Developmental hip dysplasia is a frequent cause of coxofemoral pain in young adults. Bernese periacetabular osteotomy emerges as a possible option for the management of pain relief and functional limitation, in order to delay the need for arthroplasty in these patients.
Material and methodsA descriptive retrospective study was conducted on 26 selected patients with symptomatic developmental hip dysplasia treated with bernese periacetabular osteotomy between 1996 and 2009 (94% women). Mean age at time of surgery was 39.8 years (15–49 years), with a mean follow-up of 10 years. Osteoarthritis (OA Tönnis scale), acetabular index and Wiberg angle were evaluated by radiology and functionality was valued by using the de Merle D’Aubigné-Postel scale.
ResultsThe mean hospitalisation time was 10 days. At 10 years, the mean radiography value of acetabular index was 9.03° and 38.3° for Wiberg angle (17° and 27° correction, respectively, above the mean pre-operative values). Joint lock was referred to by 43% of patients and 53% to non-evidence based limb failure. Mean functional value was 14.30 (Good). At 5 years of follow-up, 20% advanced at least by one grade in OA Tönnis scale compared to their pre-operative status, increasing to 55% at 10 years. At 10 years after surgery, 83% patients did not need arthroplasty and 85% showed high satisfaction level.
ConclusionsBernese periacetabular osteotomy is a useful alternative in young adults with symptomatic developmental hip dysplasia that can improve pain relief, femoral head coverage, and slow down coxofemoral osteoarthrosis progression in order to delay arthroplasty.
La displasia del desarrollo de cadera es causa frecuente de dolor coxofemoral del adulto joven. La osteotomía periacetabular bernesa se perfila como una forma de abordar el problema de dolor, limitación funcional y necesidad de artroplastia a edades tempranas en estos pacientes.
Material y métodoEstudio descriptivo retrospectivo de 26 pacientes seleccionados con displasia del desarrollo de cadera sintomáticos, tratados mediante osteotomía periacetabular bernesa, entre 1996 y 2009 (mujeres 94%). La edad media en el momento de la cirugía era de 39,8 años (rango: 15-49), con seguimiento medio de 10 años. Valoramos radiológicamente evolución de artrosis (escala de Tönnis), índice acetabular y ángulo de Wiberg; funcionalmente utilizamos la escala de Merle-D’Aubigné-Postel.
ResultadosEl tiempo medio de hospitalización fue de 10 días. El valor radiográfico medio a los 10 años fue de índice acetabular: 9,03° y ángulo de Wiberg: 38,3° (corrección de 17° y 27° respectivamente, sobre valores medios preoperatorios). El 43% refería bloqueo articular y el 53% fallo del miembro no evidenciable. Valor promedio funcional de 14,30 (bueno). A los 5 años de seguimiento, el 20% progresó en al menos un grado según la escala de Tönnis respecto a su estado preoperatorio, y a los 10 años, el 55%. A largo plazo, el 83% de los pacientes no precisó artroplastia a los 10 años y el 85% de nuestros pacientes confesó alto grado de satisfacción.
ConclusionesLa osteotomía periacetabular bernesa es una alternativa terapéutica útil en adultos jóvenes con displasia del desarrollo de cadera sintomática, mejorando el dolor, la cobertura cefálica femoral y retrasando la progresión de osteoartrosis coxofemoral.
Developmental hip dysplasia (DHD) is a pathology with an incidence of about 1:1000 live births in our environment. However, some meta-analyses in the literature maintain that this figure could be underestimated, and that a correct exploration by an orthopaedic surgeon could increase up to 11:1000, rising to even 25:1000 if an imaging test, like an ultrasound, is added. An early diagnosis is important, as it enables early and correct treatment, which, if established during the first 6 months of life, increases the percentage of successes up to 85–95%.1 On the other hand, the percentage of satisfactory treatments decreases after this threshold, whilst complications gradually increase, becoming especially notable after the age of 3 years.
DHD which is not diagnosed in time during infancy produces a residual dysplastic hip in the adult, which may be either symptomatic or not. When it is, at an age between 20 and 40 years, patients report pain,2,3 functional limitation, locking, clicking, limb failure, onset of labral lesions4 and early arthrosis, which represent a challenge for orthopaedic surgeons and which may lead to joint replacement at an early age5 if they are not treated in the early stages through non-prosthetic surgical methods, like osteotomies.
Pelvic reorientation osteotomies require joint congruence and a spherical femoral head. Out of all the options, we have analysed our medium-term results with bernese periacetabular osteotomy (bernese PAO), as described by Ganz, which enables a reorientation of the acetabulum through a single approach route (modified Smith-Petersen) without interrupting the pelvic ring.6,7
Materials and methodsWe reviewed a series of 26 patients intervened at the Traumatology Service of Hospital Clínico San Carlos in Madrid due to symptomatic adult hip dysplasia between 1996 and 2004 (20 of them as follow-up of patients who were part of another series published previously in another article). Regarding the distribution by gender, 24 were females and 2 were males, with 20 cases of unilateral involvement and 6 of bilateral involvement. The mean age was 39.8 years (minimum of 15 and maximum of 49). We lost 1 individual in our study and had 1 case of death due to massive pulmonary embolism in the first hours after the operation.
