Revision total knee arthroplasty (TKA) is a common procedure with varying results depending on the cause. Our objective was to compare the clinical and radiological outcomes in patients undergoing aseptic revision versus revision due to prosthetic infection.
Material and methodsThe study included 41 patients who underwent TKA revision with the same varus-valgus constrained implant. In all cases a clinical evaluation was performed including pain, range of motion (ROM), Knee Society Score (KSS), complications, as well as radiological study. A comparative analysis was performed on the pre- and postoperative results between septic and aseptic groups. The mean follow-up was 6 years.
ResultsROM had a mean increase of 17° (p<.01). KSS and functional KSS improved significantly postoperatively. In the radiological study, joint interline and limb alignment were restored in all cases. Radiolucencies were found in 36.5% of cases; however they were unrelated to the appearance of loosening of the implant. There were complications in 29.2% of cases, mostly related to the surgical wound. Mobility, KSS, KSS functional and satisfaction at follow-up were better in the septic group. Implant survival was 95% at follow-up.
ConclusionRevision arthroplasty with constrained varus-valgus implant is safe, and has successful mid-term results despite the cause of the replacement procedure.
La artroplastia de revisión de rodilla es un procedimiento frecuente con resultados variables en función de la causa. Nuestro objetivo fue comparar los resultados clínicos y radiológicos en pacientes sometidos a revisión protésica tras infección frente aquellos con revisión por causa aséptica.
Material y métodosSe incluyeron 41 casos de revisión con el mismo implante constreñido varo-valgo. En todos los casos se realizó una valoración clínica (dolor, rango de movilidad, función mediante la escala KSS) y de complicaciones, así como un estudio radiológico. Se realizó un análisis comparativo de los resultados pre y postoperatorios y entre los grupos de causa séptica y aséptica. El seguimiento final medio fue de 6 años.
ResultadosLa movilidad al final del seguimiento mejoró una media de 17° de balance articular (p<0,01). El KSS y el KSS funcional mejoraron significativamente respecto al preoperatorio. Radiológicamente, se restauró la interlínea articular y se corrigió el eje del miembro en todos los casos. Se encontraron radiolucencias en el 36,5% de los casos sin relación con la aparición de aflojamiento del implante. Se produjeron complicaciones en el 29,2% de los casos, siendo la mayoría relacionadas con la herida quirúrgica. La movilidad, el KSS, el KSS funcional y satisfacción al final del seguimiento fueron mejores en el grupo de pacientes de causa séptica. La supervivencia del implante fue del 95% al final del seguimiento.
ConclusiónLa artroplastia de revisión con implante constreñido varo-valgo es un procedimiento seguro y con buenos resultados a medio plazo independientemente de la causa del recambio.
Primary knee arthroplasty (PKA) gives good results over the long term, with survival rates of 95% at 15 years of follow-up.1 On the contrary, revision arthroplasty gives less consistent results, with survival rates that differ widely between published series and which in some works leads to a failure rate of 60%.1 Nevertheless, the latest series report a 90% success rate due to improvements in the implants and surgical technique.2 In spite of the high success rates of PKA, the increase in the number of operations means that more and more revisions are taking place. In the USA it is estimated that the number of revision arthroplasties will increase up to 6 times from 2005 to 2030.3 The causes of failure include infection, pain or loosening, and they may be determined by situations such as loss of bone reserve or ligament instability, among others.4–8
Septic loosening is one of the most frequent causes of revision.9 Incidence of this has been decreasing as a result of the use of antibiotic prophylaxis and pre- and perioperative control measures.10 However, in spite of the fall in incidence, it is becoming increasingly common to find this pathology due to the high number of operations, increasing patient comorbidity and the recent appearance of multi-resistant germs. Of the different therapeutic options the 2-step change is still the gold standard, with curation rates close to 90%,11 even though there is still no consensus on the type of space, the time between operations or how long antibiotic treatment should last. In spite of these high rates of cure, many works12,13 show that the results of revision TKP secondary to infection are worse than those for revisions with an aseptic cause. These results have been attributed to rigidity after the spacer, poor fixing due to bone defects and soft tissue damage.13
This study compares the clinical and radiological results of revision arthroplasty, differentiating between aseptic and septic causes. A hand-made articulated spacer was implanted in the first surgical operation and the same varus-valgus constrained implant was used.
