Pain treatment for patients with hip fracture has been based on the use of nonsteroidal anti-inflammatories and opioid derived drugs. These medications have been associated with multiple adverse effects. Fascia iliaca block is a recent pain management alternative for these patients.
The objective of this study was to evaluate the effectiveness of fascia iliaca block performed in the emergency room (ER) for patients over 65 years of age with hip fracture.
Materials and methodsA cohort of 216 patients, from January to December 2016, was studied prospectively. Analysed variables were pain upon arrival at ER, pain after fascia iliaca block, need for rescue medication, protocol compliance, delay in analgesia administration and delay for surgery.
ResultsDifferences between visual analogue scale (VAS), before and after the fascia iliaca block, were statistically significant (p<.001). Pre-block VAS recorded was 6.16 (SD=2.82). The mean VAS reduction after the block was 2.99 (95% CI: 2.45–3.53%). Twenty-six percent of patients required morphine as rescue medication in the first 8h after diagnosis. Compliance with protocol administration was of 84%. Fascia iliaca block was performed in a mean time of 16min (SD=10.33) after diagnosis. The median delay for surgery was 1 day (RIQ 25–75%: 1–2).
ConclusionFascia iliaca block is a reproducible, safe and effective technique for pain management. It is a keystone in pain treatment for patients with a proximal femur fracture at our institution. Other objectives in our pain management protocol include early analgesia administration and reduction of time to surgery.
La analgesia en pacientes con fractura de cadera se ha basado en la utilización de antiinflamatorios no esteroideos y opiáceos, que se asocian a múltiples efectos secundarios. El bloqueo iliofascial es una alternativa analgésica relativamente novedosa en el tratamiento del dolor de estos pacientes.
Nuestro objetivo es evaluar la eficacia analgésica del bloqueo iliofascial realizado en Urgencias a pacientes mayores de 65años con fractura de cadera.
Material y métodosEntre enero y diciembre de 2016 fueron estudiados prospectivamente 216 pacientes. Las variables analizadas fueron: dolor al llegar a Urgencias y después del bloqueo, necesidad de rescate, cumplimiento del protocolo, demora en la administración de la analgesia y demora para la cirugía.
ResultadosSe observaron diferencias estadísticamente significativas entre los valores de EVA antes y después del bloqueo (p<0,001). La puntuación EVA media pre-bloqueo fue de 6,16 (DE=2,82). Tras el bloqueo, la disminución media de la EVA fue de 2,99 (IC95%: 2,45-3,53%). El 26% de los pacientes recibieron morfina de rescate en las primeras 8h. La tasa de cumplimiento del protocolo analgésico fue del 84%. El bloqueo se administró en 16mins de media (DE=10,33). La mediana de demora para intervención quirúrgica fue de 1día (RIQ 25-75%: 1-2).
ConclusiónEl bloqueo iliofascial es una técnica analgésica reproducible, efectiva y segura. Constituye un pilar fundamental en la estrategia analgésica de los pacientes con fractura de cadera en nuestro centro. Los otros dos pilares incluyen la analgesia precoz y la disminución de la demora para la intervención quirúrgica.