Patients reviewed in this study were intervened based on their symptoms and the procedure was defined based on the radiographic study:
- (a)
Patients with closed triradiate cartilage and under 55 years of age.
- (b)
Pain resistant to adequate drug management according to the WHO analgesic scale.
- (c)
Adequate joint balance.
- (d)
Within the following radiographic parameters in an AP pelvic projection: femoroacetabular spherical congruence in abduction and internal rotation, arthrosis grade under or equal to II according to the Tönnis scale (Table 1) and Wiberg angle <20° and acetabular index >25°.
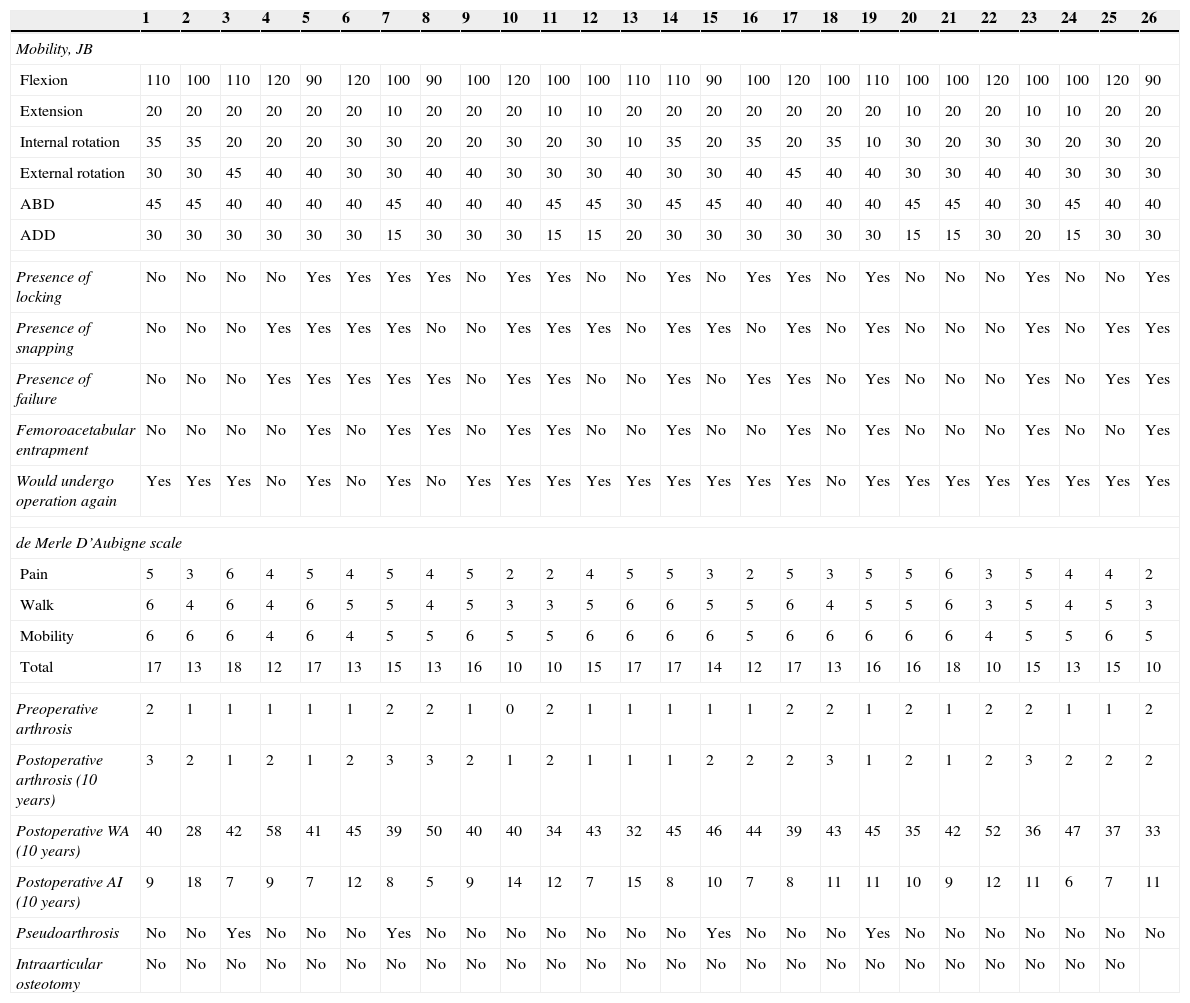
Table 1.Patient assessment results in our series (the results from patients who did not complete the follow-up are not reflected).
