Charcot-Marie-Tooth disease (CMT) is a hereditary motor sensory neuropathy that frequently results in a cavovarus foot in the adult. Surgical treatment allows correction of the deformity while preserving an adequate range of motion.
ObjectiveThe objective of this study was to assess the result of posterior tibial tendon transfer, first metatarsal ascent osteotomy, and calcaneal valgus osteotomy in the treatment of cavovarus foot secondary to CMT.
Material and methodsRetrospective cohort of CMT patients who received surgical treatment of their cavovarus foot. Collected data included demographics, CMT genetic variant, neurologic involvement, surgical technique, range of motion, functionality, radiology, and postoperative satisfaction.
Results16 patients met the inclusion criteria, mostly women (62.5%) with the CMT1A variant (62.5%), and a mean age of 39.5 years. 13 patients required additional surgical techniques: lengthening of the Achilles tendon, interphalangeal arthrodesis and/or plantar fascia section. 2 patients underwent a secondary procedure: subtalar arthrodesis due to persistence of the varus deformity, and a lengthening of the extensor hallux longus due to initial undercorrection. The mean follow-up was 42 months. Significant differences (P = .003) were observed between the pre-surgical AOFAS and at 12 months postoperatively (37.25 vs. 86.5). 75% of the patients reported “excellent” or “good” satisfaction after surgery. All radiographic parameters showed significant improvement.
ConclusionsThe combination of the aforementioned surgical techniques for the cavovarus foot in CMT results in adequate functionality, good radiological correction and a high degree of satisfaction, avoiding primary arthrodescent surgery.
La enfermedad de Charcot-Marie-Tooth (CMT) es una neuropatía sensitivomotora hereditaria que suele llevar a un pie cavo-varo en el adulto. El tratamiento quirúrgico en estos pacientes busca corregir la deformidad preservando un adecuado rango de movilidad.
ObjetivoEl objetivo de este estudio fue valorar el resultado de la transferencia del tendón tibial posterior, la osteotomía de ascenso del primer metatarsiano y la ostetomía valguizante de calcáneo en el tratamiento del pie cavo-varo secundario a CMT.
Material y métodosCohorte retrospectiva de pacientes con CMT sometidos a cirugía correctora de su pie cavo-varo. Se recogieron datos demográficos, variante genética de CMT, afectación neurológica, técnica quirúrgica, rango de movilidad, funcionalidad, valoración radiológica, y satisfacción postquirúrgica.
Resultados16 pacientes cumplieron los criterios de inclusión, la mayoría mujeres (62.5%) con patrón CMT1A (62.5%), y edad media de 39.5 años. En 13 pacientes se necesitaron gestos quirúrgico adicionales: alargamiento del tendón de Aquiles, artrodesis interfalángica y/o sección fascia plantar. Dos pacientes fueron reintervenidos: artrodesis subtalar por persistencia de varo, alargamiento del extensor largo del hallux por hipocorrección inicial. El seguimiento medio fue de 42 meses. Se observaron diferencias significativas (P = .003) entre el AOFAS prequirúrgico y a los 12 meses postquirúrgicos (37.25 vs. 86.5). El 75% de los pacientes refirió una satisfacción “excelente” o “buena” tras la cirugía. Todos los parámetros radiográficos presentaron mejoría significativa.
ConclusionesEl manejo quirúrgico del pie cavo-varo en el CMT mediante la combinación de las técnicas descritas presenta una adecuada funcionalidad, buena corrección radiológica y alto grado de satisfacción, evitando la cirugía artrodesante de entrada.
Charcot-Marie-Tooth disease (CMT), also called hereditary sensorimotor neuropathy, is a heterogeneous group of peripheral neuropathies with an incidence worldwide of 15.2–40/100,000, around 28.2/100,000 in Spain.1 It is characterised by demyelination and/or axonal degeneration of the peripheral nerves, and its clinical onset is typically in the first two decades of life.2,3
Clinical examination and neurological assessment show the trophic muscle changes and muscle imbalance typical of CMT patients. The confirmatory diagnosis begins with an electromyogram, but the definite diagnosis is obtained by molecular analysis that categorises the disease into one of several genetic patterns.4 Eighty causative genes have been identified,4 although CMT type 1A is the most common subtype in our region, with a prevalence of 62.8% of diagnosed cases.1 Approximately 90% of patients with CMT have pes cavus and the prevalence of the disease is 78% in subjects with bilateral pes cavus.5
In the literature1,4 36 loci in 30 cloned genes have been identified for CMT. CMT is classified at the clinical genetic level as follows1:
- •
CMT 1: Demyelinating phenotypes with autosomal dominant (AD) inheritance.
