The traditional treatment of unstable symptomatic discoid meniscus (DM) has been total or subtotal meniscectomy. However, long-term studies show that the results are poor. The aim of this study was to evaluate the clinical outcomes and survival of arthroscopic saucerization combined with peripheral repair for the treatment of symptomatic discoid meniscus in children.
MethodsPatients ≤18 years with DM and a peripheral lesion treated between January 2012 and January 2018 were analyzed. Clinical results were evaluated using the Ikeuchi, Pedi-IKDC and Lysholm scales. The survival analysis was performed with the Kaplan-Meier method.
ResultsEighteen patients (18 knees) were treated in the evaluated period. The average age at the time of surgery was 11.1 ± 3.8 years. The average follow-up was 40.4 ± 21.2 months. An average of 3.4 ± 1 meniscal sutures (range, 2–6) was used. Repairs were carried out with a combination of inside-out and outside-inside techniques as dictated by the configuration of the injury. Sixteen patients could be evaluated functionally (2 lost of follow-up). Four patients presented mechanical symptoms. One was treated conservatively with physical therapy and three (18.8%) required further surgical treatment (subtotal meniscectomy). According to the Ikeuchi scale 12 (75%) had excellent results, 1 (6.2%) good and 3 (18.8%) poor (repair failure). The average Pedi-IKDC and Lysholm scores were 98.3 ± 2 and 98.7 ± 2.9 respectively at the last follow-up. The overall Kaplan-Meier survival probabilities after repair were 93.7% at 1 year, and 85.9% at 2 years.
ConclusionsMid-term outcomes of saucerization in conjunction with meniscal repair are encouraging for children with a symptomatic unstable discoid meniscus.
El tratamiento tradicional del menisco discoide (MD) sintomático inestable ha sido la meniscectomía total o subtotal. Sin embargo, estudios a largo plazo demuestran que los resultados son pobres. El objetivo de este estudio fue evaluar los resultados clínicos y supervivencia de la remodelación artroscópica combinada con la reparación periférica para el tratamiento del menisco discoide sintomático en niños.
MétodosSe analizaron todos los pacientes ≤18 años con MD y una lesión periférica tratados entre Enero 2012 y Enero 2018. Las reparaciones se llevaron a cabo con una combinación de técnicas de dentro-fuera y fuera-dentro según lo dictado por la configuración de la lesión. Los resultados clínicos se evaluaron utilizando las escalas de Ikeuchi, Pedi-IKDC y Lysholm. El análisis de supervivencia se realizó con el método de Kaplan-Meier.
ResultadosEn el período evaluado se trataron 18 pacientes (18 rodillas). El promedio de edad al momento de la cirugía fue 11.1 ± 3.8 años. El promedio de seguimiento fue 40.4 ± 21.2 meses. Se utilizó un promedio de 3.4 ± 1 suturas (rango, 2 a 6). Dieciséis pacientes pudieron ser evaluados funcionalmente (2 pérdidas de seguimiento). Cuatro pacientes presentaron síntomas mecánicos. Uno fue tratado de manera conservadora con fisioterapia que alivió los síntomas y tres (18.8%) requirieron una nueva cirugía (meniscectomía subtotal). De acuerdo a la escala de Ikeuchi 12 (75%) tuvieron resultados excelentes, 1 (6.2%) bueno y 3 (18.8%) malos (falla de la reparación). Las puntuaciones promedio Pedi-IKDC y Lysholm fueron 98.3 ± 2 y 98.7 ± 2.9 respectivamente al último seguimiento. Las probabilidades generales de supervivencia de Kaplan-Meier después de la reparación fueron del 93.7% a 1 año y del 85.9% a los 2 años.
ConclusionesLos resultados a medio plazo de la saucerización asociada a la reparación periférica son alentadores en niños y adolescentes con MD inestable sintomático.