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 Mobility, JB Flexion 110 100 110 120 90 120 100 90 100 120 100 100 110 110 90 100 120 100 110 100 100 120 100 100 120 90 Extension 20 20 20 20 20 20 10 20 20 20 10 10 20 20 20 20 20 20 20 10 20 20 10 10 20 20 Internal rotation 35 35 20 20 20 30 30 20 20 30 20 30 10 35 20 35 20 35 10 30 20 30 30 20 30 20 External rotation 30 30 45 40 40 30 30 40 40 30 30 30 40 30 30 40 45 40 40 30 30 40 40 30 30 30 ABD 45 45 40 40 40 40 45 40 40 40 45 45 30 45 45 40 40 40 40 45 45 40 30 45 40 40 ADD 30 30 30 30 30 30 15 30 30 30 15 15 20 30 30 30 30 30 30 15 15 30 20 15 30 30 Presence of locking No No No No Yes Yes Yes Yes No Yes Yes No No Yes No Yes Yes No Yes No No No Yes No No Yes Presence of snapping No No No Yes Yes Yes Yes No No Yes Yes Yes No Yes Yes No Yes No Yes No No No Yes No Yes Yes Presence of failure No No No Yes Yes Yes Yes Yes No Yes Yes No No Yes No Yes Yes No Yes No No No Yes No Yes Yes Femoroacetabular entrapment No No No No Yes No Yes Yes No Yes Yes No No Yes No No Yes No Yes No No No Yes No No Yes Would undergo operation again Yes Yes Yes No Yes No Yes No Yes Yes Yes Yes Yes Yes Yes Yes Yes No Yes Yes Yes Yes Yes Yes Yes Yes de Merle D’Aubigne scale Pain 5 3 6 4 5 4 5 4 5 2 2 4 5 5 3 2 5 3 5 5 6 3 5 4 4 2 Walk 6 4 6 4 6 5 5 4 5 3 3 5 6 6 5 5 6 4 5 5 6 3 5 4 5 3 Mobility 6 6 6 4 6 4 5 5 6 5 5 6 6 6 6 5 6 6 6 6 6 4 5 5 6 5 Total 17 13 18 12 17 13 15 13 16 10 10 15 17 17 14 12 17 13 16 16 18 10 15 13 15 10 Preoperative arthrosis 2 1 1 1 1 1 2 2 1 0 2 1 1 1 1 1 2 2 1 2 1 2 2 1 1 2 Postoperative arthrosis (10 years) 3 2 1 2 1 2 3 3 2 1 2 1 1 1 2 2 2 3 1 2 1 2 3 2 2 2 Postoperative WA (10 years) 40 28 42 58 41 45 39 50 40 40 34 43 32 45 46 44 39 43 45 35 42 52 36 47 37 33 Postoperative AI (10 years) 9 18 7 9 7 12 8 5 9 14 12 7 15 8 10 7 8 11 11 10 9 12 11 6 7 11 Pseudoarthrosis No No Yes No No No Yes No No No No No No No Yes No No No Yes No No No No No No No Intraarticular osteotomy No No No No No No No No No No No No No No No No No No No No No No No No No ABD: abduction; ADD: adduction; AI: acetabular index; JB: joint balance; WA: Wiberg angle.
