To analyze the results of unipolar modular radial head arthroplasty in the treatment of complex fractures associated with elbow joint instability.
Materials and methodsRetrospective design study of 44 patients, 17 men and 27 women with a mean age of 51 years (17–78) who suffered radial head fractures (Mason III) in the context of an unstable elbow injury. Mean follow-up was 21.2 months (12–60). Radial head replacement was performed with a unipolar modular prosthesis with a fixed stem (Ascension® Modular Radial Head, MRH), associating repair of concomitant lesions. The “Mayo scale Elbow Performance Score” (MEPS) was used to perform the functional assessment. A radiological evaluation was performed at the last follow-up and the complications were recorded.
ResultsFinal arc of flexion–extension was 108° with an average of 135° of prono-Supination. At final follow-up, 82% of results were satisfactory according to the MEPS. 40% of patients (17) had radiographic signs of lucencies around the stem, although most of them were asymptomatic. Two of them needed a second surgical procedure because of painful prosthetic loosening and further surgery was required for a prosthesis dislocation.
DiscussionRadial head implants are an adequate treatment option for restoring stability in complex radial head fractures. Modularity allows a wide range of size combination and helps to avoid overstuffing. Periprosthetic osteolysis could be associated with the presence of pain, so it is necessary to perform long-term studies to test the potential complications of this finding.
Analizar los resultados de la artroplastia monopolar modular de cabeza radial como tratamiento de fracturas complejas del codo asociadas a inestabilidad articular.
Material y métodoEstudio retrospectivo de 44 pacientes, 17 varones y 27 mujeres con edad media de 51 años (17-78) que fueron intervenidos de fracturas de cabeza radial tipo III de Mason, en el contexto de lesiones inestables del codo. El seguimiento medio fue de 21,2 meses (12-60). La sustitución de la cabeza radial se realizó con una prótesis monopolar modular de vástago fijo, denominada Ascension® Modular Radial Head (MRH), asociando la reparación de las lesiones concomitantes en el mismo acto quirúrgico. Para la evaluación funcional se utilizó la escala “Mayo Elbow Performance Score” (MEPS). También se registraron los hallazgos radiográficos y complicaciones durante el seguimiento.
ResultadosEl arco final de flexo-extension fue de 108° con una prono-supinación media de 135°. Al final del seguimiento, el 82% de los resultados fueron satisfactorios de acuerdo con la “MEPS”. El 40% de los pacientes (17) presentaron signos radiográficos de radiolucencia alrededor del vástago que resultaron asintomáticos. Dos de estos dicisiete pacientes precisaron reintervención por aflojamiento protésico doloroso y una nueva cirugía fue necesaria por luxación de la prótesis.
DiscusiónLos implantes monopolares son una opción válida de tratamiento para restaurar la estabilidad en fracturas complejas de cabeza radial. Su modularidad permite ampliar la selección de tamaños y evitar el pinzamiento radio-capitelar. La osteolisis periprotésica no es siempre sinónimo de ausencia de sintomatología, siendo necesarios estudios con seguimiento más prolongado para valorar la asociación de este hallazgo con el desarrollo de complicaciones potenciales.
Radial head fractures are relatively common, accounting for one-third of all fractures occurring in the elbow.1–3 Approximately 85% of them occur between the ages of 20 and 60 years, due to falls on a bent arm, although they can also occur in the context of high energy trauma.1,2,4
The radial head is an important primary stabilizer against longitudinal stress on the elbow and a secondary stabilizer against valgus stress,1 recognized both in clinical and biomechanical studies.5,6 The ulnar portion of the lateral collateral ligament (LCL) is the primary stabilizer against varus and posterolateral elbow stress.1,7–9 Combined injury of these structures leads to the development of joint instability and, therefore, makes it necessary to repair them. Repair of the medial collateral ligament (MCL) is controversial, and some authors recommend repairing it if instability persists after repair of the radial head, the LCL and concomitant bone fractures. The use of an external fixator is recommended in case of residual instability.10,11
There are several treatment options for these lesions, depending on the fracture pattern and severity of the associated soft tissue injury.