- •
CMT 2: Neuronal or axonal with AD or autosomal recessive (AR) inheritance.
- •
CMT 4: Demyelinating phenotypes like 1 but AR with severe forms.
- •
CMTX1: Intermediate demyelinating/axonal sex-linked form.
The deformity present in these pes cavus is the result of an imbalance between agonists and antagonists, but also due the action of other muscles recruited to compensate for the loss of function. Plantar flexion of the first metatarsal (M1) is the first and most characteristic change in the geometry of CMT cavus foot. This change is due to loss of strength of the tibialis anterior muscle, which does not compensate for the tone of the lateral peroneus longus muscle. Later, the strength of the peroneus brevis muscle is also reduced and its weakness relative to the tibialis posterior leads to increased midfoot supination and varus hindfoot. Fibrosis and shortening of the plantar fascia contribute to an increased plantar arch.6 Finally, recruitment of the extensor hallucis longus and extensor digitorum longus, which function as accessory dorsiflexors, attempting to compensate for the weakness of the tibialis anterior muscle, leads to the development of forefoot deformities such as clawing of the hallux and lesser toes. Clinically, patients may present with lateral ankle instability, hyperkeratosis under the metatarsal heads, metatarsalgia, problems with footwear and clearly impaired gait.7
The aim of surgical treatment is to obtain a plantigrade foot.8 In the presence of a flexible foot and the absence of degenerative signs, it is desirable to preserve as much of the range of motion of both foot and ankle as possible. In these cases, it is usually sufficient to correct plantar flexion of the first metatarsal and perform a tendon transfer to restore the lost muscle balance.9
Concerns arise when the hindfoot is clearly not flexible. In these feet, sufficient correction of hindfoot varus is not achieved with the isolated elevation of M1. In the scientific literature, there are two schools of thought,9 where the fundamental difference is how to correct the hindfoot in these cases. One school of thought, with which the authors agree, considers that performing an extra-articular calcaneal osteotomy, together with tendon transfers, is sufficient to correct and stabilise the hindfoot, while the other school advocates early triple arthrodesis. We believe that the addition of a calcaneal valgus osteotomy (Dwyer-type osteotomy),10 with or without lateral displacement, is very useful for stabilising the foot in an appropriate position without the need for arthrodesis, provided there is no joint degeneration.
Therefore, the aim of this study is to present the outcome of surgical treatment of cavovarus foot secondary to CMT, flexible or otherwise, without joint degeneration, using a combination of non-arthrodesis techniques: M1 ascent osteotomy, posterior tibial transfer, and calcaneal valgus osteotomy. Our hypothesis is that these three techniques act in a global manner and achieve optimal and sustained correction of the patient's deformity.
Material and methodsWe undertook a retrospective review of all patients in our centre affected by CMT with cavovarus foot with surgical indication from 2007 to 2019. The inclusion criteria were no previous surgeries, uncontrolled symptoms with conservative treatment for at least one year, no disease other than CMT that could alter gait and no degenerative changes in the joints of the foot (diagnosed by previous clinical and radiographic controls). From an initial cohort of 38 patients, we selected those who had undergone the three surgical procedures we analysed in our study: posterior tibial tendon transfer, ascending osteotomy of the first metatarsal and calcaneal valgus osteotomy.
The patient with CMT was diagnosed by full neurological and clinical assessment and diagnosis was confirmed by genetic pattern analysis. All the subjects gave their consent for inclusion in the study.
Demographic data such as age, sex, laterality, and the genetic pattern of the disease were collected. In the physical examination, the strength of the different muscle groups of the affected limb (Medical Research Council scale),11 type of gait, impaired myotendinous reflexes and distal sensitivity were noted.
In the examination of the foot and ankle, the plantar footprint and support points, plantar flexion of the first radius and heel varus were analysed. The stiffness of the deformity was assessed using Coleman’s test.12
All the patients were followed up clinically and radiographically one, three, six and twelve months following surgery and then once a year.