The exclusion criteria were the Matta criteria,8 a short and horizontal ceiling due to the risk of generating an inverse obliqueness thereof; as well as an acetabulum in retroversion.
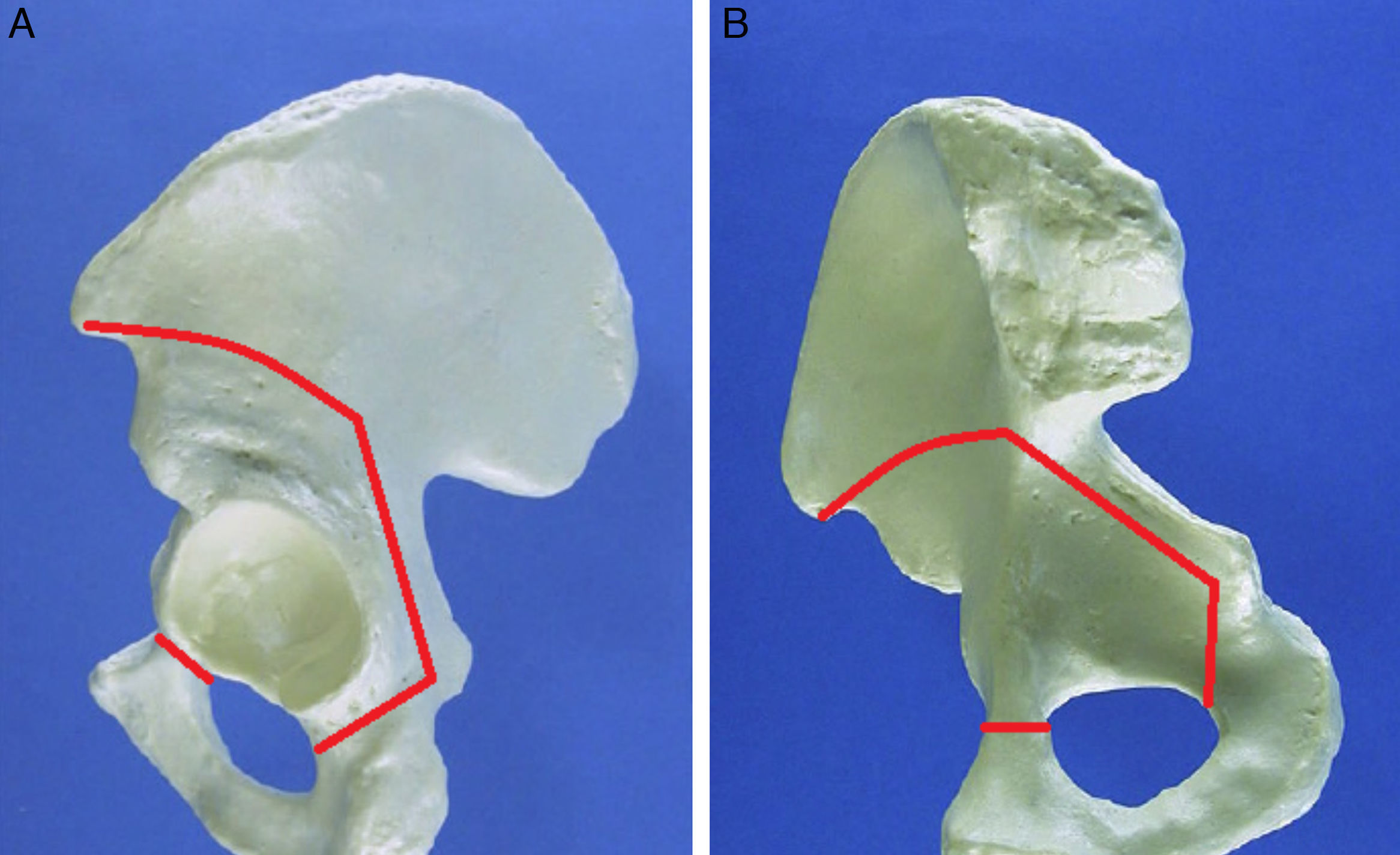
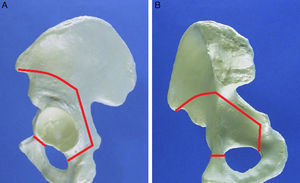
The technique was based on a modified Smith-Petersen approach, according to the report by Ganz31 (Fig. 1). In our series we did not routinely perform associated actions, such as femoral osteotomy or revision or labral suture.
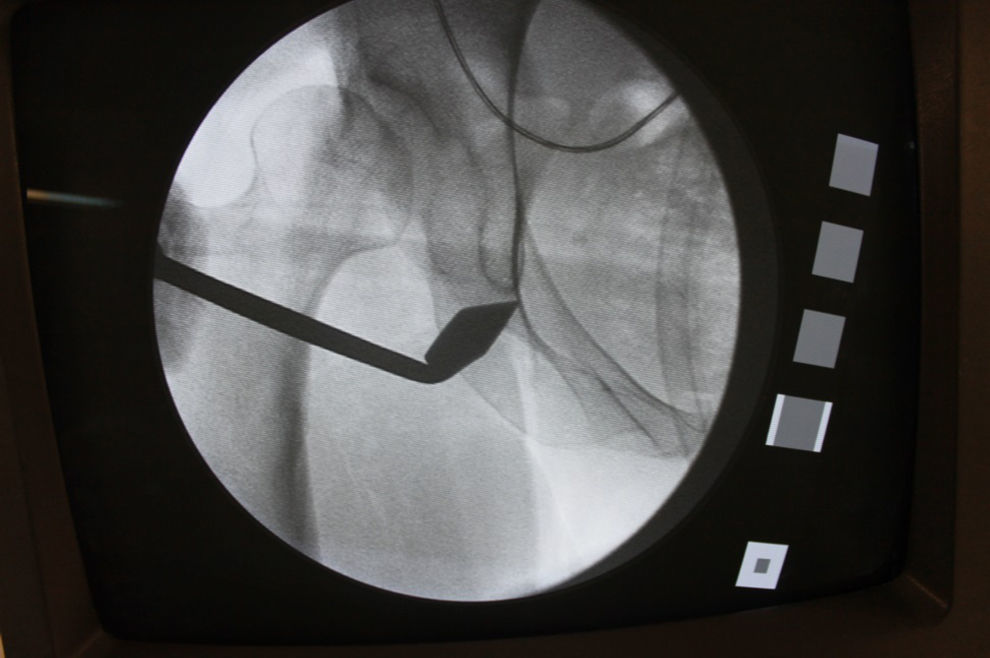
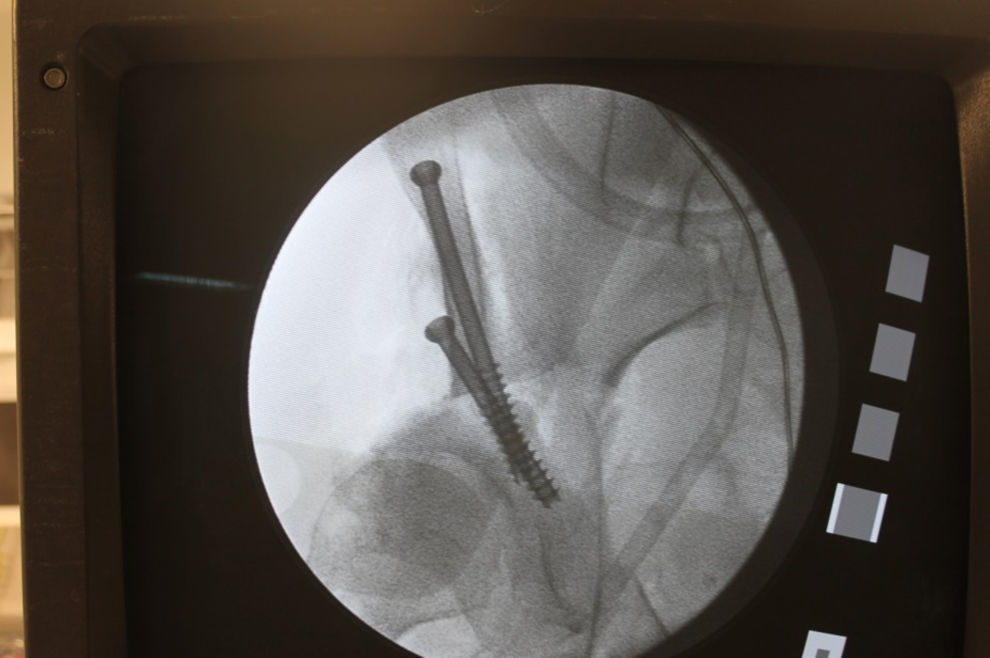
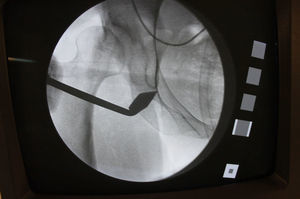
Once manipulation of the acetabulum was concluded we carried out an intraoperative fluoroscopic control which helped to determine the correct position of the acetabulum (Fig. 2) with an AP pelvic projection centred on the X-ray beam and at a distance of 1m with the bone fragments provisionally fixed with Kirschner wires or Steinmann nails (Fig. 3).
The criteria to determine a correct acetabular position were: Wiberg angle (WA) 25–35°, acetabular index (AI) 0–10°, distance <10mm between the ischial line and the femoral head, recovery of the Shenton line and joint congruence with absence of the cross sign (correct anteversion).9
Following the surgery, patients remained in bed for 1 week, followed by 8 weeks of limb discharge, and then starting with partial load which was progressively increased until total load without crutches was authorised. All the patients followed a prophylactic protocol to prevent venous thromboembolism, with 6 weeks of low molecular weight heparin.
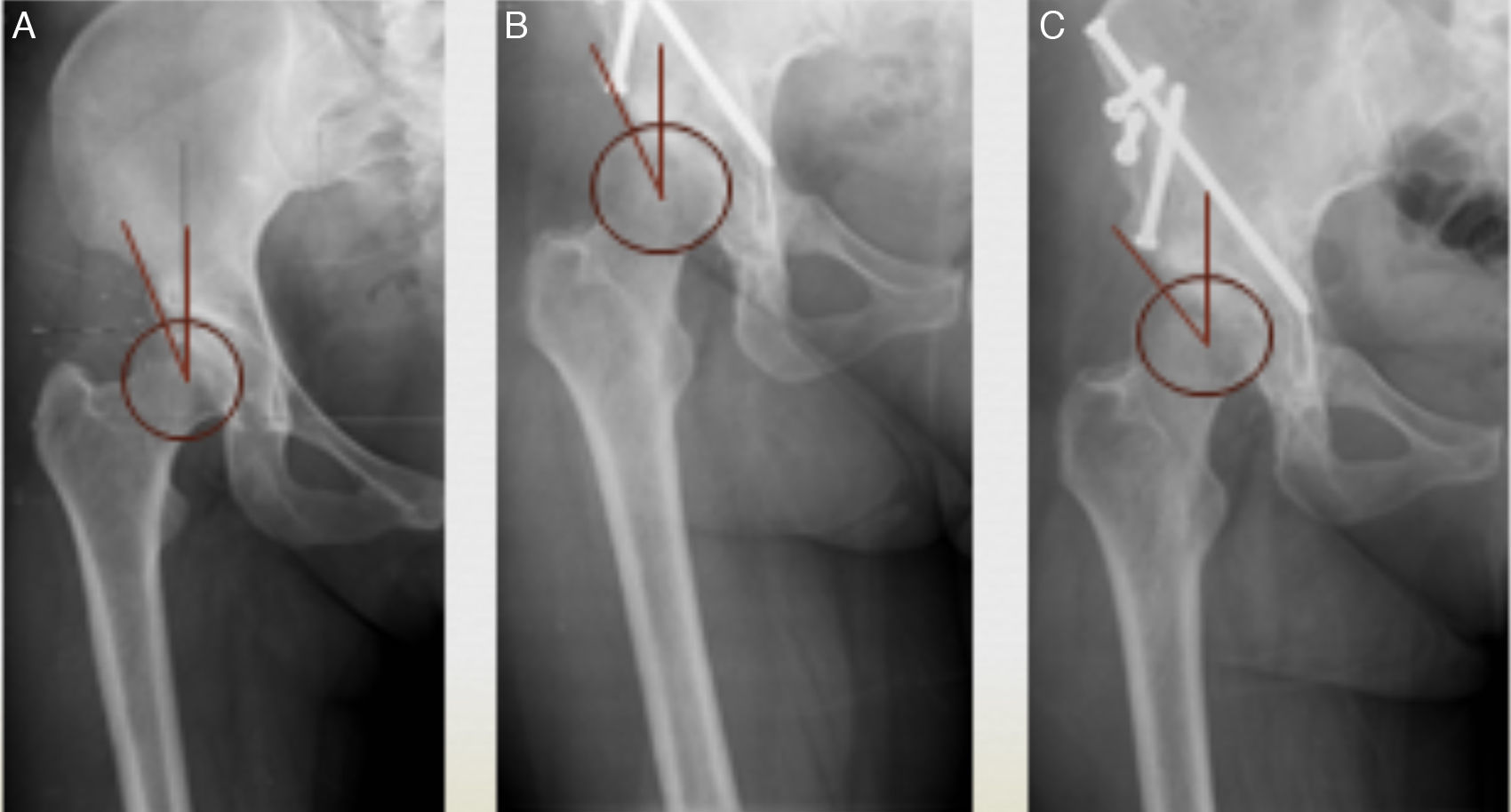
