not displaced and can be treated conservatively, there is no consensus on the best treatment option in displaced proximal humeral fractures. While some authors are in favor of a conservative approach, others recommend surgical treatment.3–9
Most proximal humerus fractures in patients of advanced age can be attributed to osteoporosis. Those who suffer fractures of the proximal humerus most often present subsequent osteoporotic fractures. In spite of this knowledge, scarce attention has been paid to the diagnosis and treatment of the underlying osteoporosis.10–12
Proximal humerus fractures are associated to a higher mortality, especially among males. Nevertheless, very few studies to date have analyzed the mortality and capacity to carry out daily life activities (DLA) among patients suffering proximal humerus fractures and undergoing surgical treatment, compared to those suffering hip fractures.13–23
The objective of this study is to analyze the factors correlating mortality and the capacity to perform DLA among patients with proximal humerus fractures treated surgically.
MethodsWe conducted a retrospective study after prospectively gathering data from 94 patients undergoing surgical treatment of proximal humerus fractures at our center, of which we were only able to locate 72. The sample included 20 males and 74 females, with a mean age of 72 years (range: 50–89 years), of which 17 patients were aged between 50 and 65 years, 35 between 66 and 80 years and 20 between 80 and 89 years. The right shoulder was affected in 56 cases and in the majority of cases (86.5%) it was the dominant arm.
The inclusion criteria considered in this study described patients arriving at our hospital between the years 2000 and 2001, with a diagnosis of proximal humerus fracture, undergoing surgical treatment and aged 50 years or over.
The exclusion criteria included all those patients who attended during the same period due to proximal humerus fractures which were treated conservatively and those aged less than 50 years.
All cases were diagnosed with fracture of the proximal humerus following a radiographic study in 2 projections (AP and profile in the plane of the scapula), as well as a computed tomography (CT) scan for correct classification. Fractures were classified according to the Neer classification,24 resulting in the following distribution: 33 fractures in 2 fragments (17 fractures of the surgical neck, 9 fractures of the anatomical neck, 7 fractures of the greater tuberosity), 44 fractures in 3 fragments (40 fractures of the greater tuberosity, 4 fractures of the lesser tuberosity), 9 fractures in 4 fragments, 2 fracture-dislocations in 2 fragments, 2 fracture-dislocations in 3 fragments and 4 fracture-dislocations in 4 fragments.
The patients studied underwent different surgical treatments depending on the type of fracture, age and criteria of the surgeon. Of these, 40 were intervened through isolated transosseous sutures, 27 through transosseous sutures associated to Ender nails, 3 through placement of angular stability plates, 22 through hemiarthroplasties and 2 through inverted prostheses.
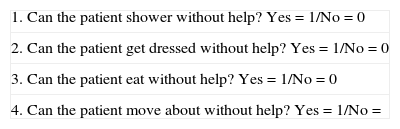
All patients were reviewed in order to obtain data on: (a) mortality, (b) subsequent fractures, (c) the level of satisfaction with the function of the affected shoulder (stratified into 3 categories: very satisfactory, satisfactory and not satisfactory) and d) the level of dependence or independence for DLA (assessed through 4 questions [Table 1] which established whether the patient was capable/incapable of DLA, with this variable being qualitative).
Questionnaire on activities of daily life.
| 1. Can the patient shower without help? Yes=1/No=0 |
| 2. Can the patient get dressed without help? Yes=1/No=0 |
| 3. Can the patient eat without help? Yes=1/No=0 |
| 4. Can the patient move about without help? Yes=1/No= |
If 3 points or >: apt (independent for DLA).
If <3 points: not apt (dependent for DLA).
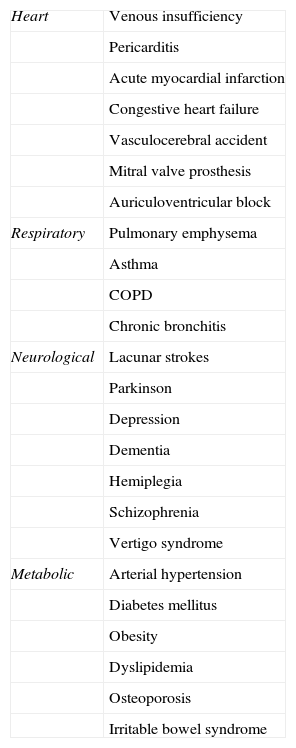
We also reviewed comorbidities (Table 2) at the time of the fracture. In total, 12 of the 72 patients did not present comorbidities at the time of the fracture, whilst the rest presented more than 1 comorbidity.
