To evaluate the use of unconstrained implants in the correction of large valgus deformities using total knee arthroplasty (TKA).
Material and methodA total of 817 primary TKA operated between 1998 and 2006 were retrospectively assessed. 50 TKA were selected (group A) in 49 patients, with a minimum deformity of 15° of valgus, 41 cases were included. Another 50 ATR were selected (group B), with a maximum deformity of 15° of varus, finally including 44 cases in 42 patients. The same surgeon performed every operation. The minimum follow-up time was 10 years. The Knee Society Score (KS and FS), the Oxford Knee Score (OKS) and the Range of Mobility (ROM), both preoperative and postoperative at 1, 5 and 10 years, as well as radiographic evolution and complications were evaluated.
ResultsPreoperative values of KS, FS and OKS were lower in group A (p<0.0001, p<0.01 and p<0.05, respectively), but not ROM. Postoperatively, KS, FS, OKS and ROM were not different between the groups, neither year, nor 5, nor 10 years. There were also no radiological or complications between the two groups.
DiscussionThe use of non-constricted implants in severe valgus was not inferior to the mild varus, implying, in addition, a saving in economic terms, with excellent postoperative results.
ConclusionsCorrection of severe valgus deformities can be performed with non-constrained primary implants, without obtaining worse results than those obtained in mild deformities.
Evaluar la utilización de implantes no constreñidos en la corrección de grandes deformidades en valgo mediante artroplastia total de rodilla (ATR).
Material y métodoFueron analizadas retrospectivamente 817 ATR primarias intervenidas entre 1998 y 2006; 50 ATR en 49 pacientes fueron seleccionadas (grupo A) con una deformidad mínima del 15° en valgo; se incluyeron 41 casos; 50 ATR fueron seleccionadas en el grupo B, con una deformidad máxima de 15° en varo, incluyendo finalmente 44 casos en 42 pacientes. El mismo cirujano realizó todas las ATR. El tiempo mínimo de seguimiento fue de 10 años. Fueron evaluados el Knee Society Score (KS y FS), el Oxford Knee Score (OKS) y el rango de movilidad (ROM), tanto preoperatorios, como postoperatorios tras 1, 5 y 10 años, así como la evolución radiográfica y las complicaciones.
ResultadosLos valores preoperatorios del KS, FS y OKS fueron inferiores en el grupo A (p<0,0001; p<0,01 y p<0,05, respectivamente), no así el ROM. Postoperatoriamente, KS, FS, OKS y ROM no fueron diferentes entre los grupos, ni al año, ni a los 5, ni a los 10 años. Tampoco hubo diferencias radiológicas ni de complicaciones entre ambos grupos.
DiscusiónLa utilización de implantes no constreñidos en los valgos graves no fue inferior a los varos leves, suponiendo, además, un ahorro anatómico para el paciente.
ConclusionesCorregir deformidades graves en valgo puede llevarse a cabo con implantes primarios no constreñidos, sin obtener por ello peores resultados a los obtenidos en deformidades leves.
In the knee, valgus deformities are considered such when they exceed 10° of the anatomical femoral-tibial angle, and comprise between 10% and 17% of all joint replacements performed, depending on the series.1,2 These deformities are anatomical variants that involve alterations at different planes in the joint, with increased flexion and external rotation.3 Secondly, this involves an increase in bone remodelling at the cost of hypoplasia of the lateral femoral condyle and the ipsilateral tibial plateau, on its posterior edge, and alteration of the soft tissues with increased tension in the lateral structures.1,3,4 Performing a joint replacement by means of a total knee arthroscopy (TKA) under these conditions poses a great challenge to orthopaedic surgeons, since achieving knee stability after correcting the deformity largely depends on the work on the soft tissues, which are altered around the joint.5
The challenges posed by correcting valgus deformities has resulted in leading authors on knee prosthetics to research and suggest different alternatives with regard to type of approach, type of implant or release of soft tissues to achieve the best result. Although there has been broad consensus as to the type of approach and soft tissue release in recent years without too much influence on the final clinical outcome of a joint replacement, there is still a difference of opinion amongst orthopaedic surgeons as to the choice of arthroplasty. Contradicting clinical outcomes are described. Thus, and for different reasons, increasingly more constrained implants have come into general use to the detriment of those that preserve more of the knee anatomy, with no evidence in this regard. This has resulted in endangering the future of these joints should rescue surgery be needed, since these implants require greater bone resection.4,6,7
The objective of this study was to compare the clinical and radiological results between a group of patients with severe knee valgus and a group with mild varus after both groups had undergone a minimally constrained TKA.
Material and methodEight hundred and seventeen primary TKAs performed between 1998 and 2006 were reviewed retrospectively. Their data were collected prospectively. Fifty TKAs performed on 49 patients (group A) were selected with a minimum deformity of 15° of valgus on the coronal plane of the anatomical femoral-tibial angle, including all the patients who exceeded this deformity in this period (Figs. 1–5). In parallel, a control group was selected with 50 TKAs performed on 45 patients (group B) during the same period but with a maximum deformity of 15° of varus on the coronal plane of the anatomical femoral-tibial angle. The patients in the control group were selected depending on how close their operation day was to that of each patient in group A, those operated on the same day were given priority, and one day before or one day after. Patients who did not complete the 10 year follow up, due to death or because they were lost to follow up, were not included in the study. The deformities were assessed on a standing anteroposterior teleradiograph. The femoral-tibial anatomical axis was measured on teleradiographs, starting from the femur from the most proximal part of the trochanter to the centre of the intercondylar notch in the femur and from the centre of the tibial plateau between both spines, to the centre of the tibial pilon. All the operations were undertaken by the same senior orthopaedic surgeon (JGB). Both groups were paired by age, sex, BMI and follow-up time, which was determined at a minimum of 10 years. The NexGen Legacy Posterior-Stabilised prosthesis (PS) (Zimmer Warsaw-Biomet, IN) was used in all cases. The patients were tested preoperatively and postoperatively at one year and subsequently every 2 years until the seventh year, when they started 3-year follow-ups. The data obtained preoperatively and postoperatively at one year, 5 years and 10 years were selected. Patients who did not complete the follow-up were rejected, the final number of patients included in the study was 41 (41 cases of TKA) in group A and 42 (44 cases of TKA) in group B.