Life expectations of the population at large are increasing every year. From 2010 to 2040 the world population over 65 will double and will account for 14% of the worldwide population. This increase will come about more rapidly in developed countries and there will be more people with osteoporosis, leading to a greater number of fractures as a result.1 Hip fractures are of greater relevance due to their high incidence and their associated morbidity and mortality. In 1990 there were 1.6 million hip fractures worldwide and it is estimated that this figure will increase to 6 million in the year 2050.2
Most patients with hip fractures present with intense pain on their arrival at the emergency department, and effective pain control is an essential objective in any hospital.3 However, insufficient analgesia is a constant in both North American and European hospitals. Pain is not correctly assessed, the powerful analgesics are underused and delay in treatment initiation is commonplace.4
According to the Spanish Society of Pain the mean time for receiving analgesia is 43min.5 The standard of the Royal College of Emergency Medicine in United Kingdom is that 100% of patients with moderate or severe pain must receive analgesia during the first hour they are admitted to the emergency services.6
Badly controlled pain, particularly in elderly patients, is associated with a higher risk of suffering from delirium, longer hospital stays and a worse quality of life.7
The treatment of pain in these patients has traditionally been based on the use of non steroid anti-inflammatory drugs (NSAIDS),8 which often have renal, cardiovascular and gastrointestinal side effects, or with opiates,9,10 which are also associated with many side effects (nausea, constipation, confusion), particularly in elderly patients.11–13
Regional anaesthesia is an alternative for better treatment of pain and for reducing the consumption of NSAIDS and opiates. Fascia iliaca block is a relatively novel analgesia technique for pain control in elderly patients with hip fractures.14 The National Institute of Health and Care Excellence (NICE) recommends considering the use of a neurological block in these patients.15
Fascia iliaca block provides effective pain management, is easy to perform and is associated with a very low risk of adverse effects.16–18
In Spain there is no extended use of fascia iliaca block as an analgesic treatment in elderly patients with a hip fracture. However, the recent appearance of multidisciplinary orthogeriatric units which include anaesthetists may promote the introduction of this analgesic technique.
The Orthogeriatric Unit of our Hospital established an acute pain control protocol in patients who were admitted to the emergency department with proximal femoral fractures. The early administration of analgesia, fascia iliaca block and the performance of surgery within 24h were the three main keystones.
The objective of this study was to assess the analgesic efficacy of fascia iliaca block performed in the emergency department on patients over 65 years of age with a clinical diagnosis of fracture due to the fragility of the proximal femur.
The duration of the effect of the fascia iliaca block and the rate of compliance with this analgesic technique, together with analysis of delay in administration of the analgesia and delay for surgery were secondary objectives of this study.
Material and methodsThe analgesic protocol of the patient with a proximal femoral fracture due to fragility includes the fascia iliaca block since its approval by the Orthogeriatric Unit, in June 2013. It is administered on arrival at the emergency department prior to diagnostic imaging tests. The fascia iliaca block is performed without the use of a neuro-stimulator, or ultrasound guide, by the trauma resident doctors and attending physicians who received the patient. All patients who received fascia iliaca block were recorded prospectively.
Inclusion criteriaPatients who were 65 years of age or older with a clinical diagnosis of a proximal femoral fracture and who did not present with any of the exclusion criteria were included.
Exclusion criteriaPatients being treated with oral anti-coagulants were excluded from treatment, and also those who presented with allergies to local anaesthesia, who had skin infections at the inoculation site and minimum pain on arrival at the emergency department on the visual analogue scale (VAS) ≤2.
TrainingPrior to the introduction of this analgesic technique, the residents and attending physicians of the orthopaedic and trauma surgery unit were given training on how to perform the block by the Anaesthesia Department. This training consisted of a theoretical session and in performing the block during surgery supervised by an anaesthesia assistant.