Types of comorbidities at the time of fracture.
| Heart | Venous insufficiency |
| Pericarditis | |
| Acute myocardial infarction | |
| Congestive heart failure | |
| Vasculocerebral accident | |
| Mitral valve prosthesis | |
| Auriculoventricular block | |
| Respiratory | Pulmonary emphysema |
| Asthma | |
| COPD | |
| Chronic bronchitis | |
| Neurological | Lacunar strokes |
| Parkinson | |
| Depression | |
| Dementia | |
| Hemiplegia | |
| Schizophrenia | |
| Vertigo syndrome | |
| Metabolic | Arterial hypertension |
| Diabetes mellitus | |
| Obesity | |
| Dyslipidemia | |
| Osteoporosis | |
| Irritable bowel syndrome |
COPD: chronic obstructive pulmonary disease.
The mean follow-up period was 8 years (range: 2–12 years).
Categorical variables were described through frequencies and percentages and quantitative variables through mean and standard deviation. The bivariate analysis was carried out through the Chi-squared test or Fisher's exact test in the case of categorical variables, the Student's t test for independent data and the analysis of variance (ANOVA) to compare quantitative variables.
Lastly, we used a multivariate model of binary logistical regression to assess the factors related to autonomy. In all cases we considered as statistically significant values of P<.05. The statistical analysis was carried out with the software package SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
ResultsThe distribution of patients is shown in Fig. 1. Of the 14 deceased patients, 9 cases involved the right shoulder and 3 cases involved the left shoulder, with 10 patients being right-handed and 2 being left-handed, and with a mean period of 4.2 years (range: 0.5–9 years) since the intervention until death in the right shoulder group and 3 years (range: 3–10 years) in the left shoulder group. Only 1 case died during the first year after the intervention (the patient had a history of mammary carcinoma), for causes unrelated to the fracture of the proximal humerus.
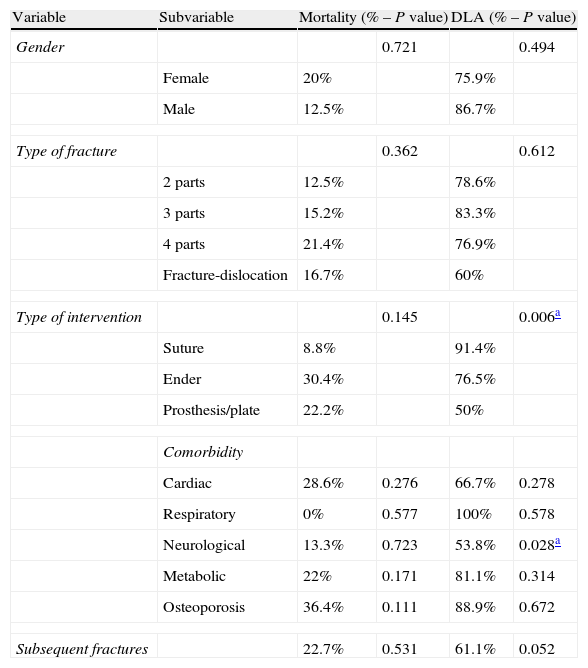
The distribution of mortality according to the type of fracture was as follows: 2 deaths among patients with fractures in 2 parts, 5 among patients with fractures in 3 parts, 3 among patients with fractures in 4 parts and 1 in a patient with a fracture-dislocation in 4 parts. No statistically significant correlation between mortality and the type of fracture was observed (P=.362).
We observed less deaths among patients treated with transosseous sutures (3 patients), whereas the number of deaths increased slightly among those treated by transosseous suture and Ender nails (7 patients), without reaching statistical significance (P=.92). The mode of treatment was not correlated with mortality (P=.145). We obtained a statistically significant correlation between age and the treatment applied, with those patients treated by prosthesis, transosseous sutures and Ender nails being older than the rest (P=.003).
We found a greater number of comorbidities among deceased patients. Respiratory disease was not present in any case of death, whereas metabolic disease was present in 13 cases, heart disorders in 4 and neurological disorders in 2 cases. In general, all deceased patients presented more than 1 comorbidity.