Discoid meniscus (DM) is a structural impairment characterised by increased thickness and diminished and disorganised collagen fibres that affect meniscal shape and stability.1,2 Its frequency of presentation varies from .4% to 20%.3–5 This condition can be detected incidentally in asymptomatic patients or present with clinical symptoms of pain, effusion and intra-articular snapping.6
Patients who are diagnosed with DM but who do not present symptoms do not require treatment. In cases where the DM is stable but symptomatic, the treatment of choice is saucerisation (partial meniscectomy). This treatment seeks to achieve a meniscus that is more similar to normal and provides satisfactory results in the short and medium term.7–9 Approximately one third of patients requiring surgical treatment often have unstable peripheral lesions.10 The traditional treatment for symptomatic, unstable DM has been total or subtotal meniscectomy. However, long-term studies show that the results are poor due to instability and degenerative changes of the lateral compartment.11–15 Along with the advances in arthroscopic techniques of meniscal repair, more recent studies recommend preservation of the meniscus through saucerisation and peripheral stabilisation.8,13,14,16 There is little information in the literature on the effectiveness of this technique in paediatric patients.
The aim of this study was to assess the clinical outcomes and survival of arthroscopic remodelling combined with peripheral repair for the treatment of symptomatic DM in children.
Material and methodsStudy designThis study was approved by the ethics committee of our institution prior to the start of the study. The medical records of all patients ≤18 years of age with an arthroscopic diagnosis of external DM treated between January 2012 and January 2018 who underwent remodelling (central meniscectomy) and peripheral repair by arthroscopy were reviewed retrospectively. All the children were operated in the same institution, by the same specialist. Patients with associated ligament injuries and follow-up of less than one year were excluded for the analysis.
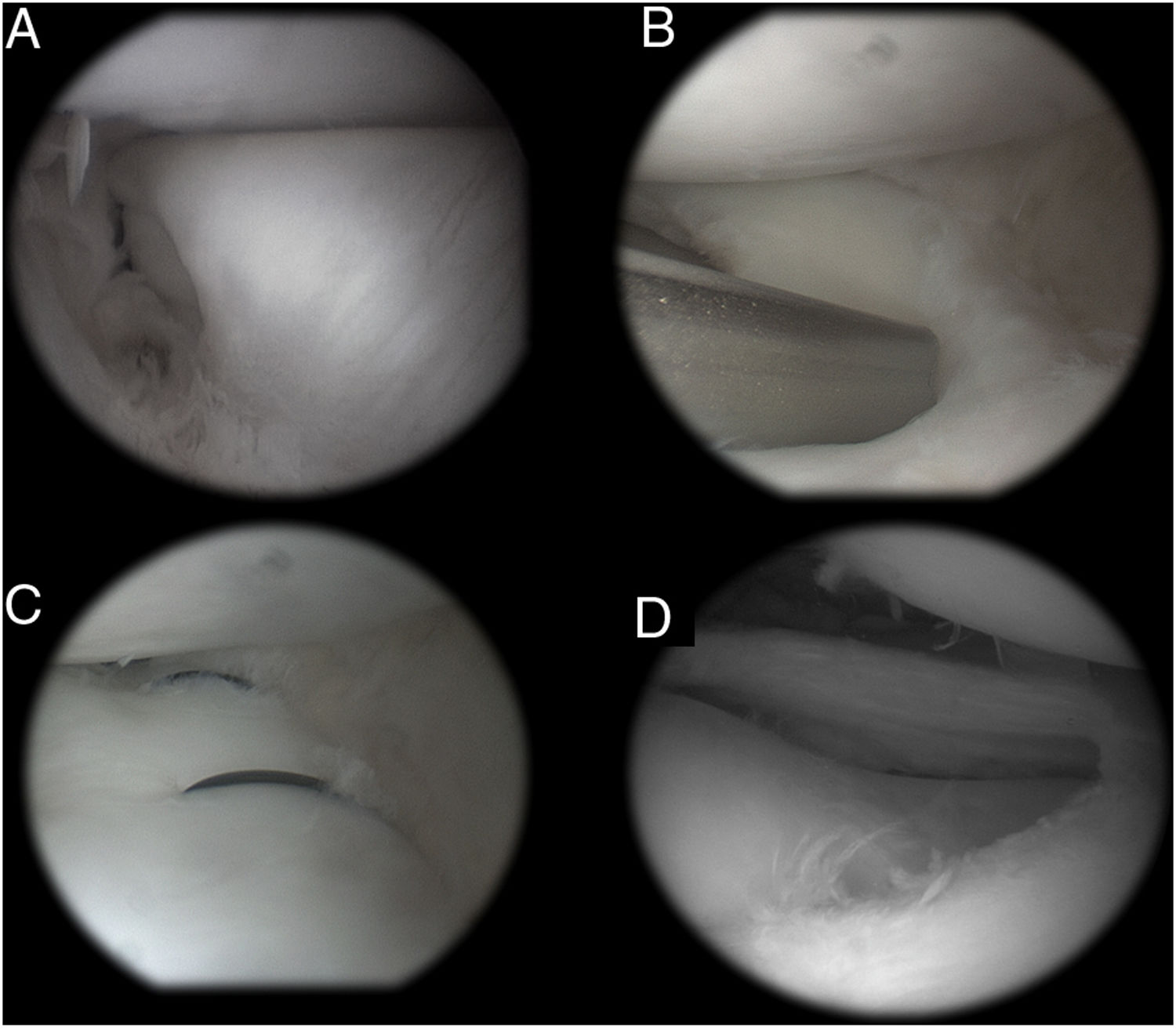
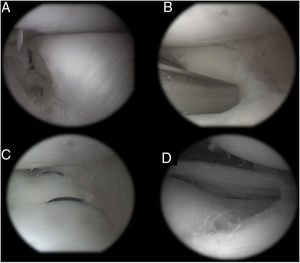