Comminuted radial head fractures represent the main dilemma of this treatment, and often the clinical decision is based on the characteristics of each patient. Replacement through arthroplasty is the recommended treatment option in the context of unstable elbow injury and a comminuted radial head fracture.12
The use of bipolar arthroplasties, unipolar with a smooth stem or diaphyseal anchor and cemented arthroplasties has all been described, with similar functional outcomes, although each option has specific complications inherent to its design.
The aim of our study is the analysis of the clinical and functional results of unipolar modular arthroplasty of the radial head for the treatment of complex elbow fractures.
Materials and methodsWe designed a retrospective study of complex fractures of the radial head treated by arthroplasty, in the context of unstable traumatic elbow injuries, which had underwent surgery between 2007 and 2011.
The inclusion criteria were Mason type III fractures of the radial head3,13 with more than 3 articular fragments or any fracture with lost or irreparable fragments,14 presence of clinical–radiological instability criteria and lesions which had a minimum of 1 year follow-up after the surgical intervention.
Clinical instability was defined as the presence of joint dislocation associated with comminuted radial head fracture (Mason type IV), presence of elbow dislocation when forcing extension in a previously reduced or lax elbow when forcing varus–valgus. Radiological instability was defined when there was an opening of the radio-capitellar or ulnohumeral joint in elbow anteroposterior and lateral radiographs, respectively, at baseline with reduced elbow or forcing varus–valgus.
This led to the review of 44 patients, 17 males and 27 females, with a mean age of 51 years (range: 17–78 years). The right arm was injured in 27 cases, and in 22 of them it was dominant. The mean follow-up period was 21.2 months (range: 12–60 months). In all cases the preoperative study included anteroposterior and lateral elbow radiographs, as well as computed tomography (CT) scans with three-dimensional reconstruction. All patients underwent surgery in the first 2 weeks after injury.
A total of 35 radial head fractures occurred in the context of terrible triad elbow injuries, 3 were associated with transolecranon fracture-dislocations, 4 were associated with Essex Lopresti fracture-dislocations and, finally, 2 radial head fractures occurred in the context of Monteggia fracture-dislocations.
Surgical techniquePatients were placed in the supine position with the affected upper limb on a separate table. We used general anesthesia along with an interscalene brachial plexus block for the surgical procedure and postoperative pain management. In all cases we used a subaxillary pneumatic arterial tourniquet.
Once the patient was anesthetized, we verified joint stability with full elbow extension and in the forced varus–valgus maneuvers.
For fractures occurring in the context of a terrible elbow triad, we used a Kaplan-type lateral elbow approach15–17 to access the radial head (between radial carpal extensor muscles and the extensor digitorum communis muscle), as it enabled a better access to the radius and, especially, to the coronoid apophysis. In the remaining cases, when there was no associated coronoid fracture, we used the Kocher surgical approach to access the radial head15–17 (between the anconeus and extensor carpi ulnaris muscle).
The fragments of the radial head were removed and used to select the size of the prosthesis.15,18,19 Subsequently, we performed an osteotomy to regularize the neck of the radius. In order to determine the level of the section, we took into account the level of the fracture and, based on this, we used a standard or long resection guide. When conducting the osteotomy it was important to avoid removing too much of the radial neck, as this may cause instability of the implant.18,19 Intramedullary canal preparation began with the use of the punch tool and gradual milling to remove the spongy (or cancellous) bone. The use of test components enabled selection of the most appropriate size for the final implant. In order to obtain the closest approximation to the native anatomy, we used the lesser sigmoid notch of the coronoid as a reference to choose the final implant. Before inserting the final implant we verified its correct size with the test material. In cases where it was too “tight” we selected a final prosthesis of a smaller size than previously measured. This was done when there were space conflicts between the radial head of the selected implant and the humeral capitellum in any range of elbow movement.
In all cases, the prosthetic substitution of fracture fragments of the radial head was performed with a unipolar prosthesis: Ascension® Modular Radial Head (MRH) (Ascension Orthopedics, Austin, TX, USA), which comprised of 2 modular components, a stem and a head. The prosthesis has been anatomically designed to articulate with the ulna in a pronosupination movement and also to allow elbow flexion–extension through its articulation with the humeral capitellum.