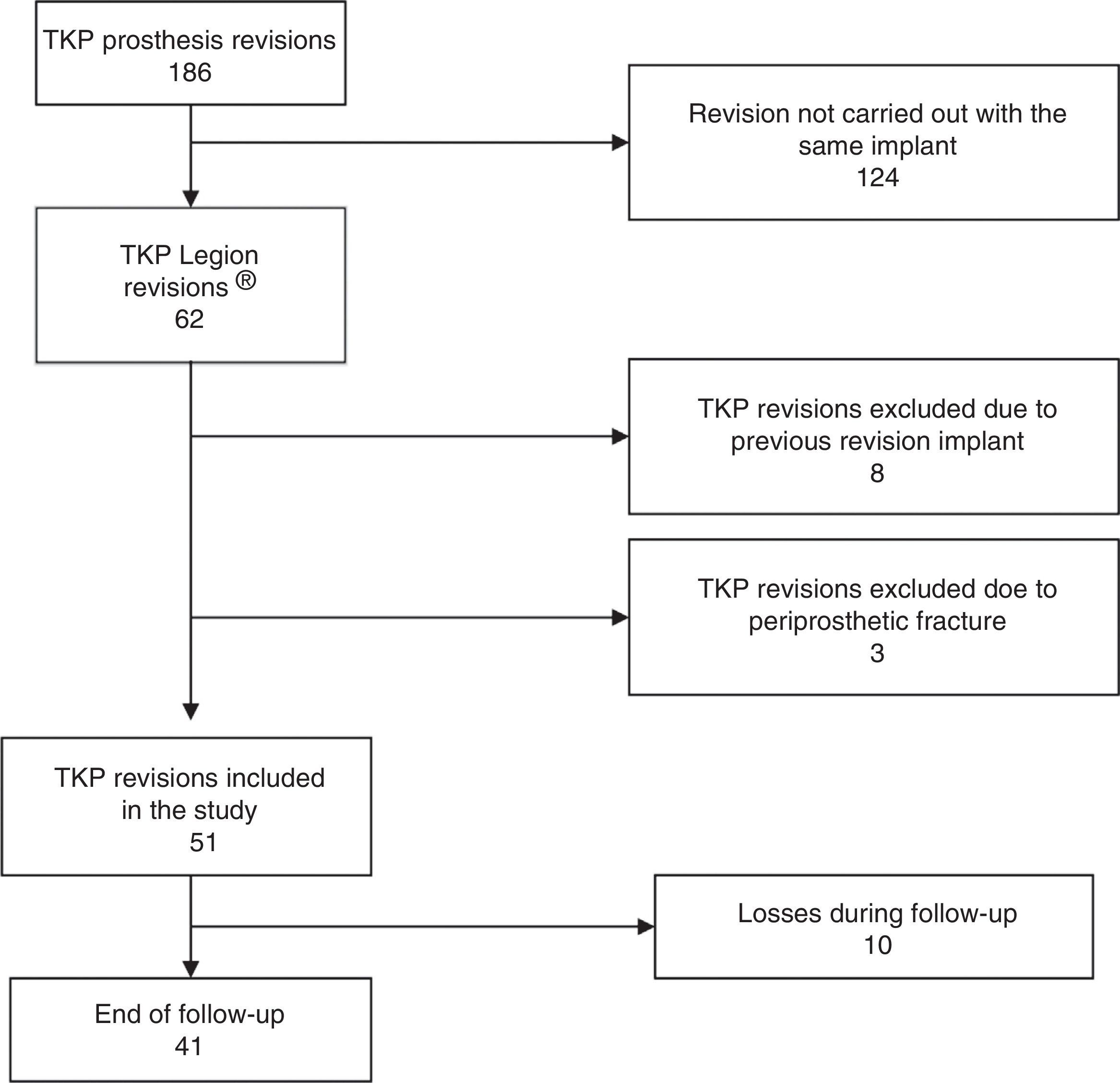
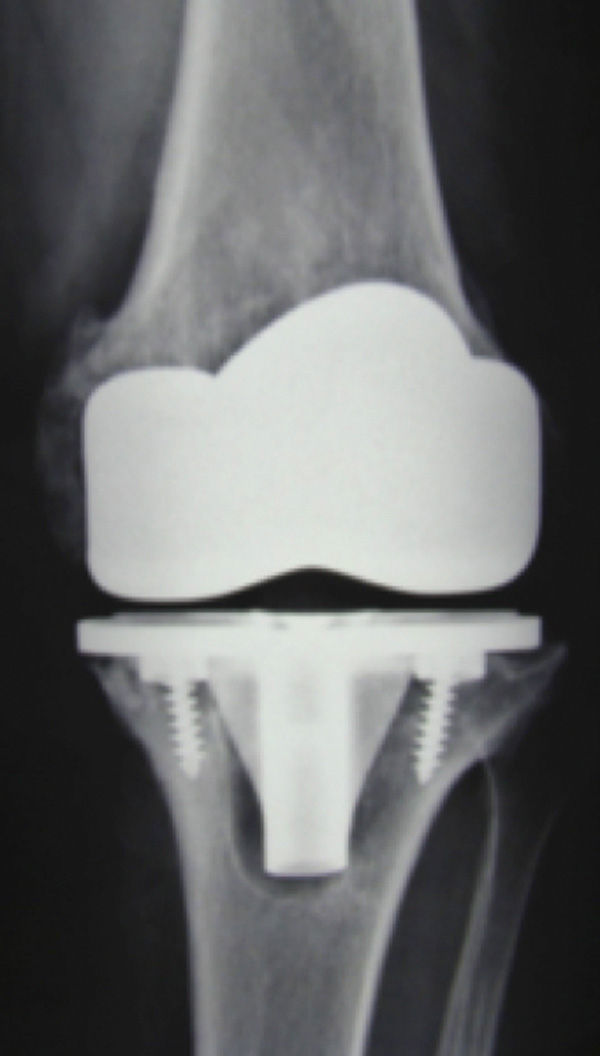
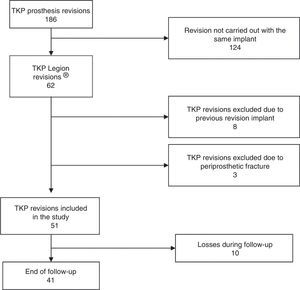
Material and methodsFrom January 2006 to December 2011 a total of 186 knee revisions were performed consecutively in our institution; 62 revisions were selected from these which used the same implant and were performed by 2 senior surgeons. The selected implant was the Legion system (Smith & Nephew, Memphis, TN, USA) with a constrained varus-valgus insert. Eight cases were excluded from the study because a previous revision implant had been used, together with 3 other cases as they presented previous periprosthetic fracture (Fig. 1). The indication for use of the revision prosthesis in the 51 remaining knees included aseptic loosening of the components (Fig. 2), ligament instability, hypersensitivity to the metals and a septic second time of revision. They were divided into 2 groups for the study.
Infection was diagnosed by using the following criteria of the Musculoskeletal Infection Society Workgroup14: (1) the presence of a fistula; (2) isolation of microorganisms in 2 or more tissue or fluid samples, or (3) if 4 of the following 6 criteria were present: high VSG and PCR; raised leukocytes in synovial liquid; a high percentage of polymorphonuclear cells; the presence of pus; the isolation of microorganisms in a tissue or fluid culture; more than 5 neutrophils per magnified field in 5 fields during histological analysis.