Surgical techniqueThe procedure is performed in the operating theatre, under spinal or general anaesthesia as an outpatient procedure. A prophylactic dose of intravenous cefazolin is administered, depending on the patient's weight, 30 min before the incision. The arthroscopic procedure is performed through medial and lateral parapatellar portals. The lesion is identified and characterised according to size, location and tissue quality. If the lesion can be reduced anatomically and the meniscal tissue is of good quality, the decision is made to perform the repair. Initially, meniscal remodelling is performed, leaving 6−8 mm of meniscus free in the periphery. The edges of the lesion are abraded with a synoviotome. Once reduced, the meniscus is stabilised with 2–6 inside-outside or outside-inside systems according to the pattern of the injury, and predominantly in a vertical pattern. When the lesion is located in the posterior horn of the external meniscus, a posterolateral approach is combined with protection of the common peroneal nerve (Fig. 1). Once the final repair has been achieved, a microfracture punch or a 2 mm pin is used in the intercondylar notch to make 2 holes to encourage a favourable environment for the repair
In the postoperative period, a knee immobiliser is prescribed for 4 weeks without support and a range of motion from 0° to 60°. Between weeks 4–6, partial non-weight bearing (50%) and a range of motion from 0° to 90° is indicated. From week 6 full support and progression to full range of motion is allowed. Return to sport is permitted after 6 months.
Assessment of patientsWe documented demographics (age, sex, affected knee, skeletal maturity), time from symptom onset to surgery, postoperative complications related to the procedure (pain, infection, locking, effusion, etc.), and the need for re-intervention. The morphology of the DM was described as complete or incomplete depending on whether or not they completely covered the tibial plate.17 Arthroscopic findings were classified into 3 types in terms of peripheral edge stability and lesion location according to the system of Ahn et al.18: 1) anterior horn meniscocapsular junction (type MC-A), 2) posterior horn meniscocapsular junction (type MC-P) and 3) posterolateral corner.
The functional results were assessed with the Lysholm19 and Pedi-IKDC20 scales. The criteria for clinical success were based on the Ikeuchi scale.21 An excellent result indicates absence of mechanical symptoms, absence of pain and a full range of motion. A good result indicates no mechanical symptoms, mild and occasional pain with exercise, and a full range of motion. A fair result indicates mechanical symptoms, mild to moderate pain with exercise and a full range of motion. A poor result indicates the presence of mechanical symptoms, moderate to severe pain with exercise, and limited range of motion of the joint.