All patients were clinically and radiographically monitored, in outpatient clinic, at 1, 3 and 6 months and annually thereafter, in order to ascertain the presence of characteristics of pain, blocking, snapping or limb failure, joint balance, the consolidation process, and the evolution of the Wiberg angle and the acetabular index on a pelvic AP radiograph (Fig. 4).
ResultsWhen recording the functional assessment of our patients according to the de Merle D’Aubigne-Postel scale, we obtained a mean result of 3.89 points for pain assessment, 4.78 for walking and 5.63 for mobility, with a mean overall result of 14.30 points out of a possible 18 for the 3 sections (Table 1), which corresponded to a good result.
In terms of the level of subjective satisfaction of the patients, based on the response to the question “Knowing your previous state, how the surgery developed, its consequences and your current condition, would you undergo the same treatment again?”, 85% of the subjects responded in the affirmative.
The range of follow-up time of these patients was between 10 and 17 years. Upon physical exploration 10 years after the procedure, we observed a mean joint balance of flexion F: 105.4°, extension E: 17.7°, abduction ABD: 41°, adduction ADD: 25.7°, internal rotation IR: 25.2° and external rotation ER: 35°.
In total, 46% of patients reported joint blocking which was not reproducible during the physical exploration, whilst in 53.8% we detected clicks with no clinical repercussion, or they reported limb failure, and 38.4% of cases with evident pain during the femoroacetabular impingement triggering manoeuvres.
In symptomatic hips, the preoperative values were WA 11° and AI 24°. The grades of preoperative OA according to the Tönnis scale were 0: 1, I: 16, II: 11 and III: 0. After the surgery we obtained a mean correction of 27° for the WA, and 15° for the AI, observing an increase of at least 1 OA grade in 20% of the patients after 5 years and 54% after 10 years. Only 1 patient required an arthroplasty in less than 5 years, due to moderate-severe pain with no response to pharmacological management. The patient presented grade II according to the Tönnis scale before the intervention. After 10 years, 83% of the individuals in the series had not required rescue osteotomy to implant a total hip prosthesis.