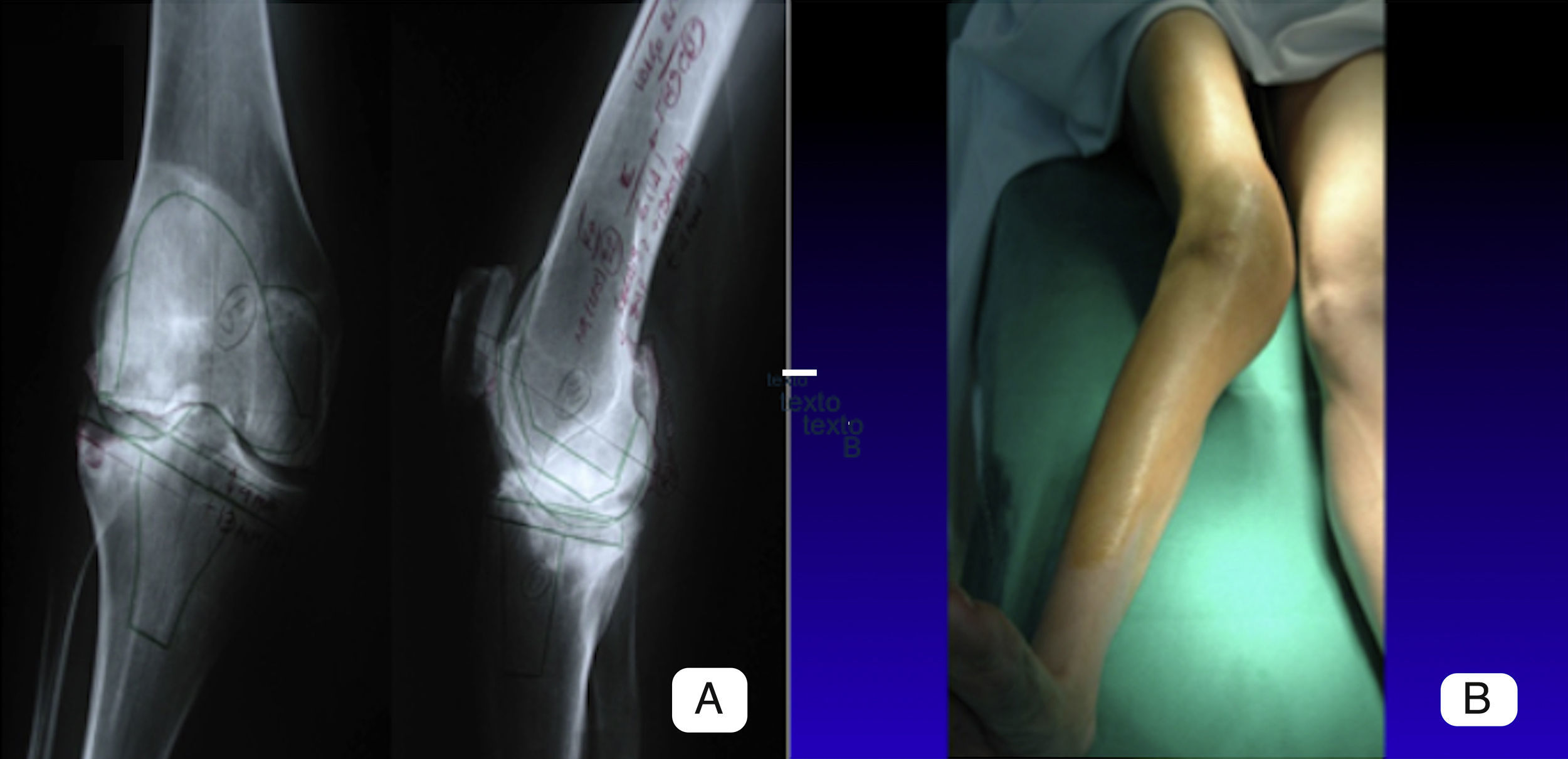
Preoperative images of a patient with a valgus deformity of 23°. (A) We can see the preoperative planning in the image with the X-rays taken in the anteroposterior and lateral planes over which the cuts and resection angles have been drawn. (B) The image shows the appearance of the limb prior to surgery.