Statistical analysisThe quantitative variables are described as means and standard deviation. Absolute frequencies were used to describe the qualitative variables. The survival analysis was performed with the Kaplan-Meier method. Time to repair failure was defined as the interval between the meniscal repair and revision (subtotal meniscectomy). MedCalc® version 12.7.8 was used for the survival analysis.
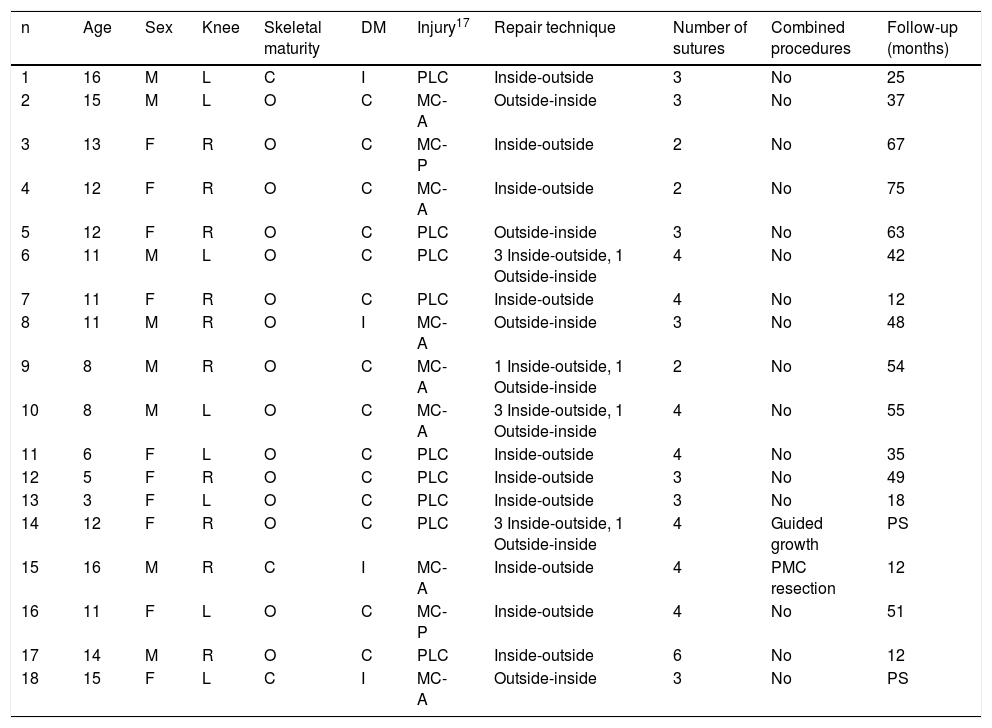
ResultsA total of 375 knee arthroscopies were performed between January 2012 and January 2018 in patients ≤18 years of age. Forty-five patients had an arthroscopic diagnosis of external DM, of whom 18 patients had a peripheral injury treated with central meniscectomy combined with peripheral repair. All had pain, joint protrusion and/or joint locking. The mean age at the time of surgery was 11.1 years (range, 3–16). The progression of symptoms was 93.1 days (range, 21–360). The mean follow-up was 40.4 months (range, 10–75). The demographic data of the patients evaluated are shown in Table 1.
Demographic data of the sample.
