There currently is a considerable variability in the content of training programs and courses for orthopaedic surgeons in training. Besides this, there is still no consensus regarding which is the most effective methodology for improving learning of the technique or for its qualitative evaluation. A study was carried out to assess the influence of carrying out a cadaveric practical course on the acquisition of arthroscopic technical skills in fifth-year residents.
MethodsA knee arthroscopy cadaveric course was performed in which forty-eight students participated. Different technical aspects during a knee arthroscopy, as well as the residents skill and the execution time were evaluated before and after the course using a specific questionnaire.
ResultsThere was a significant statistic improvement between the initial and final evaluation, increasing from 11,7 till 17,1 (maximum 20) points. Also, a significant improvement in all the parameters analysed was observed; the identification of anatomic structures, the palpation and the time necessary for the arthroscopic knee check (P = ,001, P = ,032, P = ,015 respectively).
ConclusionA knee arthroscopy cadaveric course improves significantly the technical skills of surgeons in training.
Existe una gran variabilidad en los contenidos de los programas y cursos de capacitación artroscópica para cirujanos ortopédicos durante su etapa de formación. Cabe destacar que no hay consenso en cual es la metodología más efectiva ni como debería realizarse la evaluación cualitativa de los mismos. Se llevó a cabo un estudio con el objetivo de evaluar qué influencia tiene la realización de un curso cadavérico práctico para el desarrollo de habilidades artroscópicas en residentes de quinto año.
Material y métodosSe realizó curso práctico de artroscopia de rodilla en cadáveres, donde participaron 48 alumnos. Previo al comienzo y tras la finalización del curso se llevó a cabo una evaluación práctica, donde se recogieron en un cuestionario específico diferentes aspectos técnicos al realizar una artroscopia de rodilla, así como la destreza y el tiempo de ejecución.
ResultadosSe obtuvo una mejoría estadísticamente significativa, evolucionando de una puntuación inicial de 11,7 a 17,1 (para un máximo de 20) puntos tras la evaluación final. La mejoría en cada uno de los parámetros de manera aislada también fue significativa; la identificación de estructuras anatómicas durante el recorrido artroscópico básico (P = ,001), la palpación de estructuras específicas (P = ,032) y el tiempo necesario para completar el recorrido artroscópico (P = ,015).
ConclusionesLa realización de un curso práctico de artroscopia de rodilla en cadáver permitió mejorar significativamente las habilidades técnicas de los cirujanos en formación.
Arthroscopic surgery is one of the most widely used surgical techniques in the usual practice of orthopaedic surgeons. It takes a long time to learn arthroscopic technique, and this is a challenge for teachers and students alike.1,2 During the learning process it is not uncommon for lesions to be caused by surgeons’ lack of experience. As well as increasing patient morbidity, this also means that the learning process is sometimes said to be inefficient in terms of time and economic cost.3,4
There is currently no international agreement on the application of a training plan, in terms of its contents or learning methodology, such as practice on cadavers5 or virtual simulators,6 or on how these technical skills should be evaluated.7
A study was conducted with the aim of evaluating the degree to which arthroscopic skills improved in a group of 5th year residents after a practical course using cadavers. It also evaluated their surgical experience prior to the course, and how this influenced the initial evaluation of the practice.
Material and methodsA practical course on knee arthroscopy in cadavers was organised during 2 consecutive years by the Spanish Knee Society (SEROD). 24 students took part in each course, which were identical in format. Each course lasted for 2 days, with a total of 11 teaching hours. The latter were divided into 1.5 h for general considerations, 3.5 h for meniscal pathology, 4.5 h for plasty extraction and reconstruction of the anterior crossed ligament (ACL) and 1.5 h to execute extra-articular plasties.
A total of 48 students took part in the courses. They were residents in Orthopaedic Surgery and Trauma in 12 Autonomous Communities in Spain. The selection/participation criteria included being a 5th year resident and the order of inscription. All of the participants accepted taking part in the evaluation, and they signed an informed consent document before being included in the study.