There were 4 deaths among patients who were diagnosed with osteoporosis prior to the fracture (all of them through bone densitometry). All osteoporotic patients with no comorbidity were still alive at the time of the interview.
Regarding the level of dependence for DLA, nearly all of the patients (79.5%) were totally independent for daily life activities at the end of the follow-up period. We found no significant correlation between the type of fracture and autonomy for DLA (P=.612). We observed that the type of treatment had a significant influence on the final autonomy for DLA of the 35 patients treated with transosseous suture, with 32/35 (91.4%) being totally independent. Of the 17 patients treated with transosseous sutures and Ender nails, 13/17 (76.5%) were independent, whilst among those treated with an angular stability plate or shoulder prosthesis, only 50% were fully independent for DLA (P=.006).
Out of the 13 patients with neurological disorders, only 53.8% were autonomous for DLA. Patients suffering Parkinson's disease and different types of dementia were already dependent before the intervention, as well as 1 patient who had been previously diagnosed with Ménière syndrome, 1 with essential tremor and 2 with depression who ceased to be independent for DLA after suffering the fracture and subsequent intervention.
A statistically significant correlation was found between neurological disorders and a lack of autonomy for DLA (P=.028). Conversely, heart disease, respiratory disease and metabolic disease did not worsen the capacity for DLA.
No significant correlation was found in relation to capacity for DLA between patients diagnosed with osteoporosis at the time of the fracture or subsequently to the fracture (P=.672).
In 18 patients (24%) we found other fractures after the proximal humerus fracture, including: 9 fractures of the proximal end of the femur, 4 vertebral fractures, 5 fractures of the distal radius, 2 clavicular fractures, 1 bimalleolar ankle fracture, 1 patellar fracture, 1 fracture of the contralateral proximal humerus and 1 fracture in the metacarpus of the hand.
Only 61.1% of those who suffered associated fractures continued to be autonomous for activities of daily life. Patients without additional fractures were significantly more autonomous for DLA than those who suffered other fractures (P=.05).
Only 11.3% of patients had been previously diagnosed and treated for their osteoporosis before the proximal humeral fracture. This condition did not significantly affect the type of fracture or the presence of additional fractures (P=.283) (Table 3).
Relationship between gender, type of fracture, type of intervention, comorbidity, osteoporosis, subsequent fractures and mortality/daily life activities (DLA).
| Variable | Subvariable | Mortality (% – P value) | DLA (% – P value) | ||
| Gender | 0.721 | 0.494 | |||
| Female | 20% | 75.9% | |||
| Male | 12.5% | 86.7% | |||
| Type of fracture | 0.362 | 0.612 | |||
| 2 parts | 12.5% | 78.6% | |||
| 3 parts | 15.2% | 83.3% | |||
| 4 parts | 21.4% | 76.9% | |||
| Fracture-dislocation | 16.7% | 60% | |||
| Type of intervention | 0.145 | 0.006a | |||
| Suture | 8.8% | 91.4% | |||
| Ender | 30.4% | 76.5% | |||
| Prosthesis/plate | 22.2% | 50% | |||
| Comorbidity | |||||
| Cardiac | 28.6% | 0.276 | 66.7% | 0.278 | |
| Respiratory | 0% | 0.577 | 100% | 0.578 | |
| Neurological | 13.3% | 0.723 | 53.8% | 0.028a | |
| Metabolic | 22% | 0.171 | 81.1% | 0.314 | |
| Osteoporosis | 36.4% | 0.111 | 88.9% | 0.672 | |
| Subsequent fractures | 22.7% | 0.531 | 61.1% | 0.052 | |
In total, 59.4% of patients described the result obtained in their shoulder as very satisfactory, 32.8% as satisfactory and 7.8% as unsatisfactory. Satisfaction was significantly correlated with autonomy for DLA at the end of the follow-up period (P=.003).
DiscussionThe best treatment option for proximal humerus fractures has not yet been defined. At the time of deciding on the treatment, the surgeon must take into account the fact that patients treated by surgery have a high mortality rate, especially those presenting comorbidities. In the present study, patients with surgically treated proximal humerus fractures who presented comorbidities seemed to have a higher mortality risk. On the other hand, the majority of surgically treated patients who remained alive at the end of the follow-up period remained autonomous and were able to live independently, except for those with neurological comorbidities.