| n | Age | Sex | Knee | Skeletal maturity | DM | Injury17 | Repair technique | Number of sutures | Combined procedures | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 16 | M | L | C | I | PLC | Inside-outside | 3 | No | 25 |
| 2 | 15 | M | L | O | C | MC-A | Outside-inside | 3 | No | 37 |
| 3 | 13 | F | R | O | C | MC-P | Inside-outside | 2 | No | 67 |
| 4 | 12 | F | R | O | C | MC-A | Inside-outside | 2 | No | 75 |
| 5 | 12 | F | R | O | C | PLC | Outside-inside | 3 | No | 63 |
| 6 | 11 | M | L | O | C | PLC | 3 Inside-outside, 1 Outside-inside | 4 | No | 42 |
| 7 | 11 | F | R | O | C | PLC | Inside-outside | 4 | No | 12 |
| 8 | 11 | M | R | O | I | MC-A | Outside-inside | 3 | No | 48 |
| 9 | 8 | M | R | O | C | MC-A | 1 Inside-outside, 1 Outside-inside | 2 | No | 54 |
| 10 | 8 | M | L | O | C | MC-A | 3 Inside-outside, 1 Outside-inside | 4 | No | 55 |
| 11 | 6 | F | L | O | C | PLC | Inside-outside | 4 | No | 35 |
| 12 | 5 | F | R | O | C | PLC | Inside-outside | 3 | No | 49 |
| 13 | 3 | F | L | O | C | PLC | Inside-outside | 3 | No | 18 |
| 14 | 12 | F | R | O | C | PLC | 3 Inside-outside, 1 Outside-inside | 4 | Guided growth | PS |
| 15 | 16 | M | R | C | I | MC-A | Inside-outside | 4 | PMC resection | 12 |
| 16 | 11 | F | L | O | C | MC-P | Inside-outside | 4 | No | 51 |
| 17 | 14 | M | R | O | C | PLC | Inside-outside | 6 | No | 12 |
| 18 | 15 | F | L | C | I | MC-A | Outside-inside | 3 | No | PS |
LF: Lost to follow-up; PMC: Parameniscal cyst.
Skeletal maturity: A: Open physis; C: Closed physis.
Discoid meniscus (MD) I: incomplete; C: complete.
Injury: Type MC-A: anterior horn meniscocapsular junction; Type MC-P: posterior horn meniscocapsular junction, PLC: Posterolateral corner.
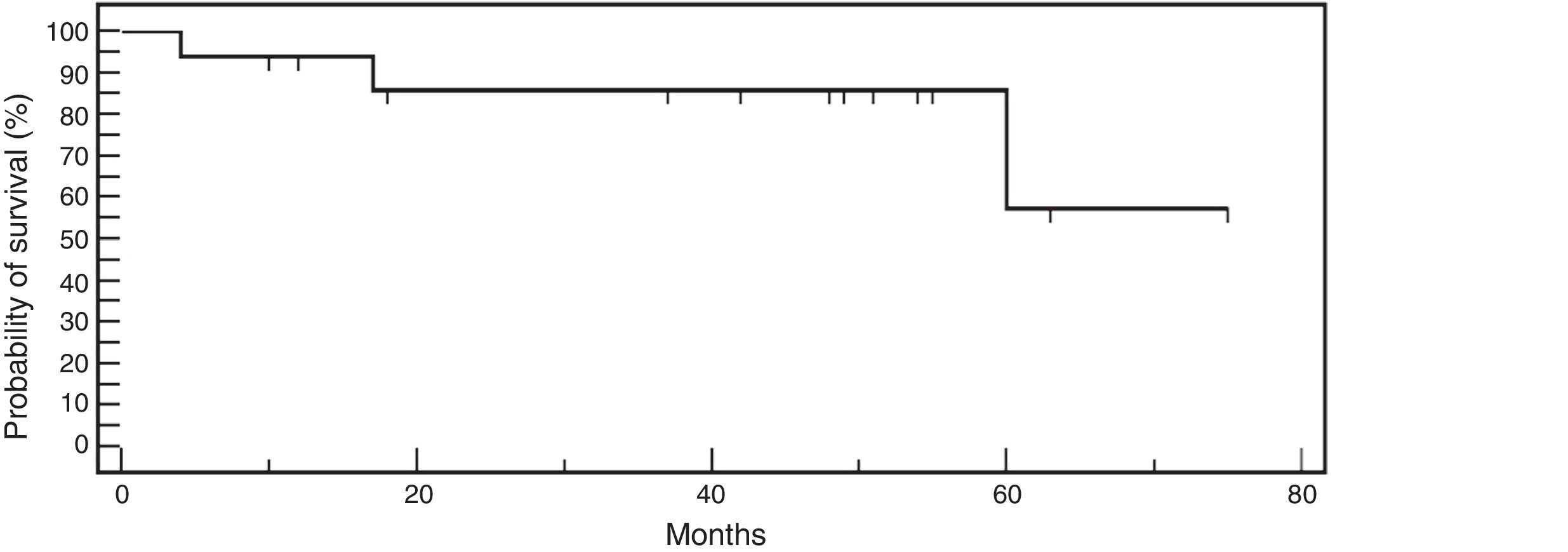
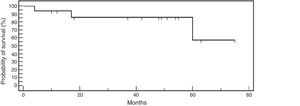