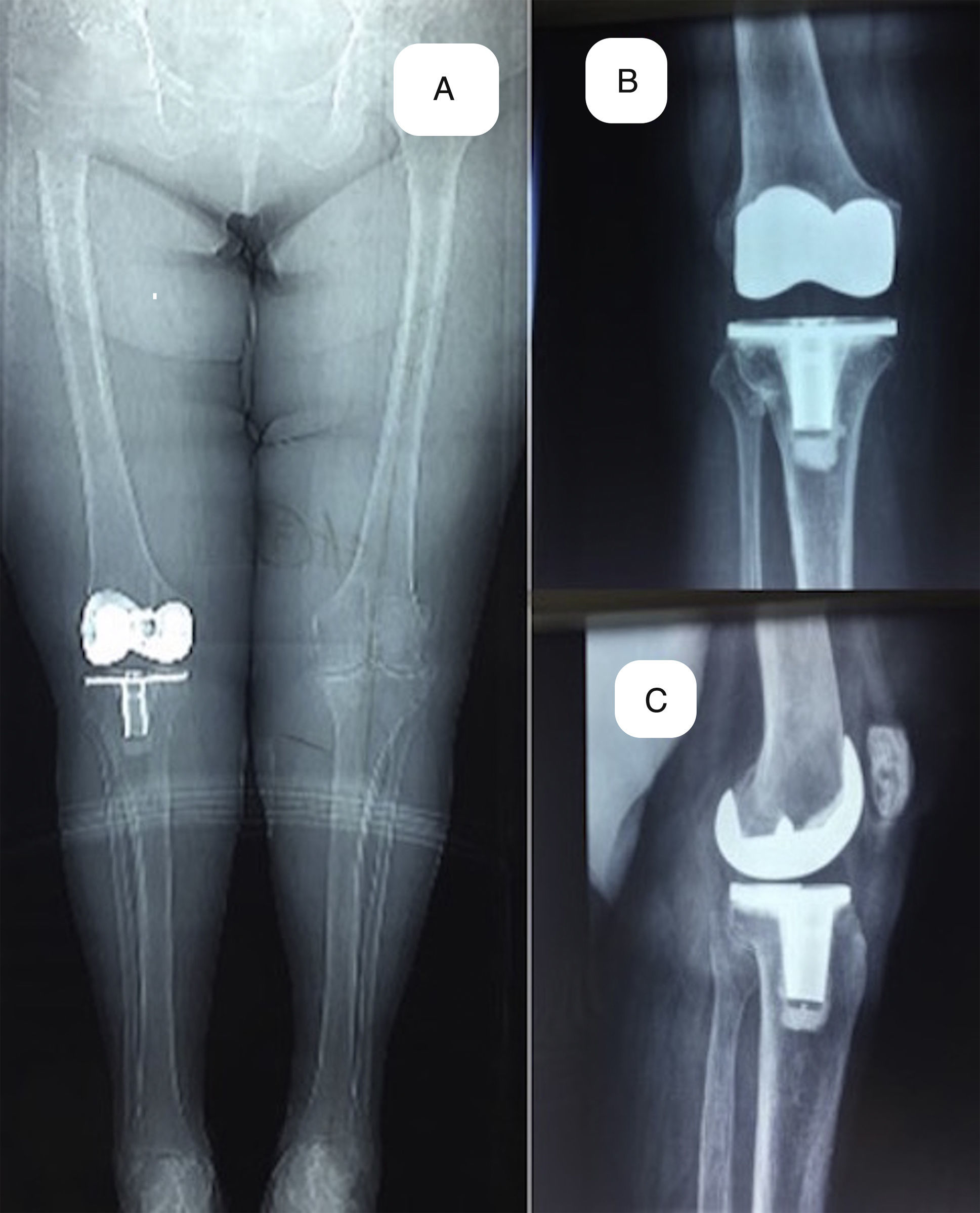
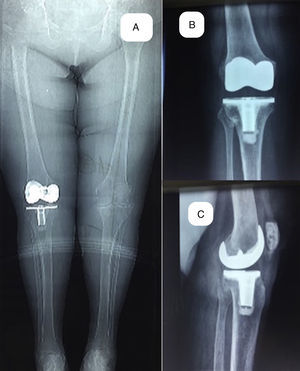
Postoperative images of the patient shown in Fig. 1A after 10 years. Teleradiography of lower limbs, weight-bearing, with valgus alignment of 6°. (B) Weight- bearing X-ray on anteroposterior plane. (C) Weight-bearing X-ray on lateral plane.
Postoperative images at 10 years of the patient shown in Figs. 1 and 2. (A) Standing anteroposterior view of both limbs. (B) Lateral view in 45° hip flexion and maximum knee extension at 0°. (C) Lateral view 125° knee flexion.
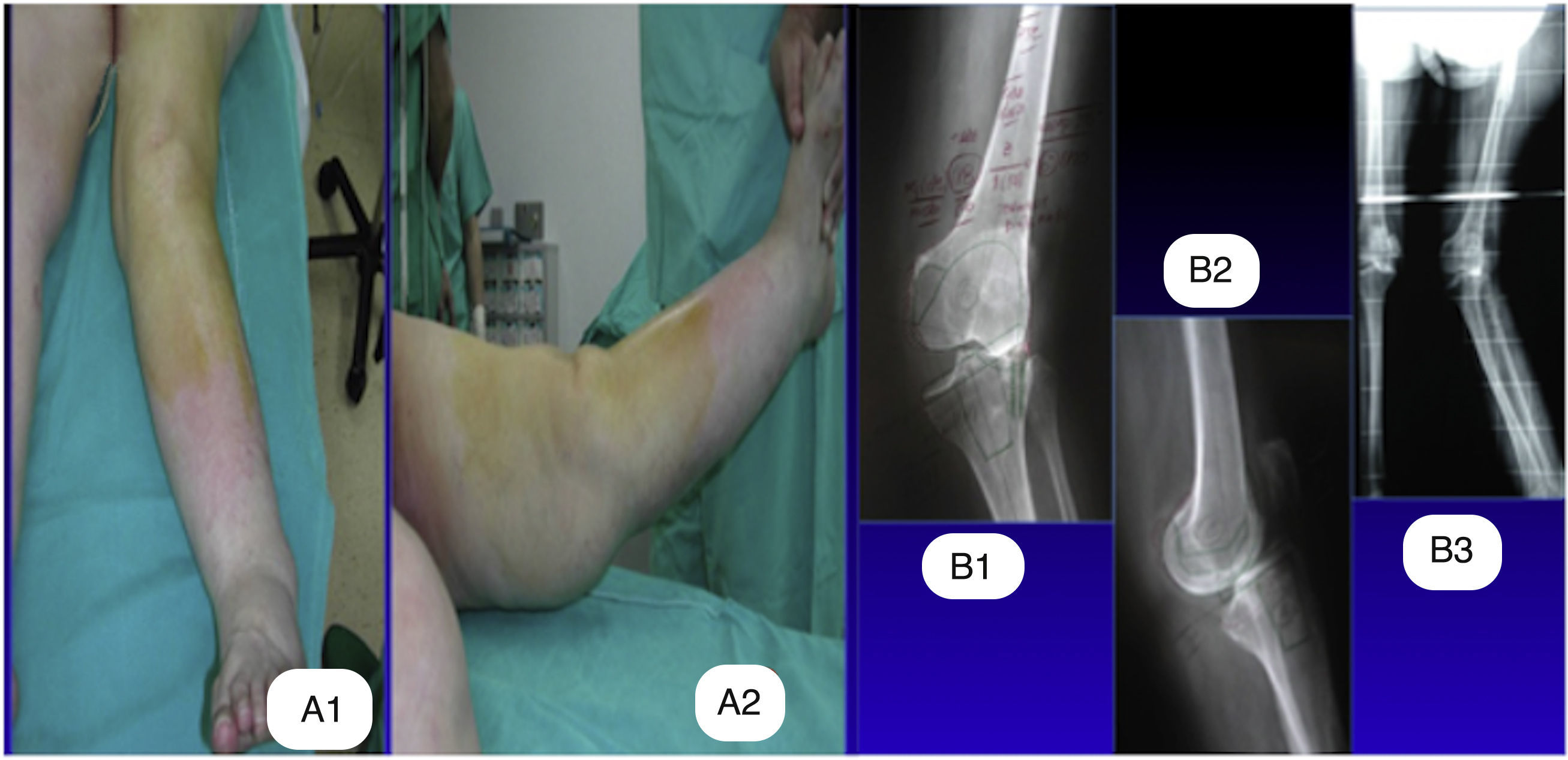