During the medium- and long-term evolution we identified 4 cases (14%) of pseudoarthrosis, 2 of them in the iliopubic ramus and the other 2 in the ischiopubic ramus, with no clinical repercussions.
We observed 3 cases of overcorrection of the Wiberg angle (>50° measured in the postoperative control radiograph), with no cases of intraarticular access during the osteotomy.
None of the relationships between joint balance, angular correction and functionality studied using the statistics software package SPSSv22.0 were statistically significant for a level of P<.05.
DiscussionIn 2012, Yasunaga et al. conducted a meta-analysis which settled the basis of the current indications to carry out a bernese PAO. These are patient: (a) with closed triradiate cartilage (15 years) and under 50 years, (b) suffering painful DHD for over 6 months despite adequate management, (c) with an adequate joint balance (at least 90° flexion, 15° abduction and 10° adduction and external rotation according to the Harris Hip Score), and (d) within the following radiographic parameters in an AP pelvic projection: joint spherical congruence in abduction and internal rotation, grade 0-I arthrosis according to the Tönnis scale (II and III only in patients aged under 30 years), Wiberg angle <20°, and joint space >2.2mm.10,11 In our study we shared many of these inclusion criteria since, due to the moment at which patients in our series were intervened, it was not possible to conduct the new imaging techniques that would have allowed us to study the condition and viability of the joint cartilage, such as dGEMRIC, T2 mapping and T1ρ.12,13 Such techniques could have improved the surgical indication to perform Ganz PAO, by ruling out patients with advanced cartilage lesions.