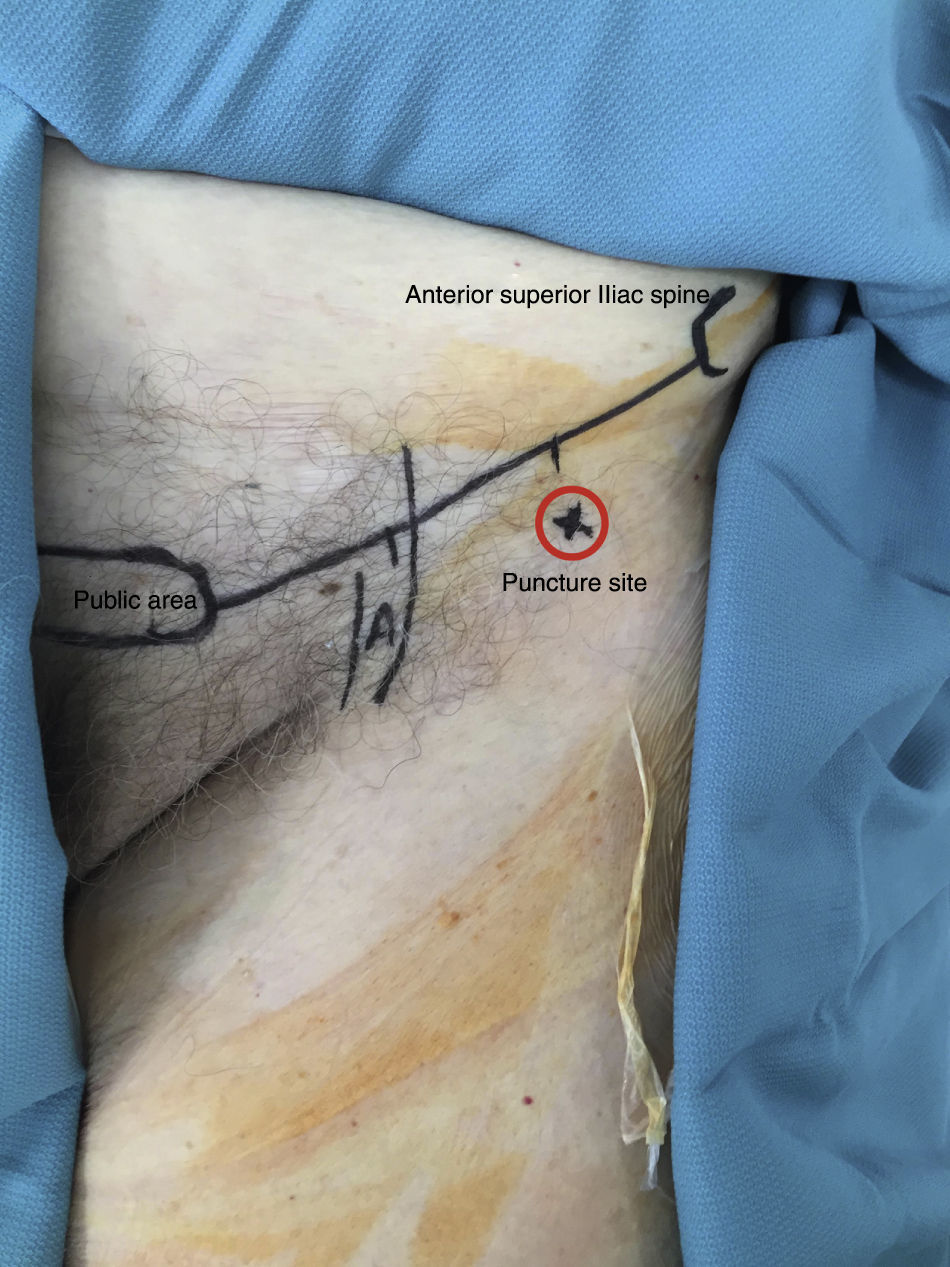
Technique and analgesiaThe technique of administration is that described by Dalens et al.19 A line is drawn from the pectin pubis to the anterior superior iliac spine and then divided into three equal parts. For safety's sake it is always a good idea to feel the femoral artery, which normally occupies the most medial third of the line. The puncture site is located laterally to the neurovascular bundle, at a safe distance from it, right between the middle part and the lateral part and approximately 2cm distal to this line (Fig. 1).
Puncture is made with an 18G Tuohy needle, since its angled point enables resistance to be detected with greater ease. Once it has passed through the skin it has to overcome its first resistance which is the fascia lata (normally at this point we would recommend an inclination of the needle of 70°, in caudocraneal direction, with respect to the patient's skin. The second resistance is the fascia iliaca. Once this has been overcome, we would recommend increasing the approach angle of the needle to 30–40° and inserting it by 1cm more, approximately. Once this virtual space has been reached and with prior suction to ensure that the tip of the needle is not inside a vessel, we proceed with the injection of 0.3ml/kg of levobupivacaine at 0.25%. The volume of the deposited local anaesthetic has cephalad spreading and enters into contact with the femoral nerve, the femorocutaneous nerve and lastly the obturator.