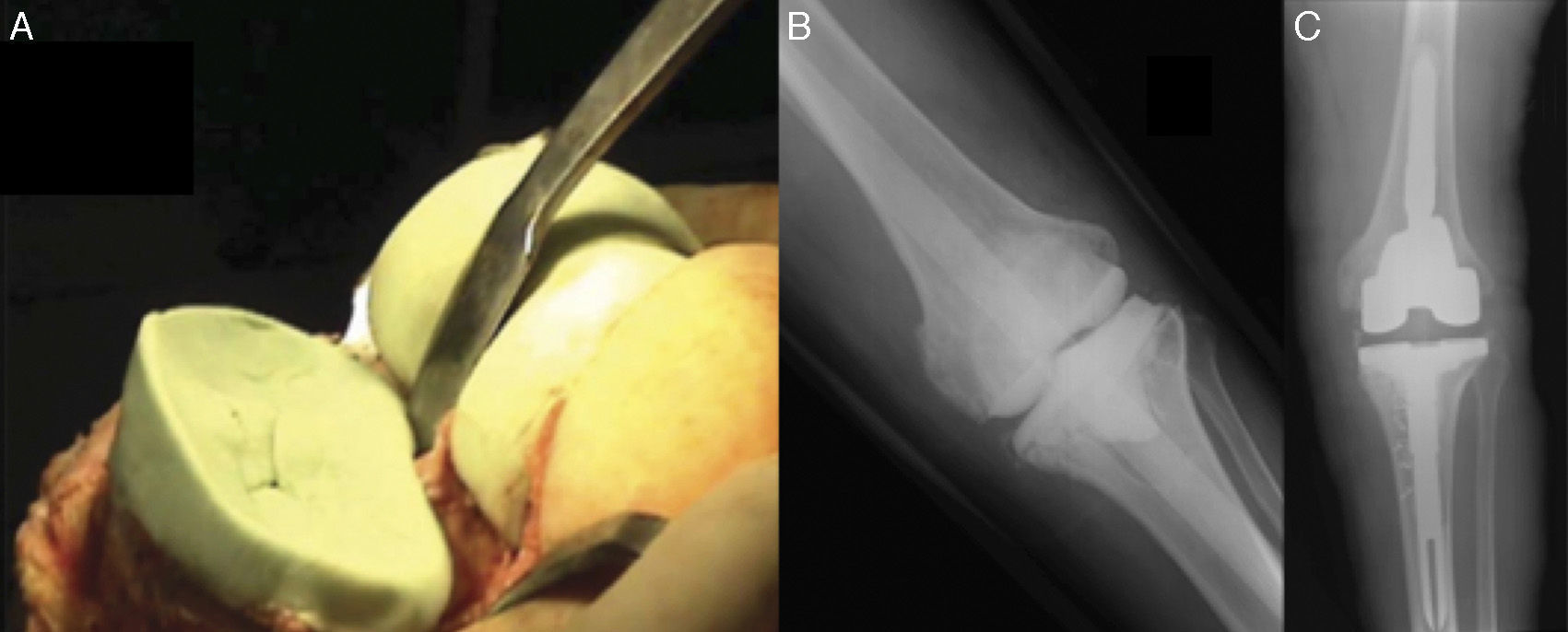
When an infection was confirmed the first surgical operation implanted a hand-formed spacer (Fig. 3).15 Intravenous antibiotic treatment was then given during 2 weeks followed by 4 weeks of oral antibiotic, according to the recommendations of the Microbiology Department and depending on the intraoperative culture. After 2 weeks without antibiotic, and following confirmation of the normalisation of PCR and VSG, arthrocentesis was performed to take samples for culture and, once they had been confirmed as negative, the second surgical operation took place to implant the definitive prosthesis. The average time from the first to the second operation was 72 days (58–96 days).
All data were prospectively entered into a computerised registry. All of the patients were examined by an orthopaedic surgeon not involved in this surgery. Clinical and radiological data were obtained before and after the operation at intervals of one month, 3 months, one year and then annually until the end of follow-up. The average time from the first operation until the revision surgery was 50 months (36–72 months).
Surgical technique: the same surgical technique was used in all cases. Normotensive epidural anaesthesia was used for the operation. The incision was through the previous scar in the mid line, with a medial parapetelar approach. Osteotomoy of the anterior tibial tuberosity (ATT) was performed in 5 cases (4 of which were aseptic) and a quadriceps snip was used in 11 knees (8 of which were aseptic). The operations were carried out with ischaemia of the limb using a pressure hose in the root of the thigh at 300mmHg.