The degree of function was assessed using the AOFAS rating system13 questionnaire for the hindfoot before surgery and at 12-months follow-up. Results were classified as excellent (100–90 points), good (89–75 points), fair (74–50 points) or poor (<50 points). Subjective improvement was recorded at one year using a categorical scale with five levels of satisfaction (very dissatisfied, dissatisfied, indifferent, satisfied and very satisfied).
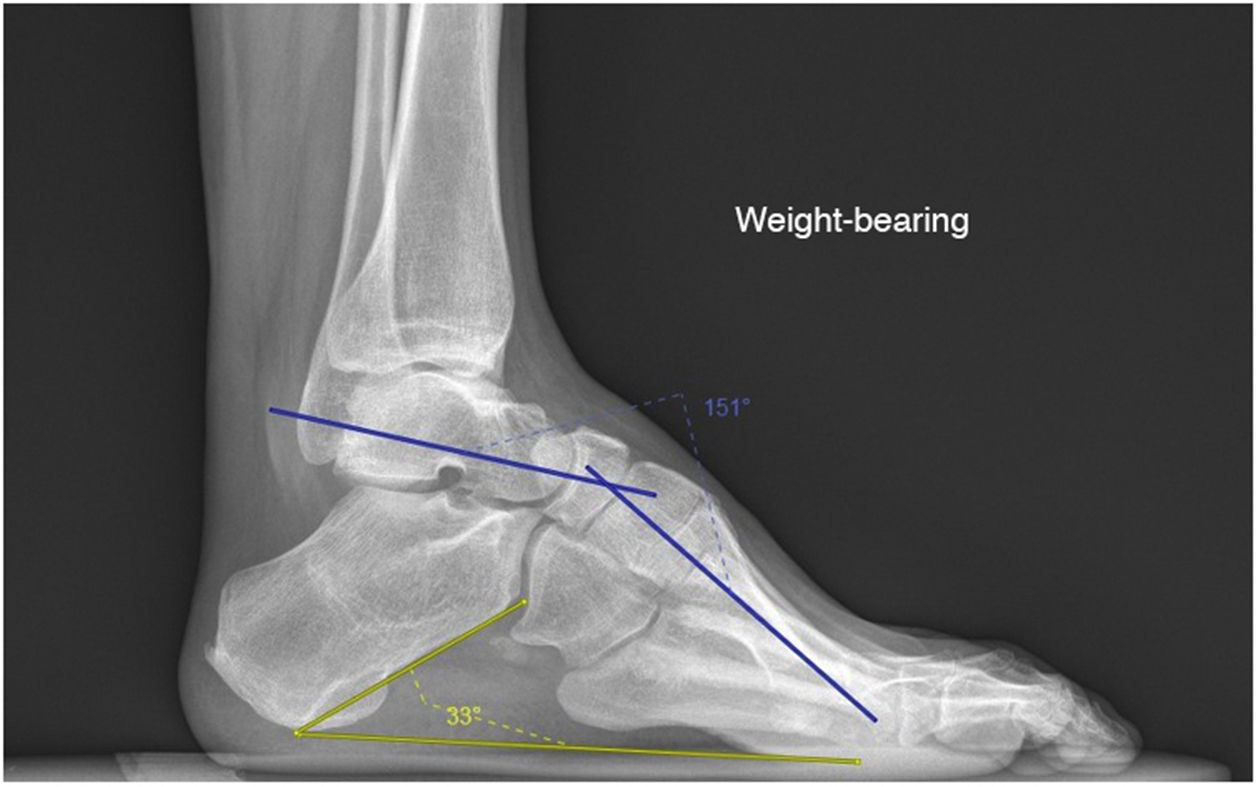
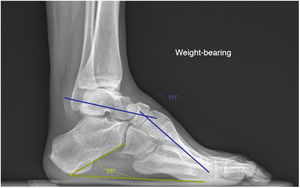
Two radiological parameters were assessed, both in the pre-surgical period and one year after surgery. Meary’s angles and the calcaneal inclination were measured in the lateral projection of plain radiographs of both weight-bearing feet and ankles (Fig. 1). Meary’s angle, between the long axis of the talus and the axis of M1, is a measure of the overall deformity of the foot, pes cavus appearing if it is >4°. If the values are <15° it is considered mild, between 15° to 30° moderate, and severe if >30°.14 The calcaneal inclination is the angle between the horizontal and a line from the base of the heel to the inferior cortex of the calcaneus, measuring the amount of cavus deformity that depends on the hindfoot, with normal values between 15° to 20°.15
Finally, complications occurring in the postoperative period and during follow-up were reviewed.