Once the block has been administered 1g of intravenous paracetamol every 8h and 3mg of subcutaneous rescue morphine is administered, with prior pain evaluation by the nurse, in accordance with the VAS.
VariablesThe following variables were recorded:
- 1.
Pain on arrival at the emergency department and 15–30min after having had the block, valued on the VAS or the PAINAD scale (in patients with mental impairment).
- 2.
The need to administer rescue analgesia and the VAS of the patient at the time of administration.
- 3.
Compliance with the analgesic technique.
- 4.
Delay in analgesia administration.
- 5.
Delay for surgical intervention.
- 6.
Patients’ age.
- 7.
Sex.
- 8.
Anaesthetic risk according to the American Society of Anesthesiologists (ASA).
- 9.
Type of fracture.
The VAS is an effective tool for measuring the intensity of pain. It consists of a horizontal line measuring 10cm where symptom extremes are expressed at both ends. On the left is the absence of pain or low pain intensity (usually described as “no pain”) and on the right that of the greatest intensity (usually described as “the worst pain imaginable”). The patient is invited to mark a point along this line which corresponds to the level of pain intensity they are feeling at that time. The result is the distance in millimetres from 0 to that marked by the patient.20
The Pain Assessment in Advanced Dementia (PAINAD) scale contains non-verbal aspects. It is composed of five elements: breathing, negating, facial expression, body language and capacity for relief. Each element is given a score on the scale, and the total scores may range from 0 (no pain) to 10 (intense pain), equivalent to those of the VAS, with the following cut-off points: 1–3 (mild pain), 4–6 (moderate pain) and 7–10 (intense pain).21