The implant head was coated with a pyrolytic carbon layer deposited on a high-strength graphite substrate. It also contained an ultra-high molecular weight polyethylene (UHMPE) insert. The stem was made of titanium with a pyramidal design, so as to prevent rotation. Introduction of the stem into the canal molded in the radial neck was performed using a pressure anchor, without the use of cement.
In cases with complex instabilities we performed a comprehensive treatment of associated lesions. The LCL complex was repaired with bone anchors in 38 patients, and the coronoid apophysis was synthesized with a plate (Acumed®, Beaverton, OR, USA) in 6 cases. In 29 cases with apex fractures, we performed suture using harpoons. The 3 olecranon fractures were synthesized using 2 Kirschner wires and cerclage. In the event of an Essex-Lopresti fracture-dislocation, after replacing the radial head, we performed a temporary percutaneous fixation of the distal radio-ulnar joint with Kirschner wires. For ulnar osteosynthesis in the context of Monteggia fracture-dislocations, we used a plate with 3.5mm compression screws (dynamic compression plate, DCP) (DCP, Synthes® Zuchwil, Switzerland).
At the end of the intervention we assessed joint stability intraoperatively. The objective was to obtain a concentric reduction without posterior or posterolateral instability through a flexion–extension arc from 20° to 130°. If the elbow was considered unstable, we then proceeded to repair the MCL complex.10–12 This was necessary in 5 patients, in whom the MCL was repaired by direct suture in the fracture area through a medial approach. Only 1 case suffered persistence of instability after medial ligament repair, making it necessary to place an articulated external fixator to allow healing of the structures within a safe range of motion.
Management after the surgical intervention included a brachio-antebrachial splint which maintained the elbow immobilized at 90° flexion and the forearm in a neutral position for 5–7 days, in order to reduce edema and soft tissue inflammation. This was subsequently replaced by a hinged orthosis for 3 weeks to allow passive movement within a stable range, preventing full extension and supination. Full passive mobility was allowed after 4–6 weeks, and active mobilization without restriction after the sixth week. Shoulder abduction was avoided in order to limit varus stress on the elbow.
The evaluation took into account the degree of function, radiographic findings and complications. The Mayo Elbow Performance Score (MEPS) was employed for the functional asessment.20 The score on this scale is between 0 and 100 points, with 100 points being the best result. It assesses pain (45 points), mobility (20 points), stability (10 points) and the use of the elbow in daily life activities (25 points). Thus, the result was considered excellent with scores between 90 and 100 points, good with scores between 75 and 89 points, acceptable with scores between 60 and 74 points and poor with scores below 60 points. The assessment of the final result was satisfactory when the score was between good and excellent.
Joint stability was assessed by examining the presence of pain or laxity in flexion–extension, pronation–supination or when forcing varus–valgus in the affected elbow.
Radiological evaluation was performed through simple AP and LAT elbow Rx. We assessed the degree of posttraumatic arthritis according to the criteria by Broberg and Morrey.21 In addition, we defined the presence of heterotopic ossification according to the classification by Hastings and Graham,22 and also assessed the appearance of osteolysis or radiolucent areas in the neck of the radius or any radiographic evidence of humeral capitellum alterations and their association with pain symptoms.
Furthermore, we also recorded complications occurring during surgery and follow-up, both those common to any surgical procedure and those specific to this type of lesions.
ResultsRegarding the functional assessment according to the MEPS scale, the mean score obtained in the assessment of pain was 33 points (range: 12–45 points). Up to 77% of patients (34) did not present pain regularly, although occasional discomfort upon certain sudden movements or impacts and when lifting weight was reported. Six patients (13%) suffered frequent but tolerable discomfort in the affected elbow. Only 1 patient, who had been following conservative treatment, reported continuous daily pain in connection with ulnar nerve symptoms.
The final ulnohumeral flexion–extension arc was of 108° (range: 35–155°), with a mean flexion of 125° (range: 95–155°) and a mean flexion contracture of 20° (range: 0–60°). The final forearm rotation arc was of 135°, with a mean pronation of 70° and a mean supination of 60°.
No patient presented signs of instability during the follow-up examination.