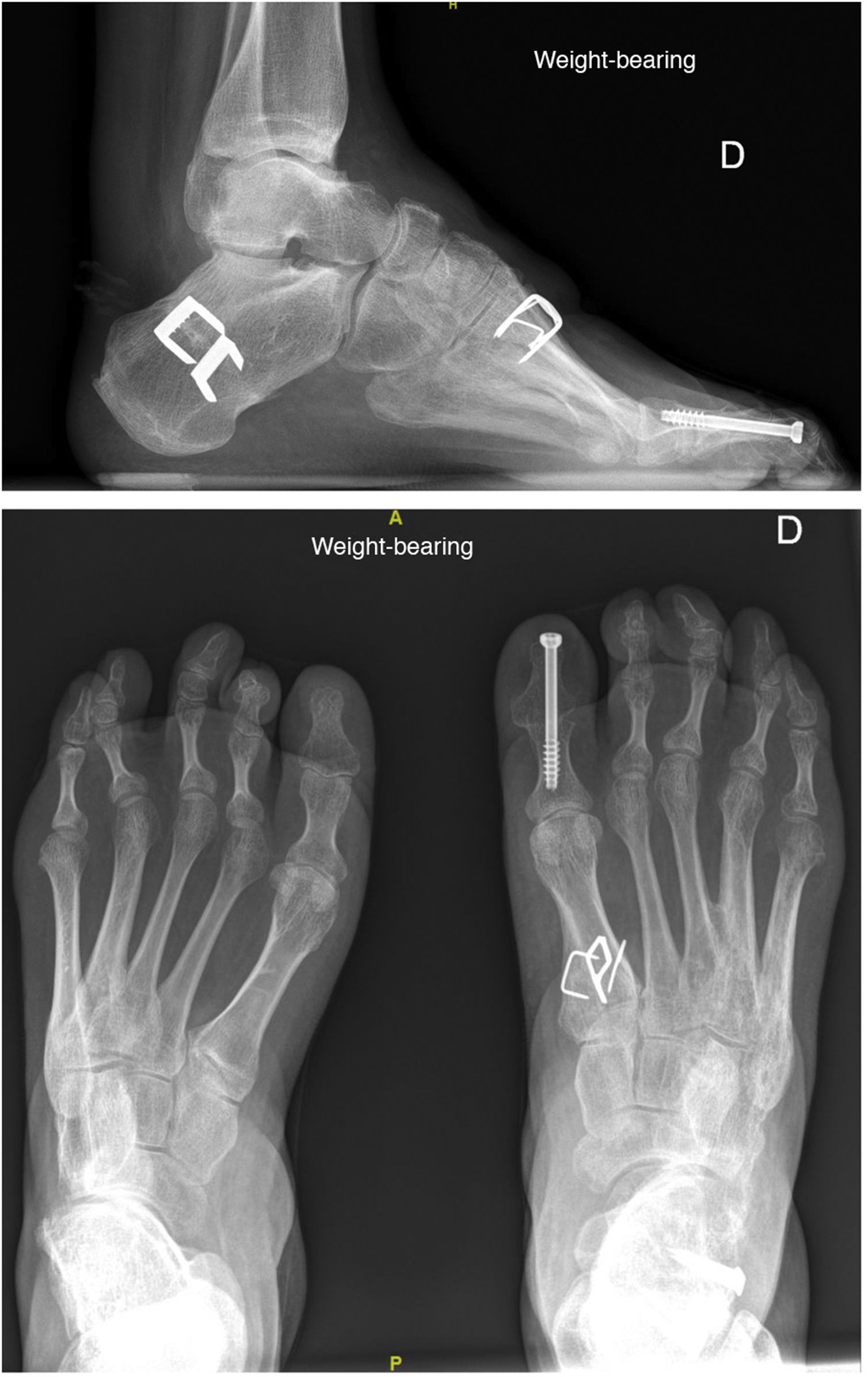
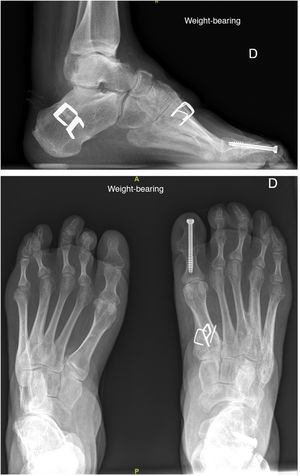
As mentioned above, in all cases, surgery consisted of a first metatarsal ascent osteotomy associated with transfer of the posterior tibial tendon to the dorsum of the foot (2 or 3 wedges) and a calcaneal valgus osteotomy. In some patients, other surgical procedures were associated such as lengthening of the Achilles tendon (percutaneous tenotomy), section of the plantar fascia and short musculature of the foot (Steindler procedure),16 and interphalangeal arthrodesis of hallux or toe clawing (Fig. 2).