Statistical analysisA descriptive analysis was made of the sample. The quantitative variables were expressed as means and standard deviation, and the categorical variables as frequencies and percentages. For comparison of qualitative variables, the chi-square test was used and for comparison of means the Student's t-test was used for independent or paired data, in keeping with the ANOVA test.
A p value under 0.05 was established for a bilateral significance for statistical contrasts. The SPSS 17.0 (SPSS Inc., Chicago, IL, U.S.A.) programme was used for statistical analysis.
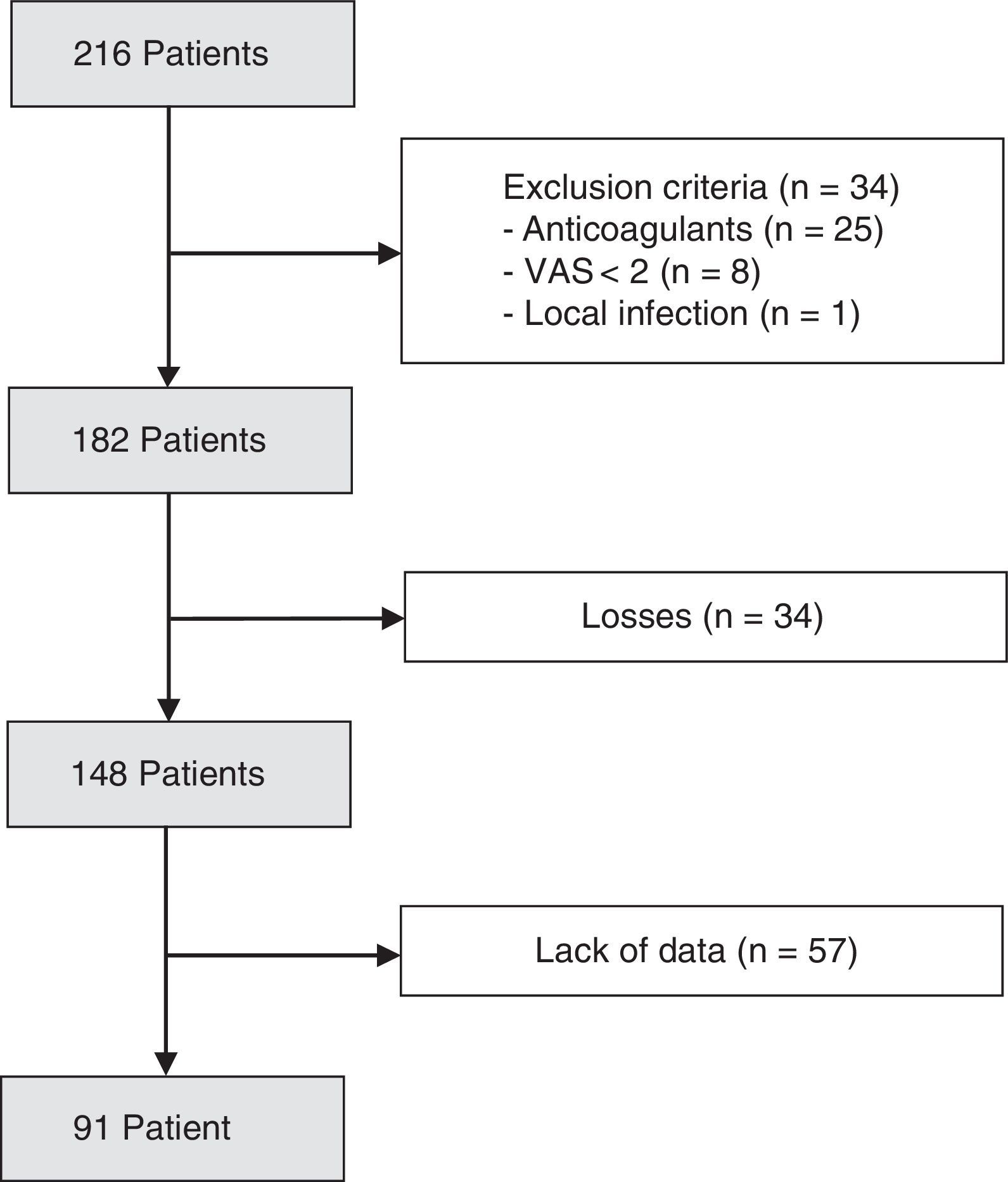
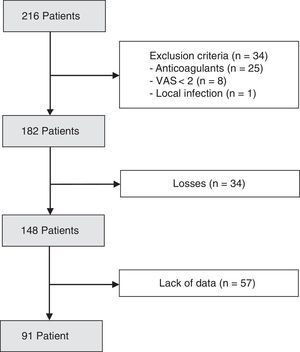
ResultsDuring a period of one year (January–December 2016), 216 patients were admitted to our emergency department with the diagnosis of a proximal femoral fracture. The data which enabled us to analyse the effectiveness of the fascia iliaca block were collected from 91 patients (Fig. 2).
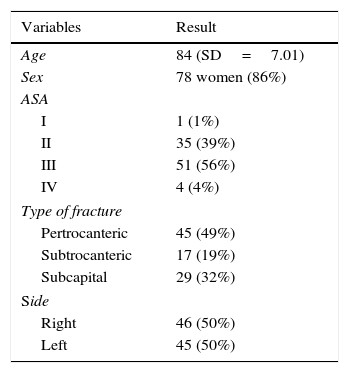
Patient sample characteristics where the effectiveness of the block is analysed are contained in Table 1.
The mean age of patients was 84 (SD=7.005) and over three quarters of patients (86%) were female. 56% of patients presented with an ASA III anaesthetic risk. Proximal femoral fractures were extra capsular in 62 cases and intra capsular in 29.
Statistically significant differences were observed between the VAS values before and after performing of the block (p<0.001). The mean pre-block VAS was 6.16 (SD=2.82). After the block the mean VAS was 2.99 (95% CI: 2.45–3.53%).