(A) Preoperative images of a case with 27° valgus taken in the anteroposterior plane and recurvatum of 10° in the lateral plane, associated with severe instability on both planes. (B) Preoperative X-rays taken in the anteroposterior and lateral planes, and teleradiography of both lower limbs, with presurgical planning.
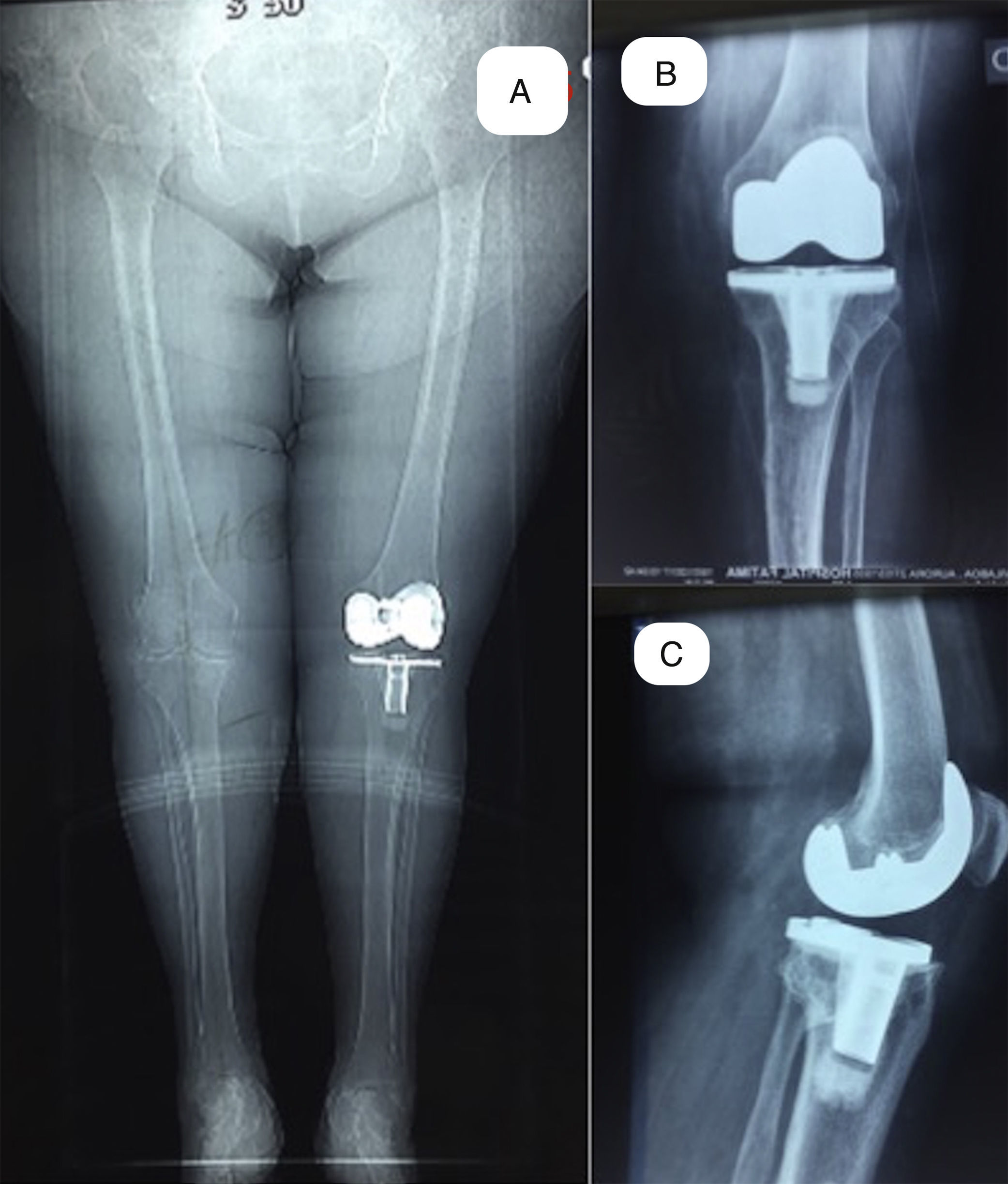
Postoperative images of the patient of Fig. 4 at 12 years after surgery. (A) Teleradiography of weight bearing lower limbs with a valgus alignment of 6°. (B) Weight-bearing X-ray, anteroposterior plane. (C) Weight-bearing X-ray, in the lateral plane.