Each student was assigned a random number from 1 to 24 at the start of the course, with the aim of maintaining their anonymity during data gathering in the previous survey and practical pre- and post-course evaluation.
Previous surveyBefore the start of the practical part, each student answered an anonymous questionnaire to describe their previous level of training. The items recorded in this survey were:
- 1
Months of rotation in the knee unit of their hospital.
- 2
They were asked whether in the Department where they were residents a routine and basic arthroscopic examination was included at the start of arthroscopic knee surgery (YES – NO).
- 3
The total number of knee arthroscopies they had performed as the first surgeon.
- 4
Type of arthroscopic surgery (arthroscopic examination, meniscectomies, meniscal sutures, ACL plasties).
An initial evaluation took place at the start of the course, with a second evaluation immediately after the end of the same. Both evaluations were performed at 3 work stations. 3 course teachers with wide experience in arthroscopic technique worked as evaluators, having received instruction for this. The same evaluating teachers took part in both courses. Students were assigned to evaluating teachers at random in both courses, and the evaluator was unaware of the result of the initial evaluation. A cadaveric knee selected beforehand by the course directors and with all of its anatomic structures intact was used in each work station. The 3 knees used for the initial evaluation were replaced by 3 others for the final evaluation. The anterolateral and anteromedial arthroscopic portals were created beforehand by the teacher.
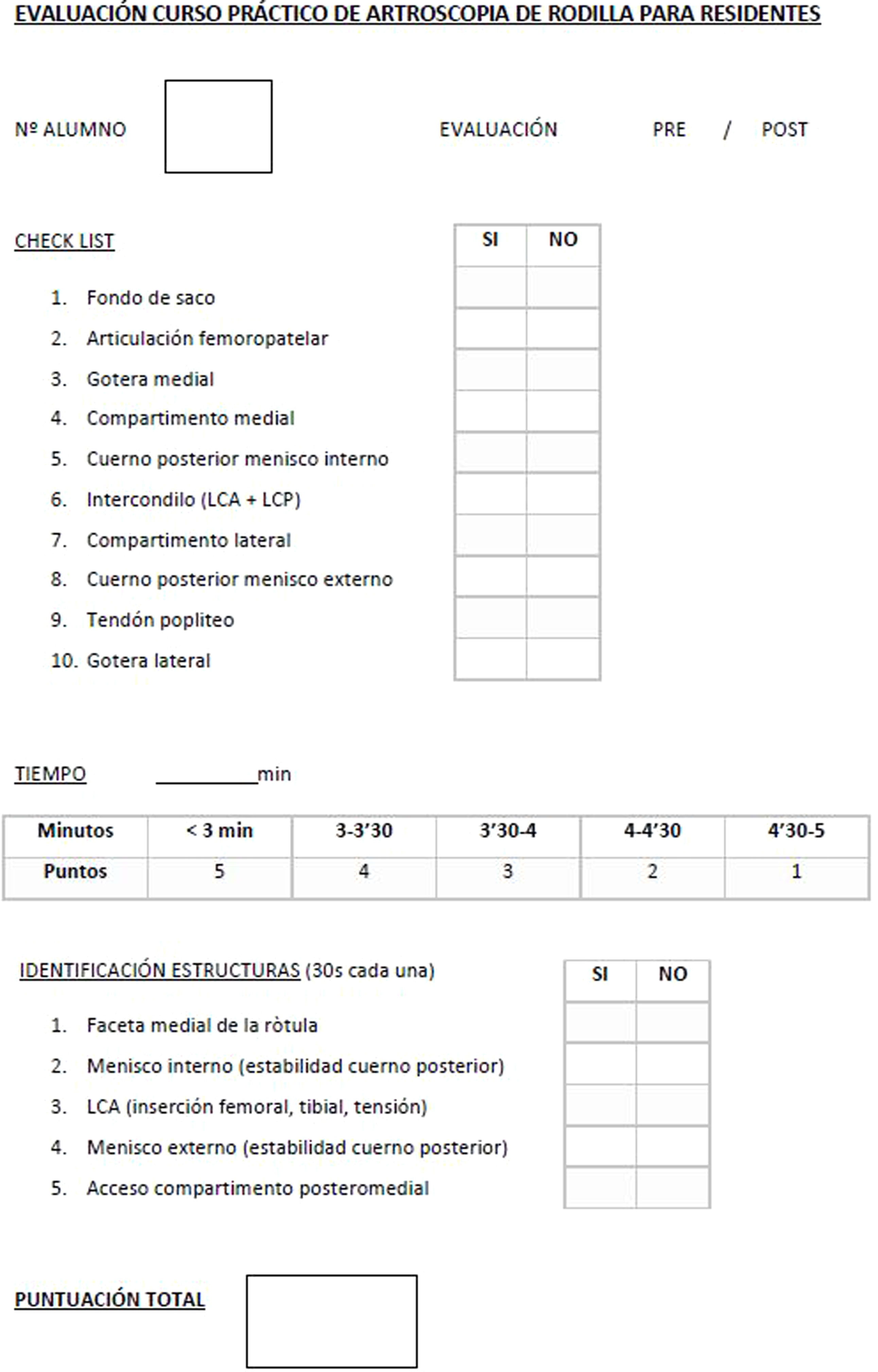
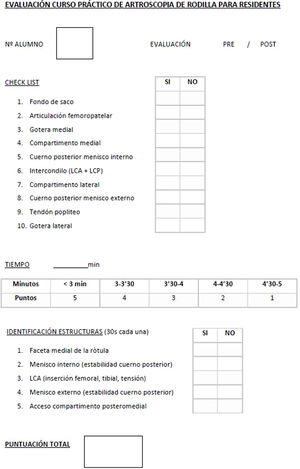