The mean score during the assessment of elbow function was 19 points (range: 14–25 points). In general, most patients (87%) reported difficulty to practice sports with the affected arm, particularly those involving impact on the arm. Up to 35% were unable to carry heavy objects or place objects higher than their own height. In addition, 4 cases suffered limitations to basic activities of daily living, such as personal hygiene.
At follow-up, 82% of the results were satisfactory according to the MEPS classification. There were 6 excellent results, 30 good, 4 regular and 4 poor.
Up to 14 patients (32%) presented radiographic evidence of posttraumatic ulnohumeral arthritis which, in most cases, corresponded to grades I and II of the Broberg and Morrey classification. Only 1 patient presented severe radiographic changes due to posttraumatic arthritis (grade III). In total, 16 patients (37%) presented heterotopic ossifications. In most cases, these were located in the anterior region of the radio-capitellar joint, although in some patients they were located in the medial part of the elbow. These ossifications did not restrict the range of motion. Only 1 of these ossification cases corresponded to grade IIA in the Hastings and Graham classification (Fig. 1), with functional limitation in flexion–extension.
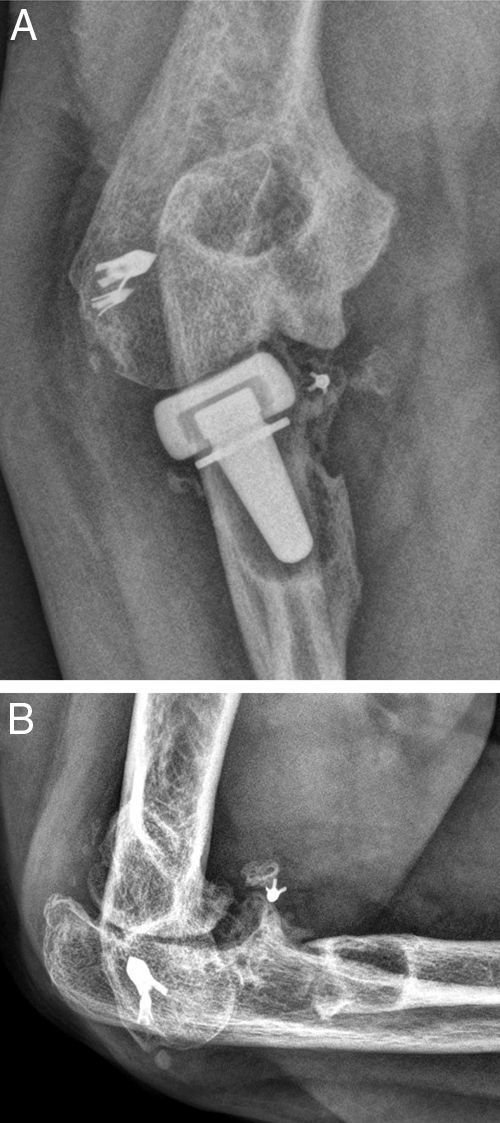
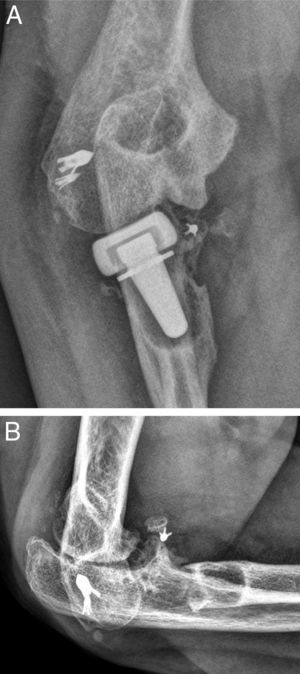
A total of 17 patients (40%) presented signs of radiolucency around the prosthesis stem, in most cases located in the proximal area of the prosthetic neck. Most of these (15) did not report any specific pain symptoms over the radial head. We also observed the presence of capitellar osteopenia in 6 patients (Fig. 2), although we could not demonstrate the implantation of an oversized prosthesis, through the existence of parallelism in the ulnohumeral joint in the elbow anteroposterior radiograph, in any of them.
There were no cases of deep or superficial infection in our series, nor were there differences regarding the results in the dominant and non-dominant sides.