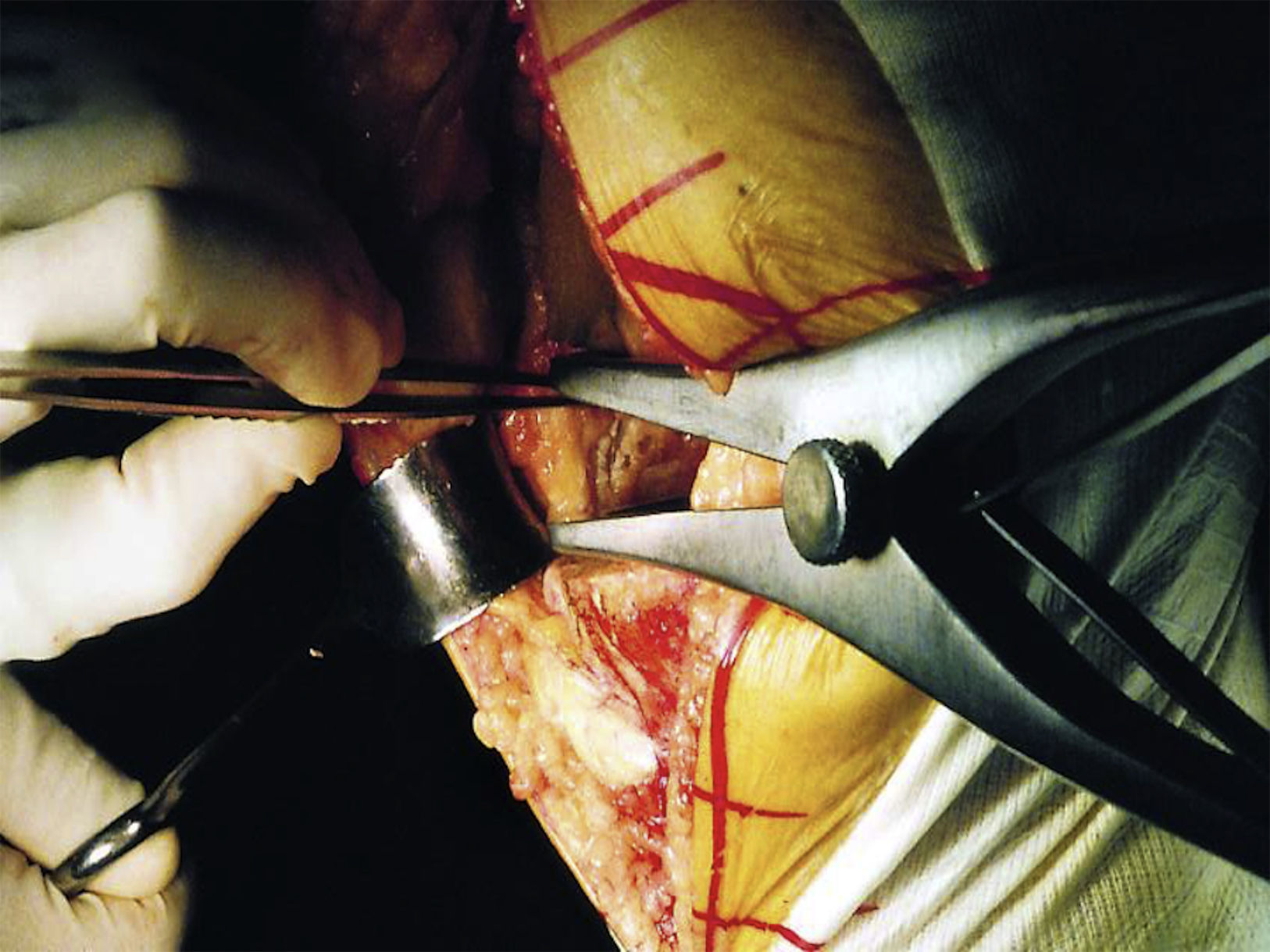
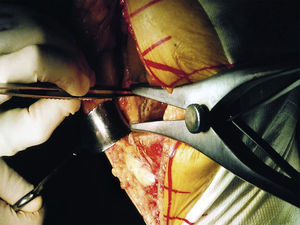
An ischaemia cuff was used in all the operations throughout each intervention, which was released after closure, and when the limb was bandaged. All the TKAs were performed using a medial parapatellar approach. All the arthroplasties were cemented, in both their tibial and femoral component. Soft-tissue release in the valgus deformities (group A) was performed using the pie crust technique8 performed in knee extension using a lamina spreader and stability was checked on each release, both in flexion and extension with the help of the specific gaps (Fig. 6). The release sequence was started at the level of the tibial cut with a surgical scalpel blade No. 15, making transversal cuts over the posterior capsule, protecting the popliteal muscle tendon and continuing up to the iliotibial band. In the cases where visualisation of the posterior capsule was not clear, release started at the iliotibial band. Only when necessary was the lateral collateral ligament released using the same technique. The release was performed until symmetric stability was achieved on flexion and extension. In the cases where there was residual instability on flexion an additional femoral resection was performed. All the patellae were fitted with a cemented polyethylene implant. Patellar tracking was checked with the test implants. If it was incompetent the lateral retinaculum was partially released without completing its thickness. The patients were assessed using the Knee Society Score, divided into Knee Score (KS) and Functional Score (FS),9 each over 100 points. The Oxford Knee Score (OKS)10 was used over 50 points. Joint movement was assessed using a manual goniometer (ROM). These data were gathered by the same investigator (JGB). The patients started early mobilisation 12h after the intervention with exercises assisted by an isokinetic machine. Partial weight bearing with crutches was commenced after 24h, removing one crutch a week later and the other after 3 weeks. The patients were fully weight-bearing after 3 weeks. Pre and postoperative X-rays were studied by the same investigator (XPC), using the Knee Society Roentgenographic Scoring System, evaluating any radiolucent lines, their progression and clinical repercussions.11
Statistical analysisInitially a descriptive analysis was undertaken where the qualitative variables were expressed as frequency and percentage. The continuous variables were expressed as mean±standard deviation, and median (minimum–maximum). Parametric/non-parametric tests were performed to determine the potential association between the study variables (chi-square test, Fisher's exact test, Student's t-test, Mann–Whitney U test). Wilcoxon's test was used to study clinical evolution in the tests and flexion. In all the analyses differences with a p value<0.05 were considered statistically significant. SPSS 15.0, Epidat 4.1 and free R software (http://www.r-project.org) were used for the analyses.