All statistical analyses were performed using the free software R Commander 3.4.3.
The analytical study of the quantitative parameters was performed using non-parametric tests, as the cohort had a small sample size and when the pre-surgical parameters were assessed using the Shapiro–Wilk normality test and the Lilliefors test (Kolmogorov–Smirnov) in both cases the result was significant (P < .05), therefore it was not possible to obtain an adequate normal distribution of the sample.
The Mann–Whitney U test was used for the analytical study of the quantitative data. Differences in the statistical results were considered significant for P values <.05.
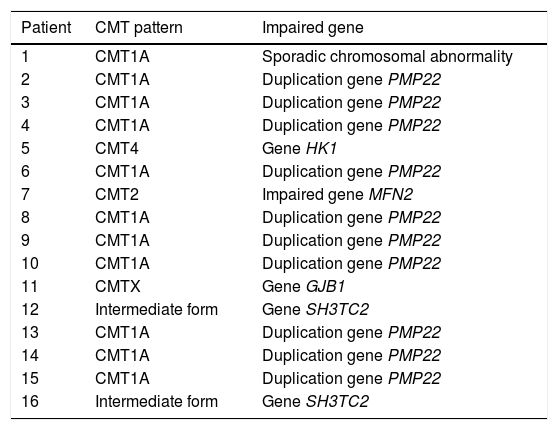
ResultsFrom the initial cohort of 38 patients, 21 operated feet were included in the study, of 16 patients (five bilateral cases) who met the inclusion criteria. The mean age of the group was 39.56 ± 16.39 years (age range 16–72 years), females comprised the largest group with 10 patients (62.5%). Age showed a normal distribution. Among the CMT patterns, type 1 A predominated at 10 cases (62.5%) (Table 1).
Genetic patterns of Charcot-Marie-Tooth.
| Patient | CMT pattern | Impaired gene |
|---|---|---|
| 1 | CMT1A | Sporadic chromosomal abnormality |
| 2 | CMT1A | Duplication gene PMP22 |
| 3 | CMT1A | Duplication gene PMP22 |
| 4 | CMT1A | Duplication gene PMP22 |
| 5 | CMT4 | Gene HK1 |
| 6 | CMT1A | Duplication gene PMP22 |
| 7 | CMT2 | Impaired gene MFN2 |
| 8 | CMT1A | Duplication gene PMP22 |
| 9 | CMT1A | Duplication gene PMP22 |
| 10 | CMT1A | Duplication gene PMP22 |
| 11 | CMTX | Gene GJB1 |
| 12 | Intermediate form | Gene SH3TC2 |
| 13 | CMT1A | Duplication gene PMP22 |
| 14 | CMT1A | Duplication gene PMP22 |
| 15 | CMT1A | Duplication gene PMP22 |
| 16 | Intermediate form | Gene SH3TC2 |
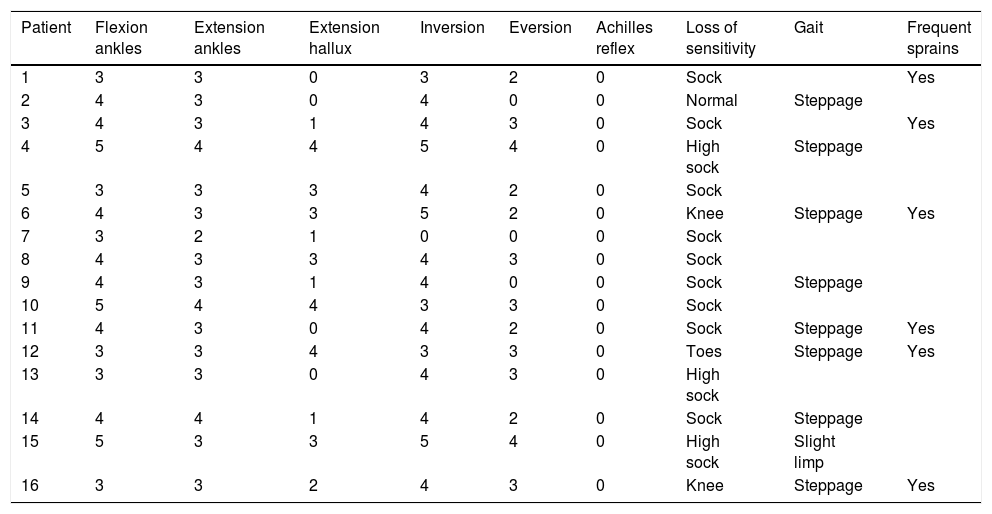
The patients’ characteristics are shown in Table 2, where we highlight the obvious weakness of ankle dorsiflexion (81% of the cases), hallux extension (81%) and foot eversion (87.5), as well as suppressed Achilles reflex. Eight people (50%) had steppage gait at the time of the initial examination and six (37.5%) had a history of ankle instability.