Following extraction of the components while trying to preserve the maximum bone reserve, broad debridement was performed together with washing in saline solution. Protocol required that at least 5 samples were taken during the operation for microbiological culture. Both medullar channels were rasped and the bone surfaces were carefully prepared to obtain the maximum contact surface. The tibia was reconstructed first; then the space when flexed was calculated with a correct femur size. The size of the femoral component is calculated using contralateral X-rays of the knee and the data of the first implant. Prophylactic antibiotic was administered as routine using cefazolin during 24h. In septic cases the hospital protocol was used (teicoplanin+meropenem) until cultures were negative.
Different rod measurements were used for the implants. The most used was the 160mm long femoral rod (59.4%) with a width varying from numbers 11 to 18, and the 120mm tibial rod (66.8%) with a width varying from numbers 9 to 16. Femoral wedges were required in 16 cases (39%) and tibial supplements were needed in 7 cases (17%).
Radiological study: anteroposterior and lateral X-rays were taken of the knee and patella, with telemetry including the head of the femur and the ankle. The X-rays were evaluated by a different observer who was not involved in the operation. Radiolucencies were detected in the digital X-rays, considering radiolucent lines larger than 2mm, following the scheme of the zones in femoral and tibial components according to the modified American Knee Society scoring system.16 The height of the patella was measured in all cases, and the correct position of the articular interline was determined using the preoperative X-rays and multiplying the femoral width by a constant (0.27) which gives us the distance from the proximal limit of the ATT to the articular interline, as described by Servien.17 The axes of the limbs and the alignment of the prosthetic components were also measured, taking femoral and tibial diaphysis as the reference and obtaining data on femoral flexion and valgus and tibial slope and varus.
Clinical results: the clinical results were measured using Knee Society scales (KSS and the functional KSS).18 Results were considered to be poor (<60), mediocre (60–70), good (70–80) or excellent (80–100). Subjective patient satisfaction was calculated using an analogue visual 10 point scale. Patients were grouped into 4 categories19: 0–2 (not very satisfied), 3–5 (fairly satisfied), 6–8 (satisfied) and 9–10 (very satisfied).
Statistical analysisData were analysed using the SPSS-20 statistical package (IBM, Chicago, IL, USA). Variable distribution normality study was based on the Kolmogorov–Smirnov and Shapiro–Wilk tests. Levene's test was used to evaluate the homogeneity of the variables. Comparative analysis of pre- and postoperative results (paired samples) was undertaken using the Student t-test for homogeneous variables and normal distribution, and Wilcoxon's test was used for the rest. The Chi squared test was used for qualitative samples. Survival analysis was undertaken using Kaplan–Meier curves. A value of p<.05 was considered to be a significant difference.
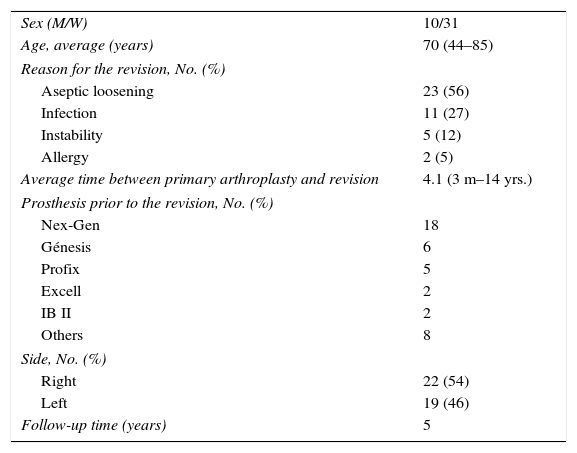
ResultsOf the 51 cases, some were lost in follow-up: 3 cases died due to concomitant causes and 7 cases were lost for other reasons. Forty-one were included in the study (Fig. 1). Twenty two were right knees and 19 were left knees. The average age±standard deviation was 70 years old (43–84±8.61 years old) and 31 cases were women. In stratified analysis of the septic group of patients (11 cases, 26.8%) and the aseptic group (30 cases, 73.2%) no significant differences were found in their demographic data (Table 1). The final average follow-up was 6 years (3.1–8.1 years).