A modified version of the basic arthroscopic skill scoring system described by Insel et al.8 was used for technical evaluation. Students firstly had to identify 10 anatomical structures included in the usual basic examination. The student had to recognise them and centre them in the visual field of the monitor (1 point was awarded for each structure identified). The time needed to complete the examination was also recorded (from 0 to 5 min, awarding 5 points if the student took less than 3 min. and subtracting a point for every 30 s that elapsed until a maximum of 5 min, when the examination ended. Finally 5 knee structures were specified that the student had to recognise and touch with the specific arthroscopic instrument (one point for each structure). The total score was obtained by summing scores from the 3 sections, and it could vary from 0 to 20 points (Fig. 1).
The SPSS v.19.0 (IBM, Chicago, IL) statistical package was used for analysis. Descriptive analysis of each variable was performed in an initial phase. Core tendency measurements (average and median) were calculated for the quantitative variables, as well as dispersion (standard deviations [SD] and range) according to normal distribution. The calculations corresponding to qualitative variables were shown in the form of frequency (absolute number) and percentage. The Kolmogorov-Smirnov test was used to determine the normal distribution of variables. The Student t-test was used for the analysis of quantitative variables corresponding to independent data and normal distribution; otherwise the non-parametric test or Mann-Whitney U test was used. To study the effect of one or more independent variables on a dependent variable a variance analysis was performed, assuming normal distribution of the sample and homoscedasticity. Statistical significance was assumed if P < .05.