A total of 9 patients (20%) suffered complications after the surgical procedure. We detected 2 lesions of the posterior interosseous nerve, 1 transient paresis and 1 complete axonotmesis with extension deficit of the metacarpophalangeal joints observed during the immediate postoperative period. After 2 years of follow-up, the patient wishes to continue with conservative management. In 1 case we observed a residual fragment of the radial head in a periarticular position during the postoperative control, but decided not to remove it because it had no functional impact. Approximately 1 year after the lesion, 3 patients suffered ulnar neuropathy sensory symptoms.
Three of the 9 patients (33%) who presented complications required a new surgical intervention for the treatment of their lesions. In one case, the patient suffered a dislocation of the prosthesis in the immediate postoperative period, which was treated by replacing the implant with another of a smaller size. The other 2 cases corresponded to painful aseptic loosening, with radiolucency around the entire prosthetic stem, requiring revision surgery. One was a patient who had suffered a “terrible triad” and who developed pain symptoms in the radial side of the elbow, with periprosthetic osteolysis, heterotopic ossifications and severe ulnohumeral osteoarthritis (or arthrosis) 4 years after the surgery (Fig. 3A and B). The patient was reintervened, with radial implant resection arthroplasty which led to the cessation of pain symptoms and a good functional result (Fig. 4A and B). The initial lesion in the other patient was an Essex-Lopresti fracture-dislocation which began with pain in the radial head, associated with signs of radiolucency around the prosthetic stem, 3 years after the initial surgery. The reoperation consisted of replacement with a new cemented prosthesis, leading to cessation of symptoms in the early postoperative period.
None of the patients required secondary surgery due to posttraumatic elbow stiffness. The greatest limitation of flexion (95°) appeared in a patient who presented heterotopic ossifications during follow-up (grade IIA in the Hastings and Graham classification) and who rejected the proposed surgery because he did not suffer functional limitations for his everyday activities (76 years old). Likewise, in the remaining patients in whom the range of motion was not complete, joint function was good enough not to require this type of intervention.
DiscussionIn the case of comminuted radial head fractures, the objective of treatment is to restore elbow stability, preserve mobility and maintain the relative length of the radius.1 This is achieved by an osteosynthesis of the fragments or, if this is not possible, by replacing the radial head by an implant. A repair is preferable in young patients with fractures associating 3 or less fragments with a sufficient size to carry out a stable osteosynthesis.14
Arthroplasty is usually indicated in cases of displaced and unstable fragments associated to other fractures or ligament injuries. Its use is also indicated in patients suffering persistent pain and instability after primary resection of the radial head, vicious union (or malunion), symptomatic pseudoarthrosis (or nonunion) and posttraumatic arthrosis.7,10,14 Excision of the radial head should be avoided in acute comminuted fractures due to its possible association with complex lesions of the ulnar LCL and interosseous membrane lesions, as it may cause premature osteoarthritis, instability and redislocation in the long term.23–26 Only in cases of isolated fractures where lesions causing instability have been ruled out can radial head resection be performed with good results, in patients younger than 40 years.27
In their studies, Harrington et al.,2,28 Moro et al.,29 and Grewal et al.30 found that metallic radial head prostheses could contribute to elbow stability in cases of unstable traumatic lesions. These authors established their results based on monopolar, monoblock, radial head prostheses intentionally inserted with some mobility into the radial neck, functioning as metallic spacers. Such implants differ from those employed in our series in that the latter had a fixed stem and their design was modular, thus allowing for a greater range of sizes and making it possible to obtain an adequate anatomical size.31 In any case, the results of these studies were similar to ours in terms of range of motion, functional ability and rate of complications.
The action of inserting the prosthesis through a pressure anchor required a very close approximation to the native anatomy, so that the new implant could function properly in the different positions of the elbow and forearm. This attachment of the stem to the medullary canal conferred greater stability to the assemblage, with radio-capitellar dislocation being infrequent.32 Cementing of the prostheses was usually reserved for revision surgery or tumoral cases, so its use for posttraumatic conditions was rare.31
In general, the ranges of flexion–extension (108°) and forearm rotation (135°) were similar to those reported by other series.2,18,28–32 It seems that the range of motion achieved was slightly higher in bipolar prostheses and there were no differences between surgical repair performed in acute conditions (less than 1 week since the lesion) or after 6 weeks.32 However, in works such as that by Bain et al.31 the worst results were obtained in fractures repaired after 15 days from the initial traumatic event. In our series, surgery was performed within the first 2 weeks from the trauma. Neither have the presence of “overstuffing”, subluxation of the prosthesis or instability been observed in any of our patients during long-term follow-up to explain the loss of supination, with any such findings being attributed to the nature of the injury rather than the presence of complications. Joint stiffness was not a cause for reoperation in any of our cases.