Ethical aspectsThe research undertaken met the fundamental principles established in the Declaration of Helsinki in the Council of European Convention on Human Rights and Biomedicine, and the requirements set out in Spanish legislation in the area of biomedical research, the personal data protection and bioethics. The study was approved by the Area Clinical Research Ethics Committee on 29 September 2016 with Registration Code: 2016/310.
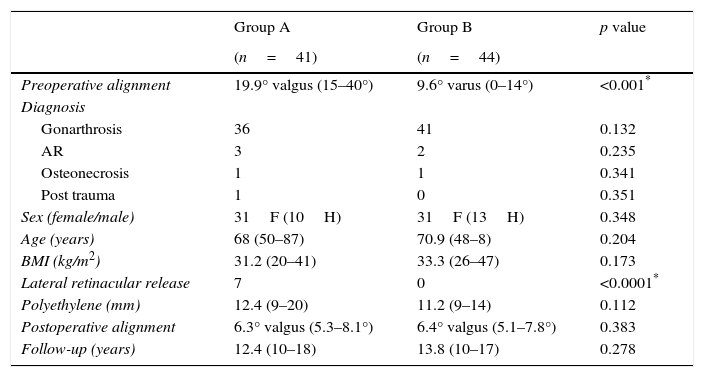
ResultsBoth groups (A and B) were comparable in terms of age, sex, BMI and preoperative diagnosis (Table 1).
Comparative descriptive data between both samples.
| Group A | Group B | p value | |
|---|---|---|---|
| (n=41) | (n=44) | ||
| Preoperative alignment | 19.9° valgus (15–40°) | 9.6° varus (0–14°) | <0.001* |
| Diagnosis | |||
| Gonarthrosis | 36 | 41 | 0.132 |
| AR | 3 | 2 | 0.235 |
| Osteonecrosis | 1 | 1 | 0.341 |
| Post trauma | 1 | 0 | 0.351 |
| Sex (female/male) | 31F (10H) | 31F (13H) | 0.348 |
| Age (years) | 68 (50–87) | 70.9 (48–8) | 0.204 |
| BMI (kg/m2) | 31.2 (20–41) | 33.3 (26–47) | 0.173 |
| Lateral retinacular release | 7 | 0 | <0.0001* |
| Polyethylene (mm) | 12.4 (9–20) | 11.2 (9–14) | 0.112 |
| Postoperative alignment | 6.3° valgus (5.3–8.1°) | 6.4° valgus (5.1–7.8°) | 0.383 |
| Follow-up (years) | 12.4 (10–18) | 13.8 (10–17) | 0.278 |
BMI, body mass index.
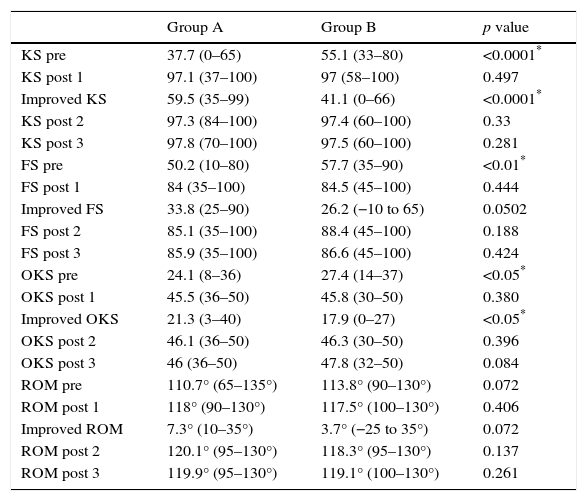
The preoperative differences between groups A and B in the KS, FS and OKS were statistically significant (p<0.0001, p<0.01 and p<0.05), with lower values in group A. There were also statistically significant differences in favour of group A in improved KSS between the preoperative check and postoperative follow-up at one year after surgery (p<0.0001), and in improved OKS (p<0.05). In the remaining comparisons the results were not statistically significant (Table 2).