45% of the patients received rescue morphine at some time during the 24h in the hospital and in 26% of cases it was necessary to administer it under 8h after the block administration 80% of the patients presented with a VAS over 3 when they were administered the morphine. The mean duration of the analgesic effect of the fascia iliaca block was 6.5h (SD=3.8).
The compliance rate of the analgesia protocol was 84%, with the block being administered in 148 patients (Fig. 2).
The block was administered, on average, in 16min (SD=10.33).
The median delay for surgical intervention was 1 day (RIQ 25–75%: 1–2).
DiscussionThe introduction of the fascia iliaca block as analgesic treatment for the patient who presented with a fracture of the femoral at the emergency department is valid, safe and effective.
For Reavley et al.,17 both the fascia iliaca block and the 3-in-1 block are equivalent in the reduction of the VAS points in patients with femoral neck fractures. As a result they believe the emergency department staff may trust in this analgesic technique.
Godoy Monzón et al.18 report similar results, for whom the fascia iliaca block is as effective as the NSAIDS, particularly for the first 8h after its administration. In their study they emphasise that use of the fascia iliaca block has enabled the disuse of narcotics, thereby preventing their deleterious effects. Similarly to Reavley et al., they consider that the block leads to faster pain control in the emergency department. In our series narcotics were not necessary in 55% of cases.
Chaudet et al.22 not only refer to the effectiveness of the block but also underline that its administration in the emergency department on the patient's arrival is particularly beneficial. Up until 2015, with the exception of Foss et al.16 and Luger et al.,2 the majority of published studies refer to the administration of the block during the postoperative period. However, the most recent publications now defend the usefulness of its administration at the stage prior to surgery.16–18,22,23
Finally, Callear and Shah14 suggest that all hospitals which receive patients with proximal femoral fractures should have an established clinical guideline which includes regional anaesthesia in its pain control strategy for patients. Their study suggests that a single administration of the block in the emergency department, when the patient arrives, reduces the needs for the administration of analgesics during the whole postoperative period.
The NICE recommends taking into consideration the use of the neurological block under two circumstances:
- 1.
When paracetamol or opiates do not provide sufficient pain relief.
- 2.
To limit opiate administration.
According to this guide, the recommendation of paracetamol administration every 6h was necessary and the administration of rescue opiates. NSAID use is not recommended.15
The learning curve for the block technique is very short. In our hospital we consider it necessary to give previous training to the professionals who will be performing the blocks.
In the study by Foss et al.16 all researchers were resident anaesthetists with an average experience of one year. They had received standard training in the practice of neurological blocks, but had had no specific training in fascia iliaca block administration.
For the Danish researchers Høgh et al.24 the learning curve is very simple, and therefore the fascia iliaca block is practised by any resident doctor in the emergency department, after a short training session.
Lastly, the article by Obideyi and the fascia iliaca block administered by trained nurses is of relevance.25
We did not observe any complications relating to the administration of the fascia iliaca block in patients. Reavley et al.17 explain that the anatomical references for the performance of the block may be easily identified, as is the location of the inoculation site which is at a safe distance from the neurovascular bundle. There is minimum risk of intravenous inoculation from anaesthesia or the probability of neurological injury. Specifically the risk recorded from neurological injury is .03%.26 Sporadic cases have been published on the associated complications of a defective administration of the fascia iliaca block. Shelley and Haldane27 published one case of an injection in the retroperitoneum. Atchabahian and Brown28 published a case of transitory neuropathy and Blackford and Westhoffen29 published a case of accidental puncture of the bladder. Godoy Monzón et al.18 described in some cases the appearance of small skin blisters at the inoculation site minor skin.
The fascia iliaca block was effective 15min after administration, although after 7h its effect began to wane. In the randomised prospective study by Godoy Monzón et al.18 highly significant pain relief was felt 15min after administration of the block compared with that of NSAIDS, although the effect began to wane 8h after administration.