It is essential for the following aspects to be clear during the surgery:
- -
An adequate fluoroscopic control: especially during the incision at the level of the ischium, where the distance from the edge at which the osteotomy is carried out is very important to preserve the stability conferred by the continuity of the posterior pillar without entering the joint (with the latter being a worse circumstance), with possible damage to the joint cartilage or alteration of joint congruence.
- -
Iliac section through an endopelvic approach: in order to preserve vascularisation of the acetabulum, subsidiary of the superior gluteal and obturator arteries. This achieves a very low incidence of necrosis of the acetabulum (Hussell et al.14).
- -
Repairing the labrum through transosseous suture, if necessary, as recommended by Ganz himself,32 to decrease the feeling of joint locking and limb failure.
- -
Intraoperative radiographic control (of better quality than the radioscopic) of the acetabular position. In spite of the existence of discrepancies between the measurements with the intraoperative device and a regulated radiographic study, according to Lehmann and Nepple15 there is a correlation between both studies in 88% of cases for the WA and in 60% for the AI. It is for this reason that, when we decided to fix the osteotomy, we did so based on the WA obtained in the surgical theatre in an AP projection of the coxofemoral joint.
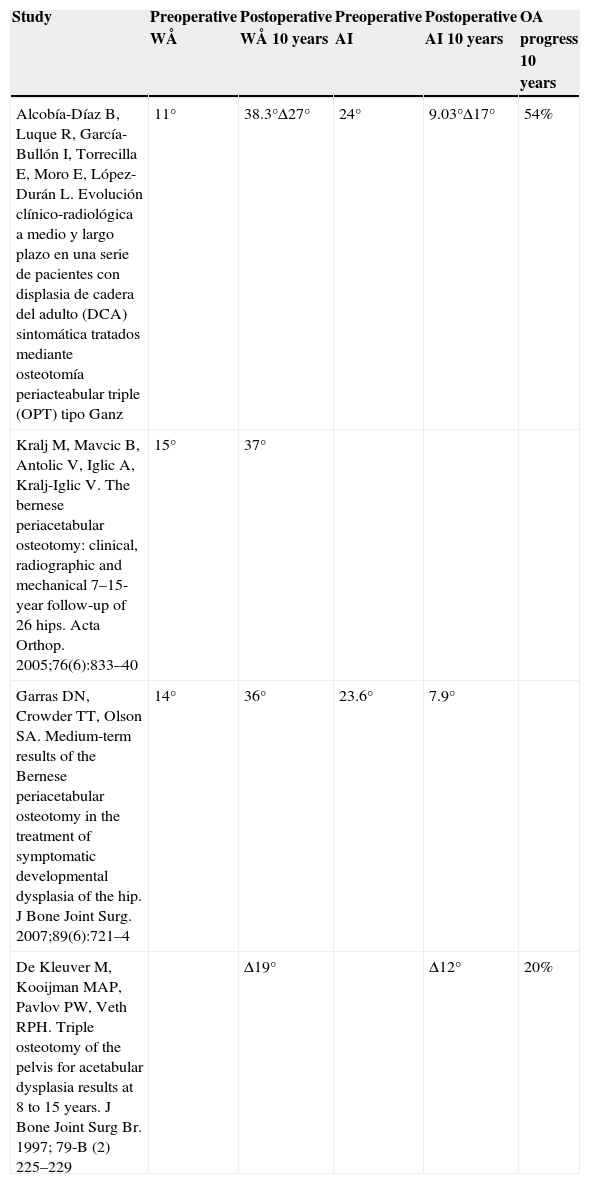
Regarding the grade of angular correction, our results coincided with those obtained in other published series, with our mean WA at 10 years being 38.3°, and our mean AI being 9.03°. In the series by Kralj the value for WA was 37°, whilst in that by Garras the value of WA was 36° and the value of AI was 7.9° (Table 2). It is possible that the value of AI was not necessarily due to an improvement, rather the opposite, as it increased over the years. This would be due to progression of the disease, which leads to a progression of osteophyte formation in the superior edge of the acetabulum, increasing the coverage of the femoral head at its own expense.
Comparison of results obtained in other previous studies.
| Study | Preoperative WÅ | Postoperative WÅ 10 years | Preoperative AI | Postoperative AI 10 years | OA progress 10 years |
|---|---|---|---|---|---|
| Alcobía-Díaz B, Luque R, García-Bullón I, Torrecilla E, Moro E, López-Durán L. Evolución clínico-radiológica a medio y largo plazo en una serie de pacientes con displasia de cadera del adulto (DCA) sintomática tratados mediante osteotomía periacteabular triple (OPT) tipo Ganz | 11° | 38.3°Δ27° | 24° | 9.03°Δ17° | 54% |
| Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15-year follow-up of 26 hips. Acta Orthop. 2005;76(6):833–40 | 15° | 37° | |||
| Garras DN, Crowder TT, Olson SA. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg. 2007;89(6):721–4 | 14° | 36° | 23.6° | 7.9° | |
| De Kleuver M, Kooijman MAP, Pavlov PW, Veth RPH. Triple osteotomy of the pelvis for acetabular dysplasia results at 8 to 15 years. J Bone Joint Surg Br. 1997; 79-B (2) 225–229 | Δ19° | Δ12° | 20% |
AI: acetabular index; OA: osteoarthritis; WÅ: Wiberg angle.