Preoperative strength according to the Medical Research Council (MRC) Scale for Muscle Strength and gait examination.
| Patient | Flexion ankles | Extension ankles | Extension hallux | Inversion | Eversion | Achilles reflex | Loss of sensitivity | Gait | Frequent sprains |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 3 | 3 | 0 | 3 | 2 | 0 | Sock | Yes | |
| 2 | 4 | 3 | 0 | 4 | 0 | 0 | Normal | Steppage | |
| 3 | 4 | 3 | 1 | 4 | 3 | 0 | Sock | Yes | |
| 4 | 5 | 4 | 4 | 5 | 4 | 0 | High sock | Steppage | |
| 5 | 3 | 3 | 3 | 4 | 2 | 0 | Sock | ||
| 6 | 4 | 3 | 3 | 5 | 2 | 0 | Knee | Steppage | Yes |
| 7 | 3 | 2 | 1 | 0 | 0 | 0 | Sock | ||
| 8 | 4 | 3 | 3 | 4 | 3 | 0 | Sock | ||
| 9 | 4 | 3 | 1 | 4 | 0 | 0 | Sock | Steppage | |
| 10 | 5 | 4 | 4 | 3 | 3 | 0 | Sock | ||
| 11 | 4 | 3 | 0 | 4 | 2 | 0 | Sock | Steppage | Yes |
| 12 | 3 | 3 | 4 | 3 | 3 | 0 | Toes | Steppage | Yes |
| 13 | 3 | 3 | 0 | 4 | 3 | 0 | High sock | ||
| 14 | 4 | 4 | 1 | 4 | 2 | 0 | Sock | Steppage | |
| 15 | 5 | 3 | 3 | 5 | 4 | 0 | High sock | Slight limp | |
| 16 | 3 | 3 | 2 | 4 | 3 | 0 | Knee | Steppage | Yes |
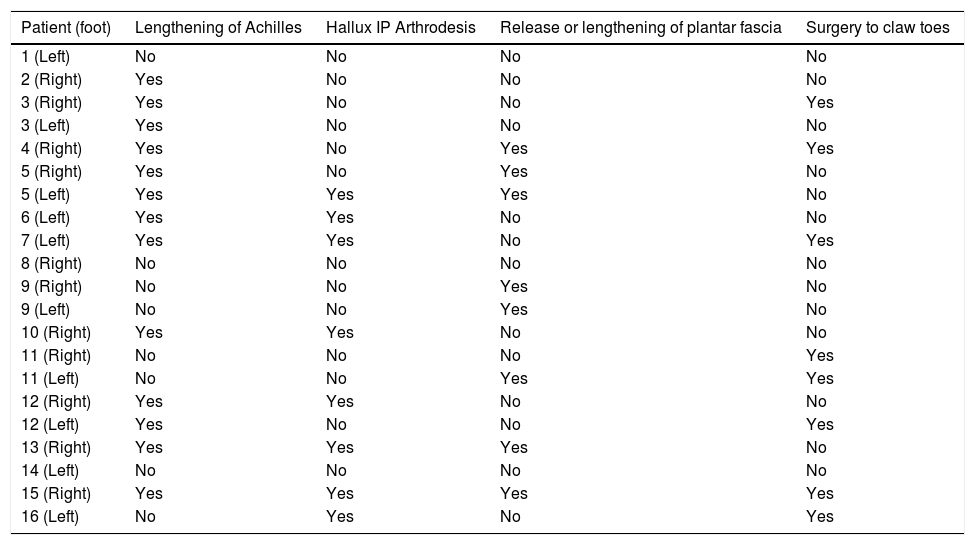
Table 3 lists the surgical procedures that were added to the basic surgery (posterior tibial tendon transfer, first metatarsal ascent osteotomy and calcaneal valgus osteotomy): interphalangeal arthrodesis of the hallux to correct clawing of the first toe (eight patients), percutaneous Achilles tendon lengthening (13 patients), plantar fascia section (eight patients) and lesser toe surgery (proximal interphalangeal arthrodesis) (eight patients).