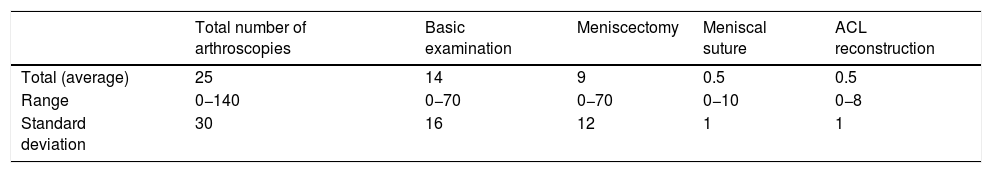
ResultsShort questionnaire2 participants in the second course joined it late due to reasons of transport/mobility, so they were excluded from the study. The 46 residents included in the study had rotated through the knee unit in their respective hospital during an average of 8−5 months (in a range of 3–20 months, SD 4), performing an average of 25 knee arthroscopies as the first surgeon (range 0−140, SD 30). In 78% of the cases the participants undertake a systematic arthroscopic examination prior to the specific treatment to be performed, while 9% do not do this and 13% did not answer this point. The other results are shown in Table 1.
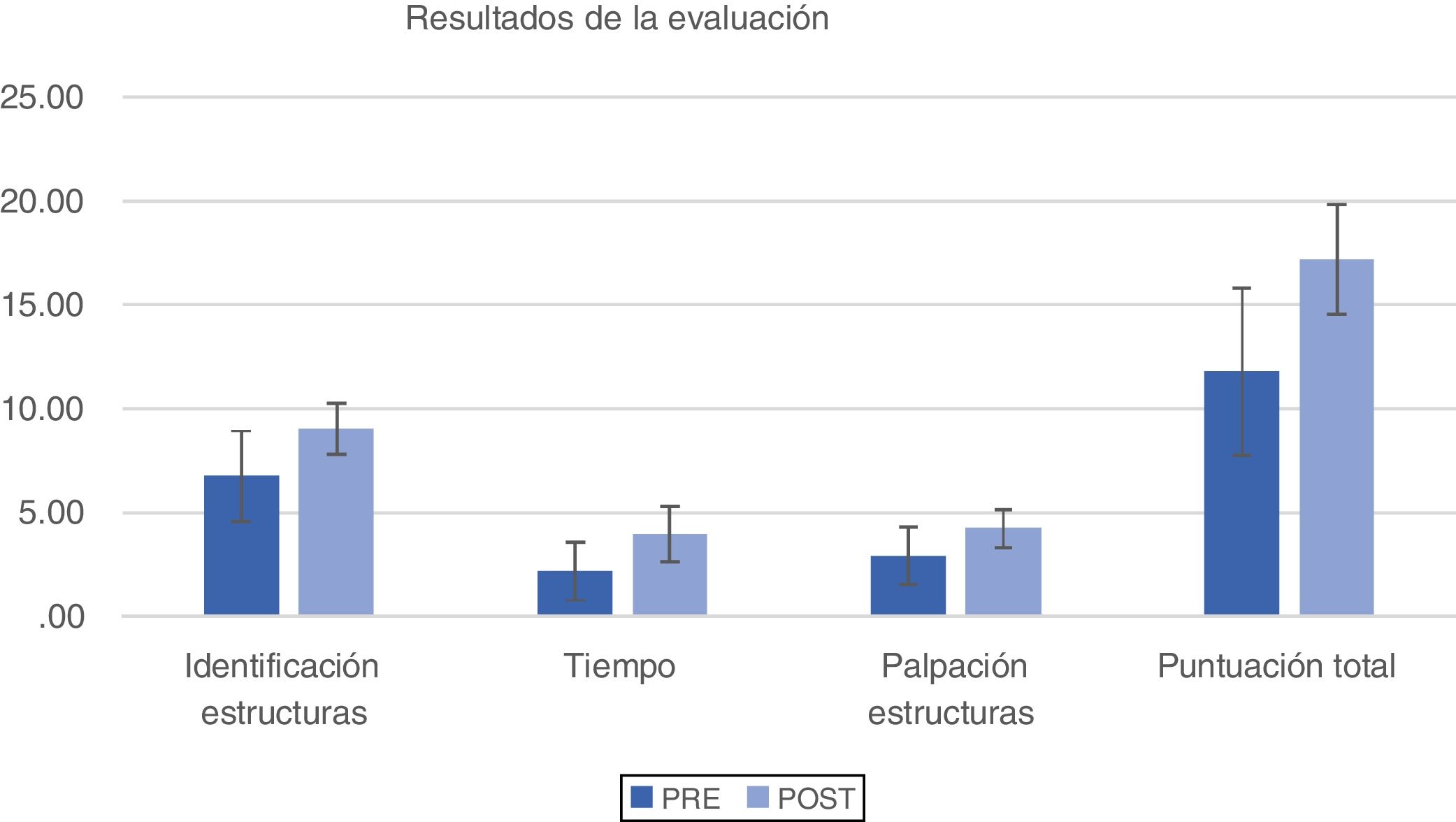
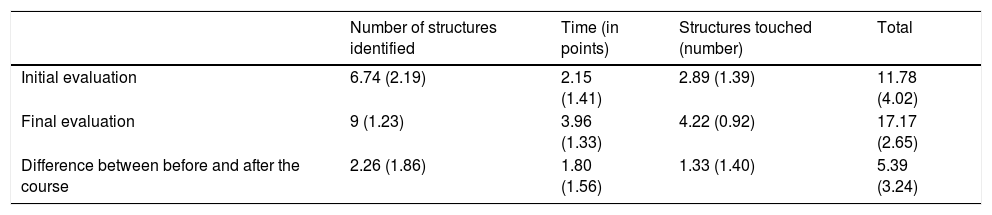
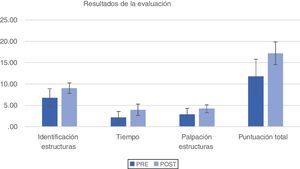
Practical evaluationTable 2 shows the results obtained in the evaluations before and after the course, as well as the degree of improvement that was found (Fig. 2).
Results of the different evaluations during the course. The score obtained is shown as an average (standard deviation).
| Number of structures identified | Time (in points) | Structures touched (number) | Total | |
|---|---|---|---|---|
| Initial evaluation | 6.74 (2.19) | 2.15 (1.41) | 2.89 (1.39) | 11.78 (4.02) |
| Final evaluation | 9 (1.23) | 3.96 (1.33) | 4.22 (0.92) | 17.17 (2.65) |
| Difference between before and after the course | 2.26 (1.86) | 1.80 (1.56) | 1.33 (1.40) | 5.39 (3.24) |
A statistically significant improvement was obtained in all of the analysed parameters: identification of structures during the basic arthroscopic examination (P = .001), the time taken to perform the same (P = .015) and the identification and touching of specific structures (P = .032).
When the results obtained in the initial practical evaluation were analysed, a statistically significant relationship was found between the results of this initial evaluation and the months the student had spent in the knee unit of their hospital (P = .023) as well as the number of arthroscopies they had performed prior to the course (P = .04).
No significant relationship was found between the performance or not of the basic arthroscopic examination and the total score of the evaluation before the course (P = .17).
DiscussionThe chief finding of this study is the significant improvement observed in all of the parameters analysed by the practical evaluation of the residents before and after the course.
The identification of different structures during the basic arthroscopic examination, the time taken to perform the same and the touching of specific structures improved after the course, and the overall improvement amounted to almost 40%. The time taken to perform the basic arthroscopic examination and the improvement in technical skill in touching structure were the points where the course had the greatest impact.