Sixteen patients could be located and functionally assessed (2 patients were lost to follow-up). According to the Ikeuchi scale, 12 had excellent results, one good and 3 bad (repair failure). Four patients had mechanical symptoms. One was treated conservatively with physiotherapy, the symptoms subsided, and 3 required surgery (subtotal meniscectomy). These patients did not present statistically significant differences in terms of age, sex, type of meniscus (complete/incomplete) but presented a tendency to a longer symptom progression time (3.83 months vs. 2.9 months; P = .58). One patient had an acute failure (at 4 months) and the other 2 delayed failure while practising sports (17 and 60 months). The average Pedi-IKDC and Lysholm scores in the patients who did not require revision were 98.3 ± 2 and 98.7 ± 2.9 points respectively at the last follow-up (Table 2). The overall Kaplan-Meier survival probabilities after repair were 93.7% at one year and 85.9% at 2 years (Fig. 2). All the patients, even those requiring revision, were able to return to their daily activities with little or no limitation.
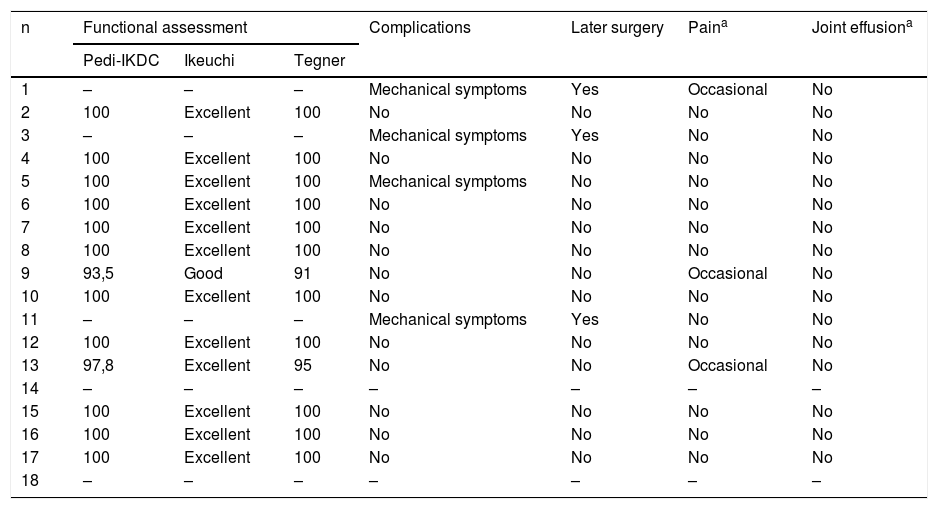
Functional results and complications.
| n | Functional assessment | Complications | Later surgery | Paina | Joint effusiona | ||
|---|---|---|---|---|---|---|---|
| Pedi-IKDC | Ikeuchi | Tegner | |||||
| 1 | – | – | – | Mechanical symptoms | Yes | Occasional | No |
| 2 | 100 | Excellent | 100 | No | No | No | No |
| 3 | – | – | – | Mechanical symptoms | Yes | No | No |
| 4 | 100 | Excellent | 100 | No | No | No | No |
| 5 | 100 | Excellent | 100 | Mechanical symptoms | No | No | No |
| 6 | 100 | Excellent | 100 | No | No | No | No |
| 7 | 100 | Excellent | 100 | No | No | No | No |
| 8 | 100 | Excellent | 100 | No | No | No | No |
| 9 | 93,5 | Good | 91 | No | No | Occasional | No |
| 10 | 100 | Excellent | 100 | No | No | No | No |
| 11 | – | – | – | Mechanical symptoms | Yes | No | No |
| 12 | 100 | Excellent | 100 | No | No | No | No |
| 13 | 97,8 | Excellent | 95 | No | No | Occasional | No |
| 14 | – | – | – | – | – | – | – |
| 15 | 100 | Excellent | 100 | No | No | No | No |
| 16 | 100 | Excellent | 100 | No | No | No | No |
| 17 | 100 | Excellent | 100 | No | No | No | No |
| 18 | – | – | – | – | – | – | – |
Cases 1, 3 and 11 had repair failures. Cases 14 and 18 were lost to follow-up.