Demographic data.
| Sex (M/W) | 10/31 |
| Age, average (years) | 70 (44–85) |
| Reason for the revision, No. (%) | |
| Aseptic loosening | 23 (56) |
| Infection | 11 (27) |
| Instability | 5 (12) |
| Allergy | 2 (5) |
| Average time between primary arthroplasty and revision | 4.1 (3 m–14 yrs.) |
| Prosthesis prior to the revision, No. (%) | |
| Nex-Gen | 18 |
| Génesis | 6 |
| Profix | 5 |
| Excell | 2 |
| IB II | 2 |
| Others | 8 |
| Side, No. (%) | |
| Right | 22 (54) |
| Left | 19 (46) |
| Follow-up time (years) | 5 |
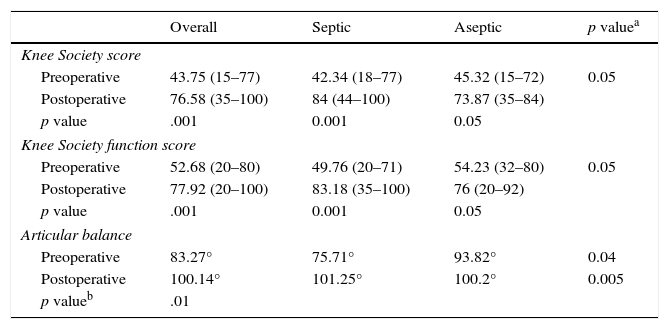
Respecting mobility (Table 2), preoperative average knee flexion was 87.12° (15–120°), average extension was 3.85° (0–30°) and average articular balance was 83.27°. After the operation average flexion was 101.04° (65–115°), average extension was 1.45° (0–25°) and the average articular balance was 100.14°. The average improvement in articular balance is 17°, and this is statistically significant (p=0.01) compared to before the operation. In the septic cases the average articular balance before the operation was 75.71° and in the group with an aseptic cause it was 93.82°, and this difference is significant (p=0.04). After the operation articular balance improved significantly in both groups with an average mobility of 101.25° in the septic group and 100.2° in the aseptic group, without any significant differences between both groups.
Pre- and postoperative functional results.
| Overall | Septic | Aseptic | p valuea | |
|---|---|---|---|---|
| Knee Society score | ||||
| Preoperative | 43.75 (15–77) | 42.34 (18–77) | 45.32 (15–72) | 0.05 |
| Postoperative | 76.58 (35–100) | 84 (44–100) | 73.87 (35–84) | |
| p value | .001 | 0.001 | 0.05 | |
| Knee Society function score | ||||
| Preoperative | 52.68 (20–80) | 49.76 (20–71) | 54.23 (32–80) | 0.05 |
| Postoperative | 77.92 (20–100) | 83.18 (35–100) | 76 (20–92) | |
| p value | .001 | 0.001 | 0.05 | |
| Articular balance | ||||
| Preoperative | 83.27° | 75.71° | 93.82° | 0.04 |
| Postoperative | 100.14° | 101.25° | 100.2° | 0.005 |
| p valueb | .01 | |||
The preoperative average KSS was 43.75 and 76.58 after the operation, with a significant improvement in the KSS scale between the preoperative score and at the end of follow-up (p=0.001). The average preoperative functional KSS was 52.68, and after the operation it was 77.92, once again with a statistically significant improvement (p=.001). When the KSS results are stratified results are good or excellent (KSS>70) in 30 (73%) cases. When they are separated according to the cause of the revision, differences were found in favour of the patients operated due to an infection in terms of their postoperative KSS, functional KSS and level of satisfaction. However, these differences are not statistically significant (p>0.05).