These results show that practice using cadaveric knees is relevant for the arthroscopic training of residents, as was shown by Raja et al., who found gradual improvement in the residents after they had undergone a specific training program.9
The importance of this type of practice in developing arthroscopic skills was supported by a survey of more than 2400 members of the American Academy of Orthopaedic Surgeons (AAOS).10 This study concluded that practice using cadavers is the second most important factor in developing the necessary skills for the arthroscopic repair of a broken rotator cuff. According to the results of this survey, only undertaking a training program in sports medicine and arthroscopy was superior to practice using cadavers. In turn, a study by Koehler et al. found that specialists as well as residents identified practice using cadaveric models as the most effective form of the same, considering it to be the gold standard. A negative finding of this study was that not all of the residents had access to this training tool.11 The use of virtual reality simulators was in third place of the academic activities that could be undertaken for the same purposes. These stimulators were also found to be useful by other authors, for the shoulder as well as the knee.12,13
The results of the survey before the course on the arthroscopic experience of the respondents varied widely, ranging from 0 to 140 procedures performed, with an average of 25 arthroscopies. According to these results of the pre-course survey, this group of surgeons could be classified as at a basic level according to the system of Insel et al., who recommend that at least 20 arthroscopies have to be performed to acquire the minimum skills and thereby correctly perform a basic arthroscopic examination. The authors reach this conclusion after surveying resident tutors and advanced arthroscopy course directors.8 Moreover, different studies establish the need to have performed 150–200 knee arthroscopies to be able to properly carry out an ACL reconstruction.14,15
There is sufficient evidence to justify holding cadaveric courses for students at this level of skill, as the improvement obtained is statistically significant in comparison with those who did not attend such a course.16 Additionally, skills are acquired during practice with cadavers twice as quickly as is the case when simulators are used. Nevertheless, it should be pointed out that the use of simulators during 300 h/year make this method more effective in cost/benefit terms compared with cadaveric practice.17
In spite of the variability observed within the study group, an association was found between the number of arthroscopies performed and the results of the initial evaluation. The residents who had performed more arthroscopies during their training gained higher scores. These findings are similar to those described in the literature, where different authors also associate a lack of experience with poorer initial results, which gradually improve with increasing practice.8,14,18
Although the sample size is insufficient to establish differences between autonomous communities or different hospitals, the existence of knee arthroscopy training plans may help to reduce the observed disparity.
On the other hand, the group studied was highly homogeneous when describing the type of procedures they had performed before the course. These were mainly grouped into simple procedures such as arthroscopic examination and meniscectomies, while hardly any had performed more complex procedures such as meniscal suture or ACL reconstruction.
As different studies state, it is indispensable to evaluate skills and technical abilities to improve residents’ learning. The scores obtained at the end of this course show that acquiring basic concepts and skills necessitates continuous practice of surgical technique with the requisite instruments.5,14
This study has a series of limitations. The residents came from different hospitals within Spain and they had followed different training programs, giving rise to major variations in their experience of arthroscopic technique. On the other hand, an evaluation technique was used which had been validated but also modified to adapt it to the specific practice to be performed, based on evaluation of the basic skill of triangulation and touching specific structures. In future courses it would be justified to add evaluation systems for specific techniques to improve the analysis of the results. Finally, it has to be taken into account that performing multiple arthroscopies on a single cadaveric knee may alter the difficulty of the procedure. It was attempted to minimise this aggression by using 3 different knees in the evaluation and replacing them between the first and final evaluations.
ConclusionsTaking a practical cadaveric course makes it possible for orthopaedic surgeons in training to significantly improve their technical skills in knee arthroscopy. The time they spend in rotation in the specific knee unit and the number of arthroscopies they have performed as the first surgeon influence the achievement of a better result in the initial evaluation of the residents.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the Spanish Knee Society (SEROD) for its role as the main driver of these training courses and this study.
We would also like to thank Marta Banqué for her help in the statistical analysis of the study.
Please cite this article as: Erquicia JI, Gil González S, Barrera Sancho A, Hernández Fernández G, Pelfort López X. Impacto de las prácticas cadavéricas en la formación artroscópica de rodilla de los residentes de Cirugía Ortopédica y Traumatología. Rev Esp Cir Ortop Traumatol. 2021;65:41–46.