In our series, 26% of the patients required the administration of rescue morphine less than 8h after block administration. The percentage of effective blocks was 74%. Foss et al. present an effective block percentage of 67%, which they consider low compared with other previous studies, where the effective block percentages were higher (81–96%).16,30,31 This lower percentage of effective blocks is attributed to the fact that although the administration technique is relatively simple, there is a minor learning curve, and in their block study, they were not administrated by a limited number of specialists. In our series there was also a major variability between the professionals who had used the technique.
Ultrasound-guided block administration and the placing of continuous infusion catheters could improve effectiveness and duration of the analgesia.22,32,33 However, in our opinion both procedures increase the complexity of the technique and limit the number of specialists who may practice it. For this reason, we do not consider these as valid alternatives for the administration of early analgesia in emergency services. Both could, however, be used in postoperative analgesia.
The compliance rate of the new strategy was high (84%), which shows that the involvement of this analgesic technique had a considerable impact on the specialists who had administered it in the emergency department. Although pain treatment is a basic clinical practice, in patients with hip fractures it is often insufficient, incorrectly assessed, powerful analgesics are underused and delay in treatment is common.11
In the study by Hwang et al.34 36% of patients with hip fractures and who stated they were in pain in the emergency department did not receive any type of analgesia, 7% received non-opioid analgesic drugs and the remaining 57% received opiates.
As previously mentioned, the fascia iliaca block is one of the three keystones upon which our analgesic strategy is based. The second keystone is early administration. Once the patient presents at the hospital the block is immediately administered, based on clinical diagnosis and prior to carrying out imaging studies. The patients receive the analgesia after an average of 15min. We therefore complied with the Royal College of Emergency Medicine in United Kingdom standard in that 100% of patients with moderate or severe pain receive analgesia during the first hour after their arrival at the emergency department.6 We improved the 43min mean waiting time for patients in Spanish hospitals to receive analgesia.5
Early administration has also been reflected in other articles,17,35 and is mainly explained by the following mechanisms:
- 1.
Because it can be carried out on clinical suspicion of proximal femoral fracture prior to imaging studies.16
- 2.
Because it is a simple technique to put into practice which may be carried out by the professionals who normally work at the emergency department, without the need to locate specialists who are often unavailable.24
- 3.
Because it is not necessary to use a scan to perform it, which could delay its administration, require specific training in ultrasound and increase the cost of the procedure.17
Lastly, the third keystone of the analgesic strategy is early surgery. Most patients were referred to surgery during the first to 24h.
In 2011 The Association of Anaesthetists of Great Britain and Ireland published a guideline for proximal femoral fracture management. The third point of the summary is that surgery is the best analgesic for a hip fracture.36
Early surgery, in under 48h, is not only performed for analgesic reasons of course. It is currently the treatment base strategy for hip fracture patients, since numerous retrospective studies have reported a report in mortality and complications of patients who are not operated on as soon as possible. This is therefore one of the most essential objectives of the orthogeriatric units and the fast-track protocols in proximal femoral fracture patients.37
ConclusionThe fascia iliaca block is a reproducible, effective and safe analgesic technique. Its learning curve is short, administration technique is simple and there is a very low risk of adverse effects. All of these factors promote its administration to the patient on arrival at the emergency department with consequent early and effective analgesia as a result.
The fascia iliaca block is an essential keystone in the analgesic strategy of hip fracture patients. The other two keystones of this strategy are early analgesia and reduced delay to surgery.
Level of evidenceEvidence level IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestAll the authors declare that there is no type of conflict of interests which could have weighted or influenced their actions or the study outcome.
Please cite this article as: Castillón P, Veloso M, Gómez O, Salvador J, Bartra A, Anglés F. El bloqueo iliofascial en el tratamiento analgésico de la fractura de cadera del anciano. Rev Esp Cir Ortop Traumatol. 2017;61:383–389.