Patients were highly satisfied with the result of the operation at the end of the follow-up period. 80% of patients considered themselves to be satisfied (6–8 points) and very satisfied (9–10 points) on the stratified analogue visual scale. Satisfaction was higher in the group of patients with an infectious cause, although this was not statistically significant.
Limb alignment before the operation was an average of 6° of deformity (0–20), including varus knees (48%), valgus (38%) and ones with a neutral axis (14%). The average deformity measured by telemetry after the revision surgery was 2.55° (0–6). The average improvement was 3.45°, and this is statistically significant (p=0.01). The articular interline was restored in all cases.
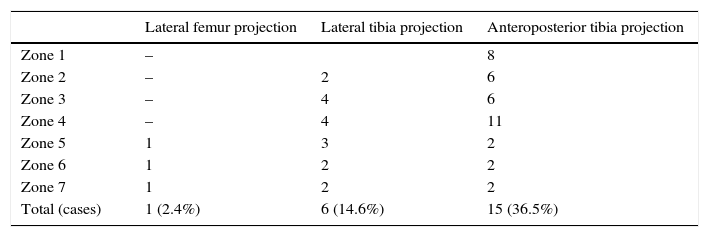
Radiologically the results were satisfactory in 39 cases (95%) while a radiological failure was only found in 2 (5%) cases when one of the components had to be replaced. Nevertheless, radiolucencies were detected in 15 cases (36.5%). Radiolucencies did not appear equally often in all of the implant zones; they were distributed as shown in Table 3. No differences were found between the groups according to the cause of replacement. The results obtained at the end of the follow-up period in terms of component alignment respecting the diaphysis of the bones (average degrees) were: 4.56° of femoral component flexion, 89.5° of tibial component descent, 95.8° of femoral component valgus and 89.8° of tibial component varus. No relationship was detected between these data and the appearance of radiolucencies or component loosening.
A total of 12 cases (29.2%) in our series suffered complications. Complications associated with surgical wound problems amounted to one third of all the complications (33%). The complications that required subsequent surgery were 2 cases of component loosening which required implant replacement, one case of acute infection that was treated by cleaning, debridement and replacement of the mobile parts, one case of pseudoarthrosis of the osteotomy of the tibial tuberosity and one case of tibial tuberosity avulsion. There were no differences between the septic and aseptic cause groups in terms of complications.
Average implant survival during the follow-up period was 95%, and it had to be removed and replaced in only 2 cases in the series.
DiscussionThe results of revision arthroplasty are described in many studies.20–22 In our study we are able to confirm that it is a successful procedure that leads to improved knee mobility, a better KSS, a better functional situation and higher patient satisfaction over the medium to long term (average follow-up of 6 years). Implant survival (95%) was also good after the revision. These results are similar to those in other previous publications on the success rate of revision arthroplasty.23–27 One of the outstanding strengths of this work is that all of the operations used the sample constrained varus-valgus implant.
Although several studies support the use of the least possible constriction,28 different circumstances such as excessive bone deficit, incompetent ligaments or major deformities make it necessary to use implants that are more constrained than is usual.29 A constrained varus-valgus implant was used in all cases of this study. However, although it was more constrained it was not a hinge. This implant was selected subjectively during surgery by an experienced surgeon. The results obtained with this constrained implant were suitable, with 95% implant survival, a 17° improvement in articular balance, achieving an average range running from 1.4° to 100.1°. Postoperative KSS and functional KSS results were very good. Satisfaction was high in 80% of cases. Radiologically alterations in limb axis were corrected in the majority of cases, obtaining correct implant alignment in 95% of the patients. These data are comparable with those of other studies, such as the one by Lee et al.30 with another constrained varus-valgus prosthetic model. An average improvement was obtained in articular range of 12° (95–108°), a KSS of 88 and a functional KSS of 73, as well as similar results in the radiological follow-up.