Comparative clinical results between both groups.
| Group A | Group B | p value | |
|---|---|---|---|
| KS pre | 37.7 (0–65) | 55.1 (33–80) | <0.0001* |
| KS post 1 | 97.1 (37–100) | 97 (58–100) | 0.497 |
| Improved KS | 59.5 (35–99) | 41.1 (0–66) | <0.0001* |
| KS post 2 | 97.3 (84–100) | 97.4 (60–100) | 0.33 |
| KS post 3 | 97.8 (70–100) | 97.5 (60–100) | 0.281 |
| FS pre | 50.2 (10–80) | 57.7 (35–90) | <0.01* |
| FS post 1 | 84 (35–100) | 84.5 (45–100) | 0.444 |
| Improved FS | 33.8 (25–90) | 26.2 (−10 to 65) | 0.0502 |
| FS post 2 | 85.1 (35–100) | 88.4 (45–100) | 0.188 |
| FS post 3 | 85.9 (35–100) | 86.6 (45–100) | 0.424 |
| OKS pre | 24.1 (8–36) | 27.4 (14–37) | <0.05* |
| OKS post 1 | 45.5 (36–50) | 45.8 (30–50) | 0.380 |
| Improved OKS | 21.3 (3–40) | 17.9 (0–27) | <0.05* |
| OKS post 2 | 46.1 (36–50) | 46.3 (30–50) | 0.396 |
| OKS post 3 | 46 (36–50) | 47.8 (32–50) | 0.084 |
| ROM pre | 110.7° (65–135°) | 113.8° (90–130°) | 0.072 |
| ROM post 1 | 118° (90–130°) | 117.5° (100–130°) | 0.406 |
| Improved ROM | 7.3° (10–35°) | 3.7° (−25 to 35°) | 0.072 |
| ROM post 2 | 120.1° (95–130°) | 118.3° (95–130°) | 0.137 |
| ROM post 3 | 119.9° (95–130°) | 119.1° (100–130°) | 0.261 |
KSS, FSS and OKS scores, ROM scores in degrees.
FS, functional score system; KS, knee score system; Improved, difference between preoperative check and follow-up at one year after the surgery; OKS, Oxford knee system; Pre, preoperative check; post 1, follow-up at one year after surgery; ROM, range of movement (ROM); post 2, follow-up at 5 years after surgery; post 3, follow-up at 10 years after surgery.
There were visible tibial radiolucent lines on the post-operative X-rays in 5 cases in group A, none were progressive and none involved complications. In group B there were 4 cases of non-progressive tibial radiolucent lines, 3 femoral radiolucent lines that were not progressive either, and one more with femoral and tibial lines, none with observable clinical impact.
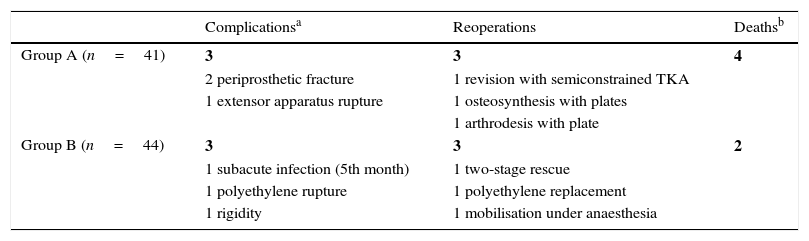
The complications in group A were 2 supracondylar periprosthetic fractures after 2 accidental falls. One was resolved by osteosynthesis with plate and screws, and the other required rescue surgery with change of the femoral component for a semi-constrained model (LCCK, Zimmer Warsaw-Biomet, IN). In addition, a third case, after another fall, suffered a knee extensor apparatus rupture and had to be rescued with an arthrodesis with two plates. There were no complications associated with the joint replacement surgery, and no infections or loosening. One case in Group B suffered a subacute infection 5 months after the primary surgery and required two-stage prosthetic exchange surgery. A second case underwent a rupture of the polyethylene insert that was changed with no subsequent complications. And finally, there was one case of postoperative rigidity which required mobilisation under anaesthesia. There were no peroneal nerve injuries in either of the 2 groups (Table 3).
Postoperative complications.
| Complicationsa | Reoperations | Deathsb | |
|---|---|---|---|
| Group A (n=41) | 3 | 3 | 4 |
| 2 periprosthetic fracture | 1 revision with semiconstrained TKA | ||
| 1 extensor apparatus rupture | 1 osteosynthesis with plates | ||
| 1 arthrodesis with plate | |||
| Group B (n=44) | 3 | 3 | 2 |
| 1 subacute infection (5th month) | 1 two-stage rescue | ||
| 1 polyethylene rupture | 1 polyethylene replacement | ||
| 1 rigidity | 1 mobilisation under anaesthesia |
Four patients died in group A after 10 years’ follow-up, due to causes unrelated to the joint surgery (2 acute lung failures, one AMI and one acute renal failure). Two patients in group B died after 10 years’ follow-up again due to causes unrelated to the surgery (one AMI and one acute lung failure) (Table 3).
DiscussionOur results support the use of minimally constrained primary implants in large valgus deformities since, based on the statistically significant preoperative differences in KS, FS and OKS (p<0.0001; p<0.01 and p<0.05, respectively) between both groups, after surgery with the same PS implant, the post-operative outcomes were no different, from the first to the tenth year.
Correction of a knee joint valgus deformity has been considered a challenge in the history of orthopaedic surgery. There has been intense debate as to the type of ligament balancing, approach and choice of appropriate implant. Yet the advances in these terrains have not been contrasted due to a lack of scientific evidence-based studies. However, the publication of leading orthopaedic surgeons’ experience has guided surgical practice in the challenges posed in correcting these deformities. The published series show us clinical improvement comparable with that obtained in varus deformities, even though these are theoretically less demanding surgically. The results we obtained in this study follow the same lines.
Our experience with the anteromedial approach has lead us to choose it over the anterolateral approach proposed by Keblish.12 Previous series have shown good clinical results with few complications using the anteromedial approach.1,3,8 Likewise, we prefer the pie crust lateral release technique, which has been endorsed by large series.1,9,13 Similarly, many authors choose to tighten the medial collateral ligament, due to its laxity in severe valgus. However in our experience this was not necessary in any of our cases after checking mediolateral stability at each stage of progressive lateral release. By checking this we did not have to opt for an LCCK implant in any of the more severe cases (which was always ready and prepared for use).