The aim of surgical treatment of a meniscal injury is to restore the biomechanics of the knee, relieve symptoms and minimise progression to osteoarthritis. The implementation of meniscal repair has been shown to reduce the incidence of osteoarthritis in the long term compared to total or partial meniscectomy.22,23 Although there are multiple studies that show favourable outcomes in non-discoid meniscus in the paediatric-adolescent population,24 there is little information available on meniscal repair in DM.
Ahn et al.18 studied the results of this technique in 28 knees of 23 patients. The mean age was 9 years (range, 4−15 years). No patient required revision at a mean follow-up of 51 months. Mean Lysholm scores improved from 78.5 (range, 69–89) to 95.5 (range, 85–100) at final follow-up (P < .001), and HSS improved from 80.3 (range, 69–89) to 95.9 (range, 90–100) at final follow-up (P < .001). More recently, the same authors25 studied the results of 18 knees that could be analysed over a longer follow-up. Over 90% were rated "excellent" or "good" at mean follow-up of 10 years. However, 39% of the patients showed evidence of degenerative changes on follow-up x-rays. This finding indicates that the early onset of radiographic changes suggestive of osteoarthritis does not necessarily correlate with the development of knee symptoms, although long-term follow-up of these patients into adulthood is clearly necessary. Carter et al.25 assessed 57 knees with stable and unstable DM that underwent remodelling alone and remodelling combined with peripheral fringe stabilisation respectively. In an average short-term follow-up (15 months), both patient populations had equivalent results, with the complication rate of the second group being 12%. The authors concluded that peripheral stabilisation would not adversely affect outcomes if instability is recognised and treated. Shieh et al.26,27 evaluated 46 remodelling and stabilisation procedures. At an average of 40 months, 15% of the cohort required a revision procedure.
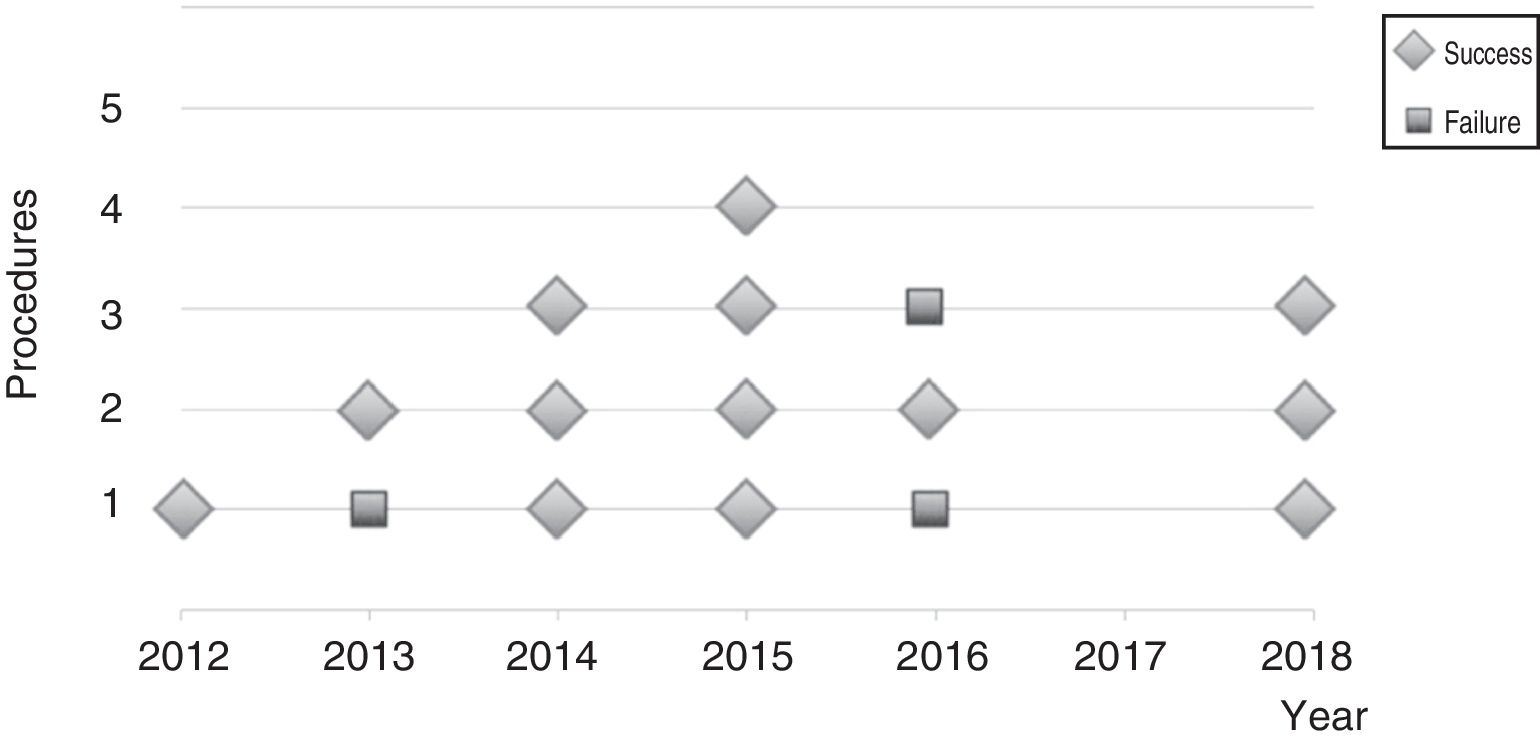
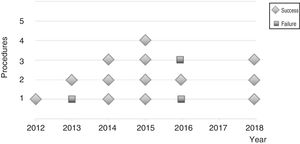