Added surgical procedures performed on patients.
| Patient (foot) | Lengthening of Achilles | Hallux IP Arthrodesis | Release or lengthening of plantar fascia | Surgery to claw toes |
|---|---|---|---|---|
| 1 (Left) | No | No | No | No |
| 2 (Right) | Yes | No | No | No |
| 3 (Right) | Yes | No | No | Yes |
| 3 (Left) | Yes | No | No | No |
| 4 (Right) | Yes | No | Yes | Yes |
| 5 (Right) | Yes | No | Yes | No |
| 5 (Left) | Yes | Yes | Yes | No |
| 6 (Left) | Yes | Yes | No | No |
| 7 (Left) | Yes | Yes | No | Yes |
| 8 (Right) | No | No | No | No |
| 9 (Right) | No | No | Yes | No |
| 9 (Left) | No | No | Yes | No |
| 10 (Right) | Yes | Yes | No | No |
| 11 (Right) | No | No | No | Yes |
| 11 (Left) | No | No | Yes | Yes |
| 12 (Right) | Yes | Yes | No | No |
| 12 (Left) | Yes | No | No | Yes |
| 13 (Right) | Yes | Yes | Yes | No |
| 14 (Left) | No | No | No | No |
| 15 (Right) | Yes | Yes | Yes | Yes |
| 16 (Left) | No | Yes | No | Yes |
Median follow-up was 42.25 months, with a median of 33 and an interquartile range of 26.25 months.
Significant differences (P = .003) were detected in functional assessment with the AOFAS score. The pre-surgical AOFAS score was 37.25 ± 19.27, whereas one year after surgery it was 86.50 ± 10.53, with a mean difference of 49.25 points. The post-surgical AOFAS score for the 21 feet assessed was classified as excellent in 13 feet (61.9%), good in five (23.8%), fair in two (9.5%, patient 1 and 14), and poor in one (4.7%, patient 13).
During follow-up, only two feet (9.5% of those operated) required further surgery. We highlight one case, patient 14, where the initial hindfoot varus correction was not good and had to be corrected by subtalar arthrodesis, with a satisfactory result. This patient represents the only conversion from osteotomy to arthrodesis in the entire series (6.25%). Finally, patient number 13, who had hyperextension of the hallux despite the M1 ascent osteotomy and arthrodesis of the interphalangeal joint of the hallux, which was the reason for their dissatisfaction with the treatment initially proposed. This had to be corrected with lengthening of the hallux extensor and dorsal capsulotomy of the first metatarsophalangeal joint, with an acceptable, although not entirely satisfactory, result.
In terms of patient satisfaction and subjective improvement after one year, assessed with a qualitative scale, we found most of the subjects to be happy with the surgery performed: 56.25% of the 16 patients were “very satisfied”, 18.75% were “satisfied”, 12.5% were “indifferent” and 12.5% were “dissatisfied”. The two dissatisfied cases were patient 1, who had an uncontrolled underlying pathology (fibromyalgia) which indirectly affected satisfaction, and patient 13, who initially reported clinically uncomfortable claw toes despite a good radiological appearance, and who did not undergo surgery.
Pre- and postoperative radiographic measurement also showed statistically significant differences. The initial Meary's angle was 20.46° ± 6.13° and decreased to 13.38° ± 7.06° with a mean correction of 6° (P < .005). In the case with calcaneal inclination, we went from 25.30° ± 5.90° preoperatively to 21.92° ± 5.66° postoperatively, achieving a mean correction of about 4.5° (P = .0004).