Selection of the appropriate implant appears to us to be most relevant, since the outcome of the arthroplasty can depend on this. PS implants provide some advantages over CR implants in correcting valgus deformities, since, as has been published previously, the posterior cruciate ligament (PCL) is at great risk of damage in these deformities, its tension can be altered, which would make any angular correction difficult.14,15 The PS implant enables us to lateralise both components to a greater extent, and thus achieve better patellar tracking and therefore avoid lateral retinacular release.1,6
However, in our opinion, the most decisive point in the outcome of a joint replacement in valgus deformity is the choice of degree of constriction of the arthroplasty. In this regard, and as previously highlighted by major authors,4,6,7 the current trend is for orthopaedic surgeons increasingly to constrain implants in severe valgus deformities. The reason for this is the need for extensive lateral releases, which results in a theoretical residual instability which is difficult to correct with a primary TKA.1 However, some experts have warned of the use of these more constrained prostheses.4,6 Pang et al.16 published a series of cases comparing 50 unconstrained TKAs with 50 constrained TKAs, and found statistically significant differences with regard to an increased joint space, greater in the constrained TKAs, and with regard to FS at 2 years, better in the unconstrained TKAs. Anderson et al.17 previously published their series of cases with 70 constrained TKAs, obtaining excellent clinical improvement, but without comparing these results with primary TKAs and with scant follow-up of less than a mean 4 years.
With the choice of a primary unconstrained implant, we managed to achieve a major saving in bone stock, thus avoiding possible contingencies in subsequent arthroplasty revisions, reserving the more constrained implants, LCCK, for rescue surgery if necessary. This was corroborated in our study on one occasion only, since in the one revision surgery carried out in group A, after a periprosthetic fracture, we used LCCK prosthesis. This which was possible because we had not used this implant in the primary surgery.
Furthermore, choosing an unconstrained implant in our opinion limits the perioperative risks for the patient. This is due to the smaller bone resection, with consequent reduction in blood loss and surgery time. We were able to confirm this because the size of the polyethylene used was similar in both groups (12.4mm in group A, 11.2mm in group B). Moreover, the increased intramedullary material with the use of stems increases the risk of periprosthetic fracture. We should also highlight the financial savings when primary implants are used compared to constrained implants, as mentioned by Pang et al. and Anderson et al.16,17 Our results endorse this choice, which preserves the patient's anatomy better although is more demanding from the surgeon's perspective, not only because it is up to them to perform a thorough lateral soft tissue release but also because preoperative planning must be scrupulous. This is where we believe a great part of success lies when a primary implant is used in a valgus deformity. Planning all the TKAs beforehand enabled us to predict the most suitable implant for each case, know the levels of bone resection and what the soft tissues required before entering the operating theatre.
The pie crust technique proposed by Ranawat et al.,1 and subsequently adapted by Clarke et al.,10 has been shown to be very useful. However, we are aware of how difficult it is and the learning curve required. Therefore wide practice on cadavers is recommended before undertaking the technique to gain an in-depth knowledge of the lateral anatomy of the knee. The absence of peroneal nerve injury, described previously at between 0.3% and 9.5%,6 was possible using the safe zone suggested by Bruzzone et al.,13 preferably over the iliotibial band, and avoiding as far as possible the danger zone between the popliteus tendon, the posterolateral capsule and the posterior fibres of the iliotibial band.
Overall complications were similar in both groups, with one revision procedure per group. However, those caused by the surgery itself were greater in group B, since in group A the complications were caused by accidental falls, whereas the 3 complications in group B could be put down to the primary surgery itself (infection, polyethylene rupture and rigidity). The radiolucent lines were comparable between both groups (5 in A and 8 in B). They were not progressive in any case.
Our data are comparable and even improve on those of other large series, such as that of Ranawat et al.,1 who presented a series of 42 knees with a femoral tibial deformity greater than 10°. Their knees improved on the clinical and functional score by 63 and 47 points respectively with a post-surgical flexion of 110°, and only 3 revisions, with a minimum follow-up of 5 years. Stern et al.18 published a series with134 cases with a femoral/tibial deformity greater than 10° (118 of them PS, 12 constrained and 4 CR) and with 4.5 years’ follow-up, where the clinical improvement of KSS was 37 points, with 4 revisions. Miyasaka et al.3 presented 60 knees with a femoral/tibial deformity greater than 10°, in a minimum of 10 years’ follow-up, with clinical improvement on the KSS of 60 points and functional improvement of 39 points, final flexion was 98°.
The weaknesses of our study were the retrospective data gathering and the lack of pre- and postoperative radiological analysis including data of patellar height and joint space. By contrast, we believe that the strengths are the minimum 10 years’ follow-up, and the fact that all the interventions were performed by the same surgeon and under very similar circumstances.
Therefore, given the results we obtained in this study, which were comparable with the most extensive series published to date, with long-term follow-up, we believe that primary TKA PS implants can be used to correct large valgus deformities without having to resort to constrained implants. This makes methodical lateral release and detailed preoperative planning necessary to anticipate and plan for intraoperative contingencies. Moreover, the savings for the patient, with regard to their own anatomy, which we must preserve in anticipation of possible rescue surgery, should be sufficient argument in itself to opt for a primary implant for a valgus deformity.
Level of evidenceLevel of evidence III.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that neither human nor animal testing have been carried out under this research.
Confidentiality of dataThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
Conflict of interestThe authors have no conflict of interests to declare.
Our most sincere thanks go to Mar, for her daily effort and dedication, without which neither this nor other studies would have been possible.
Please cite this article as: Paredes-Carnero X, Fernández-Cortiñas AB, Escobar J, Galdo JM, Babé JG. Tratamiento de valgos severos de rodilla mediante artroplastia total no constreñida: estudio comparativo con seguimiento a largo plazo. Rev Esp Cir Ortop Traumatol. 2017;61:240–248.