The appearance of radiolucency around the prosthesis was less frequent than with movable stem implants, which function as spacers, and was not usually associated with the presence of symptoms.18,30 However, in our study there were 2 cases of reoperation due to pain linked to prosthetic loosening, documented by plain radiography. These findings have already been highlighted in other publications,32 where osteolysis around the prosthetic stem was the most common radiological finding, resulting painful with moderate to severe intensity in all patients suffering from it. Osteolysis appeared to be less common in bipolar and monopolar prostheses with fixed stems, possibly due to lesser stress being transmitted. The absence of suspicious clinical data and negative analyses (erythrocyte sedimentation rate [ESR], C-reactive protein [CRP]) ruled out an association of this radiological finding with the presence of low-grade infection, so there was no need to extend the study with bone scintigraphy scans or joint arthrocentesis in patients with painless osteolysis. Cultures from the 2 replaced prostheses were negative.
In cases where the arthroplasty fails, removal of the radial implant may be an adequate option to restore function and prevent pain.
Another complication which required reoperation in our series was dislocation of the prosthesis in the early postoperative period, probably due to an inadequate choice of prosthesis size during surgery. Choosing the appropriate implant size is a crucial point to avoid complications like “overstuffing” or radiocapitellar impingement. Placement of an excessively large prosthesis can cause capitellar erosions, implant dislocation and abnormal friction of the radiocapitellar joint. Doornberg et al.18 advocate the use of the lateral edge of the coronoid, at the level of the lesser sigmoid notch, as a guide to determine the correct size, and, if in doubt, selecting the smallest size which adjusts to this reference. We used these criteria in all our patients. According to a biomechanical study by Pomianowski et al.,33 the development of bipolar prostheses would reduce capitellar friction and tension in the implant-bone interface, thus decreasing the possibility of subluxation and the need to adjust the size of the implant exactly.
Ulnar neuropathy is a possible sequel of this type of injury, so some authors18,34 have considered a prophylactic release/transposition of the ulnar nerve for complex reconstructive procedures in the elbow. Some series34 have reported up to 15% of cases with neurological symptoms after 2 years of surgery following a terrible elbow triad. Although there is scarce evidence in this respect, its relative frequency leads to investigate its possible causes, often difficult to determine: whether the lesion occurs during the surgical procedure itself, which seems unlikely, or is due to the initial trauma. The latter alternative could not be demonstrated in our series, since no patient suffered symptoms dependent on the ulnar nerve during the preoperative assessment. Late presentation after surgery could be related to inflammation, wound healing and thickening of the fibrous tunnel after the repair of the initial injury. The presence of osteophytes or heterotopic ossification near the path of the nerve can also cause long-term neurological lesions.34 In our series, 2 patients with ulnar symptoms presented signs of ulnohumeral arthrosis and ossifications in the medial elbow.
Among the main limitations of our study we highlight its retrospective nature and the absence of a control group. Moreover, it also covers a very heterogeneous set of injuries and has a limited follow-up period, although it does allow us to conclude that radial head arthroplasty with unipolar implants seems to be an appropriate management option to restore joint stability and biomechanics in complex lesions. Despite having some advantages, such as modularity, which expands the options for size selection and avoids radiocapitellar impingement, it also has some drawbacks. The presence of radiolucency around the prosthetic neck and radiographic changes in the capitellum may determine painful symptoms, which may require a new surgical intervention. Nevertheless, further studies with a longer follow-up period are needed in order to determine the true effect of the prosthesis on the articular cartilage and elbow biomechanics.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThis study has received no grants or financial aid.
Please cite this article as: Martín-Fuentes AM, et al. Resultados a medio plazo de la artroplastia monopolar modular de cabeza radial. Rev Esp Cir Ortop Traumatol. 2013;57:217–23.