In our study we observed excellent or good functional outcomes in more than 80% of the sample. Four patients presented mechanical symptoms after surgery. One was treated conservatively with remission of symptoms and 3 required revision (subtotal meniscectomy). These patients tended to have longer symptom progression times, although there were no differences in other demographic characteristics which could be due to the small sample size. These 3 failures would not be related to the experience of the surgeon either (Fig. 3). When analysing survival, almost 86% of the patients operated had maintained their external meniscus with good function 2 years after the operation. This percentage decreased to 57.3% after 5 years, although this last percentage is not very representative and should be viewed with caution since only 19% of the sample had had 5 years of follow-up at the time of the evaluation.
The results of this study should be interpreted in the context of a retrospective design study. Although the sample size is limited, which does not enable us to establish predisposing factors for repair failure, it is comparable to other studies with similar characteristics.28,29 In order to perform a multivariate analysis, a study including several centres with surgeons with a similar level of training, surgical volume and experience would be required. Moreover, the functional scales used, although translated into Spanish, are not validated in our language. The time of symptom progression was recorded according to the indirect anamnesis (parents) in the youngest patients. These data could present some inconsistencies since some did not remember exactly the time of onset of the symptoms. Finally, the minimum follow-up of one year is relatively short. While allowing us to detect early failures, results in patients with DM tend to decline with long-term follow-up.30 We consider that a multicentre study would be ideal with clinical-radiographic evaluation and a minimum follow-up of 5 years.
ConclusionThe medium-term results of arthroscopic remodelling combined with peripheral repair are encouraging in children and adolescents with symptomatic unstable DM.
Level of evidenceLevel of evidence IV – Case series.
Conflict of interestsThe authors have no conflict of interests to declare.
We thank would like to thank Silvia Barzón (Bioch. Sp.) for her help in interpreting the data and statistical analysis
Please cite this article as: Carabajal M, Allende GJ, Masquijo JJ. Resultados a mediano plazo de la remodelación artroscópica asociada a reparación periférica en niños con menisco discoide inestable. Rev Esp Cir Ortop Traumatol. 2020;64:206–212.