DiscussionIn patients with cavovarus feet as a clinical manifestation of Charcot-Marie-Tooth disease that generate symptoms, a surgical approach is recommended to treat deformities that are not very rigid or structured. Thus, we avoid the onset of degenerative joint changes and the need for arthrodesis surgery. The deformity present in these feet is a consequence of abnormalities affecting the hindfoot, midfoot and forefoot, which is why we believe that treatment should combine several surgical techniques.17,18
The main aim of surgery for these patients is to achieve a stable foot in a plantigrade position.9
If the varus hindfoot is a consequence of plantar flexion of the first radius,19 we believe that correction of anterior cavus with dorsiflexion osteotomy of the first radius can resolve talus varus, as Ward20 states, but only in young patients with flexible feet. We believe that, by adding a Dwyer-type calcaneal valgus osteotomy in less flexible and even stiff hindfeet, we can achieve excellent corrections without arthrodesing any joints. There is no doubt that, by improving the overall biomechanical alignment of the foot, an improvement in pain reduction and greater stability is achieved.21
Tendon transfer of the tibialis posterior aims to support the clearly weakened tibialis anterior, correcting foot drop, actively assisting during the first rocker22,23 and improving stability during the support phase. In addition, we eliminate its deforming force in varus and supination without the opposition of the peroneus brevis, aiding correction. Some studies propose transferring the tibialis anterior muscle to the third wedge, but this tends to present more rapid progression of the disease with early claudication, and therefore function is better preserved with the use of the tibialis posterior.24–26
We believe, therefore, that the combination of the two bone procedures described above (first metatarsal ascent osteotomy and calcaneal valgus osteotomy) together with a soft-tissue procedure (posterior tibial tendon transfer) offers excellent or good results in most patients with cavus feet in CMT, provided they show no degenerative signs.
In some of our patients, we also combine other surgical procedures on an individual basis, such as lengthening of the Achilles tendon,27 tenotomy of the plantar fascia28 or correction of clawing of the hallux or lesser toes.9 Thus, we achieve better adaptation of the foot to a shoe, clearly improving the patient's subjective perception.29
In cases with severe bone deformities or in the presence of signs of joint degeneration, it is worth considering arthrodesis (generally triple) instead of the extra-articular surgeries proposed in this article.25,30
It is also important to remember that surgery does not alter the course of the disease or improve its prognosis, although it does improve functionality, and it is vitally important that the patient understands the extent of the benefit that can be obtained through surgery.
In our series, there was no progression of the deformity during the follow-up period after a mean 42 months of monitoring, although there was one initial hypocorrection (reintervention at 22 months). However, the literature describes progression of up to 30% in some series, which in most cases usually require triple arthrodesis.7,25,31
Radiographic analysis revealed that, although the correction obtained with respect to the preoperative parameters was significant, slight residual cavus persisted in most patients, which did not affect the patient’s final functional quality.
Most of our patients reported a high degree of satisfaction with the surgery, with marked recovery on the AOFAS functional scale. However, this is a progressive systemic disease, and it is to be expected that the functional results will be affected in the long term, despite adequate correction being achieved.32
We can highlight as limitations of our study the fact that it is a retrospective review and the low number of patients, which may make it susceptible to committing type II statistical error; nevertheless, our group of subjects is among the largest published in the current literature. Although almost all the study participants have a homogeneous phenotype, there is a wide variety of genetic subtypes, which makes it difficult to standardise or predict a similar functional outcome for these patients in the long term.
Furthermore, it should be noted that our work followed a similar surgical protocol in all patients, with the aim of standardising the process. This brings homogenisation to the sample and data collection, as there are numerous studies focussing on the surgical treatment of patients with CMT, but with multiple techniques that make them more difficult to evaluate.
ConclusionIn conclusion, the results of our study suggest that the surgical technique described (posterior tibial tendon transfer, first metatarsal ascent osteotomy and calcaneal valgus osteotomy) for the treatment of pes cavovarus in patients with CMT achieves adequate function with a plantigrade foot. Individuals can wear regular footwear, no recurrence of the deformity or degenerative changes are observed in the medium term, and the rate of secondary surgeries is very low.
Level of evidenceLevel of evidence IV.
FundingNo funding was received for this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Jordà-Gómez P, Sánchez-Gonzalez M, Ortega-Yago A, Navarrete-Faubel E, Martínez-Garrido I, Vicent-Carsí V. Manejo del pie cavo-varo flexible en pacientes con enfermedad de Charcot-Marie-Tooth: resultados a medio plazo. Rev Esp Cir Ortop Traumatol. 2021;65:355–362.