In the series by Tönnis et al.,3 17% of the cases presented a clear progression of arthrosis, as was the case in 83% of grade III cases in the series by Matta et al.7 after 10 years, notably below our own results, which were over 50%. In addition, it was observed that the progression of OA was greater after grade II, which leads us to believe that this grade should be the cut-off point to restrict these type of surgeries for individuals aged under 30 years and without labral involvement. At present, there is a tendency to attach greater importance to posterior coverage defects, versus anterior, and a preoperative CT assessment is preferred over surgery to calculate the translation to be applied to the acetabular fragment during surgery.16 The grade of postoperative angular correction was, along with preoperative arthrosis, age and labral tear, a determinant factor of the result. Both Tönnis and Siebenrock17 associated a poor evolution to postoperative frontal (WA) and anterior coverage angles over 40° and an inferior roof tilt angle (AI) over −10°. Although we did not register statistically significant data in our series, we did appreciate a tendency to present better functional results when the postoperative Wiberg angle after 10 years was equal to 40±5°.
We could associate a varisation femoral osteotomy in patients with marked coxa valga anteversion and/or in cases in which, after the bernese PAO, femoroacetabular congruence could be improved by repositioning.19
From a functional standpoint, our patients presented a mean value of 14.30 points after 10 years for the scale used, versus nearly 8 points described in some series published to date, with the greatest improvements being recorded in the section on mobility. On the other hand, in the future it would be interesting to track the evolution of these patients, given that some publications have noted the fact that, between 10 and 20 years after the surgery, the functional scale values tend to decrease again due to a progression of the disease.18,20,21
While other series publish figures for femoroacetabular involvement around 18–24%,19,20,22 in our case 38.4% of patients presented it. This difference could be due to the fact that our series of patients had a mean age of 39 years, versus a mean value of 33 years in the series compared; or to the progression of normal joint wear after 10 years.
Pseudoarthrosis of the various osteotomy paths may appear, with the pubic being the most frequent, in up to 16% in some series23,24 and 14% in ours. This figure did not have clinical relevance. In order to prevent this occurrence, Tönnis described how to perform a tension cerclage.
In our series we observed 7.5% of heterotopic ossifications, a figure comparable to 5% in the series published by the Mayo Clinic,25 which is related to respecting the external iliac fossa and gluteal musculature.
The fact that 83% of patients in our series maintained their own joint after 10 years of our intervention is considered to be a result in accordance with those published by various series in the literature.17,26–30 The only patient in whom the process failed (understanding as such the need for arthroplasty in less than 5 years) corresponded to a case with grade II initial arthrosis with a subchondral cyst of about 10mm diameter and preoperative values of WA 20° and AI 18°, who continued to suffer significant pain and functional limitation throughout the first year of postoperative evolution. The preoperative values showed corrections of 50° and 5°, respectively. The patient presented obesity, sedentary life and coagulation disorders in relation to rheumatological pathology.
The repair of labral lesions is associated to an improvement in the feeling of limb failure and joint locking.
An adequate posterior coverage and WA between 30° and 40° and AI between 5° and 10°, were related to a better prognosis.
The authors of the present work are aware of the limitations that it may present, including the fact of being a series with very few patients which was reviewed retrospectively. However, given the infrequent application of the technique studied, for the reason mentioned previously, it is one of the longest series found in the literature and with a long follow-up period. Although the results do not have the necessary statistical significance, they have provided several ideas.
The intervention is technically challenging and has a pronounced learning curve, as reflected by all the authors. However, when orthopaedic surgeons follow the appropriate indications and it is conducted with adequate planning and surgical technique, we managed to improve the function of our patients, decrease their pain and slow down the rate of wear of the joint cartilage. In this way, we managed to slow down coxofemoral joint degeneration and delay arthroplasties until a later age.
In summary, we propose performing a bernese PAO as a therapeutic alternative for young adult patients, aged between 15 and 49 years, suffering painful DHD with a non-deformed femoral head, joint congruence, joint space >2.2mm, WA between 10 and 30°, and grade 0 or I arthrosis according to the Tönnis scale; limiting grades II and III to patients younger than 30 years.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Alcobía Díaz B, Luque Pérez R, García Bullón I, Moro Rodríguez LE, López-Durán Stern L. Evolución clínico-radiológica a largo plazo en una serie de 26 pacientes con displasia de cadera del adulto sintomática tratados mediante osteotomía periacetabular bernesa. Rev Esp Cir Ortop Traumatol. 2015;59:421–428.