In our study of proximal humerus fractures treated surgically, mortality during the first year was limited to 1 patient. This lower mortality rate during the first year can be explained by the fact that patients eligible for surgery are generally those who are most suitable and do not present serious diseases. Despite the fact that 85.4% of the patients included presented some comorbidity at the time of the fracture, this did not significantly harm patients.
Mortality increased to 18.6% throughout the follow-up period (with a mean duration of 8 years), significantly higher than the mortality rate expected in a group of comparable age and gender in Spain, according to the National Statistics Institute (the combined rate of deaths among males and females at the age of 72 years was of 16.67 per 1000 in 2012).25 We only found deaths in patients with comorbidity at the time of the fracture and with no correlation with the type of fracture or the treatment applied, which means that special attention should be paid to comorbidities when facing the decision of applying surgical treatment to proximal humerus fractures, although in our study we did not identify a significant relationship. A study conducted on a sample French population found a mortality rate of 9.1% in patients with proximal humerus fractures and a mean follow-up period of 4 years.26 Another work in the same line of analysis found a mortality rate of 0.6% after 1 year of having suffered a proximal humerus fracture treated conservatively.27
The results obtained in this work indicate that the majority of patients who underwent surgery due to fractures of the proximal humerus and who were in good condition in terms of autonomy and capacity for DLA, did not vary after the treatment. When comparing quality of life through the HRQol test between elderly patients intervened due to fractures of the proximal humerus and those treated conservatively, similar studies, such as that by Fjalestad et al. obtained a mean result of 0.841 among patients treated surgically and 0.819 among those treated conservatively at 1 year follow-up, thus favoring surgical treatment.28
The surgical treatment of proximal humerus fractures is highly efficient in terms of patient autonomy and capacity for DLA. In our study, neurological disorders were the main consideration in the recovery of previous capacity for DLA. The indication for surgery should only be adopted with precaution, as patients may not regain their prior capacity for DLA and the mortality rate may increase. Calvo et al. conducted a study of proximal humerus fractures treated conservatively among a sample population of Spanish patients analogous to ours in which 32.6% suffered depression or anxiety after the intervention.29
The majority of patients with proximal humerus fractures treated surgically in the present study (79.5%) regained their previous capacity for DLA and were able to live at their home. These data differ from those obtained with other types of fractures, like hip fractures, in which only 55% of patients with stable pertrochanteric hip fractures treated surgically regained the capacity to walk after the fracture and only 66% regained their level of capacity for DLA prior to the fracture, thus indicating that a severe decline can be expected after hip fractures.18
The type of fracture does not influence the capacity for DLA. However, the treatment applied significantly influences the level of autonomy of patients. A greater deterioration for DLA was observed among patients treated surgically through hemiarthroplasty, and only 50% of them were fully independent. This result agrees with the expected functional results in hemiarthroplasties for proximal humerus fractures. In a series of hemiarthroplasties in comminuted fractures of the proximal humerus, Grönhagen et al. found that only 25 out 46 patients examined (54%) considered the function of the intervened shoulder to be satisfactory. They observed that neurological disorders also had a significant effect on DLA, and only 53.8% of patients with prior neurological disorders regained a full capacity for DLA after the intervention.5 Calvo et al. found that, at 6 months after the fracture, 43.5% of patients reported difficulties for personal hygiene and 56.5% for normal activities of daily life, with only 13% of them being fully dependent.29
Although it is widely recognized that proximal humerus fractures are osteoporotic and can be associated to subsequent additional fractures,30 the data obtained in the present study suggest that osteoporosis is underdiagnosed in the population selected, since only 11.3% of patients had been previously diagnosed and treated for osteoporosis prior to the proximal humeral fracture and up to 24% of our patients presented additional fractures during follow-up. Calvo observed that only 35.8% of patients who had suffered a fracture of the proximal humerus treated conservatively had been previously diagnosed with osteoporosis.29
Proximal humerus fractures still represent a challenge for decision making and treatment. Aspects like morbidity and mortality, the possibility of regaining capacity for DLA and osteoporosis must be taken into consideration, along with the type of fracture and techniques, in order to offer the best possible treatment option.
Study limitationsThis was a retrospective study with a small sample. It would also require a validated test for DLA.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Isart A, Sánchez JF, Santana F, Puig L, Cáceres E, Torrens C. Morbimortalidad en fracturas de húmero proximal tratadas quirúrgicamente. Rev Esp Cir Ortop Traumatol. 2014;58:223–228.