Two stage revision is the treatment of choice for prosthesis infection.31–35 This technique achieves a high success rate, controlling the infection and returning patients to their functional status. In spite of the good results in terms of infection control, several series show worse results than is the case after revision due to an aseptic cause.13,36,37 Wang et al. show that, in spite of the differences in the clinical results between both groups, 85% of patients express the same level of satisfaction after the process in septic and aseptic revision cases.12 Several factors have been proposed as the reasons for these results, including the restriction in articular balance, preoperative articular dysfunction and fibrosis after repeat operations in patients with an infection.13 More recent studies have shown better functional results in patients treated for TKP infection. After an average follow-up of 40 months Patil et al. showed better results in septic cases in terms of function, although levels of satisfaction were comparable.38 This may be due to the shorter time between implantation of the spacer and re-implantation, together with the increasingly wider use of articulated spacers. Although the latter have only given better functional results in some studies, they have been shown to be useful in preventing larger bone defects and less need to use enlarged approaches.2,33,39,40
In our study the patients with a septic cause commenced with a lower articular balance than the aseptic cases (p<0.05). Nevertheless, their articular balance improved more after surgery, when it equalled or surpassed those of the aseptic cases (although the difference is not significant). In the case of the KSS and functional KSS evaluation scales, the results at the end of the follow-up were better in those cases when revision had a septic rather than an aseptic cause, although this difference was not statistically significant. The authors believe that this is due to the systematic use of articulated spacers and patient collaboration, as they realised the importance of keeping the operated knee mobile, as well as the short time between the spacer and replacement implant. The use of standardised protocols in multidisciplinary management and the importance of achieving negative infection parameters have also been postulated as causes of these good results.38 Others have associated them with the low virulence of certain microorganisms.11 Regarding patient satisfaction, after the revision surgery it may be said that it was higher in the group of patients with a septic cause, although this difference was not statistically significant.
In our series complications arose in a total of 12 cases (29.2%). This is similar to the 26.3% published by Saleh et al.21 and slightly higher than the figure in other works.41 Complications in connection with surgical wound problems account for a third of the total number of complications (33%). There were 2 cases of implant loosening that required further surgery to replace them, one case of acute infection that was treated by cleaning, debridement and replacement of the mobile parts, one case of pseudoarthrosis of the osteotomy of the tibial tuberosity, and one case of tibial tuberosity avulsion. There were no differences between replacements in the septic and non-septic cause groups.
This study has a series of limitations. Firstly, although the clinical and radiological data were analysed prospectively there was no randomisation. Secondly the cohort is too small to allow stronger statistical analysis. Thirdly, possible distortion may occur as this is a referral hospital. To try to avoid this, those patients who had already been operated in another hospital were excluded, as well as patients with previous revisions. In spite of these factors our results are comparable with other recently published works that show similar results for septic and aseptic revisions.
The strengths of this study are the homogeneity obtained with a single surgical technique and implant, as well as the fact that the same constrained insert was used in all cases. All of the cases were operated in the same institution by 2 senior surgeons. Postoperative data were gathered using a single protocol in the attempt to reduce any possible distortion. Our study also offers results after a long average follow-up of 6 years.
To our knowledge this is the first study to offer functional and radiological results as well as patient satisfaction with the same constrained implant, comparing septic and aseptic cases, and with follow-up over the medium term.
To conclude, revision arthroplasty with a varus-valgus constrained implant is a safe procedure that gives good results over the medium term regarding functionality, patient satisfaction and implant survival. These results do not depend on the cause of prosthesis replacement, and it was found that correct treatment of the infection led to comparable or even better results for the revision than aseptic cases. Nevertheless, it must not be forgotten that this procedure gives rise to a large number of complications requiring multidisciplinary management in referral centres with experience in handling them. We believe that a multicentre study would be necessary to increase the robustness of the results obtained, making it easier to generalise the conclusions.
Level of evidencePrognostic evidence level III.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments in human beings or animals were undertaken for this research.
Data confidentialityThe authors declare that they followed the protocols of their work centre for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gil-Martínez P, Sanz P, López-Torres I, Arnal-Burró J, Chana F, Vaquero J. Influencia de la causa de revisión en el resultado tras revisión protésica de rodilla con implante varo-valgo constreñido. Rev Esp Cir Ortop Traumatol. 2016;60:184–191.