The aim of this study was to evaluate the association of the anatomical and functional characteristics with therapeutic failure in patients with femoroacetabular impingement, who underwent hip arthroscopy.
Materials and methodsA cohort study was performed on 179 patients with femoroacetabular impingement who underwent hip arthroscopy between 2004 and 2012. The demographic, anatomical, functional, and clinical information were recorded. A logistic regression model and ANCOVA were used in order to compare the described characteristics with the treatment outcomes of the hip arthroscopy.
ResultsThe median time of follow-up for symptoms was 13 months (8–30), and the mean time of follow-up after surgery was 23.83±9.8 months. At the end of the follow-up 3.91% of the patients were considered as a therapeutic failure. The WOMAC score in pain and functional branches, as well as the total WOMAC score, showed significant differences (p<0.05). The mean WOMAC score was higher (0–100 with 0 being a perfect score) in the group of patients who failed after surgery as compared with the group who meet the requirements for a successful treatment, 65.9 vs 48.8, respectively (mean difference 17.0; 95% CI; 1.3–32.6; p=0.033).
ConclusionThe poor functional state prior to arthroscopic treatment of femoroacetabular impingement, mainly due to preoperative pain, assessed using the WOMAC scale, is associated with a higher therapeutic failure rate.
Evaluar la asociación entre las características anatómicas y funcionales y el fracaso terapéutico de la cirugía artroscópica en pacientes con choque femoroacetabular (CFA).
Materiales y métodosSe realizó un estudio de cohorte que incluyó a 179 pacientes adultos con diagnóstico de CFA sometidos a artroscopia de cadera entre 2004 y 2012. Se obtuvo información demográfica, clínica, anatómica y funcional para determinar si ocurrió fracaso del tratamiento. Se utilizó un modelo de regresión logística y un análisis de covarianza para comparar las características anatómicas y funcionales con el resultado del tratamiento artroscópico.
ResultadosLa mediana del tiempo de evolución de los síntomas fue de 13 meses (8-30) y el tiempo de evolución posquirúrgico fue en promedio de 23,83±9,8 meses. El 3,91% presentaron fracaso del tratamiento. La puntuación en la escala de WOMAC en el dominio de dolor y capacidad funcional, así como su puntuación global, mostraron diferencias significativas (p<0,05). La media de la puntuación de WOMAC total también fue mayor (0 a 100, siendo 0 una puntuación perfecta) en el grupo de fracaso en comparación con el grupo de éxito del tratamiento, 65,9 vs. 48,8, respectivamente (diferencia de 17,0; IC del 95%, 1,3-32,6; p=0,033).
ConclusiónEl pobre estado funcional previo al tratamiento artroscópico del CFA principalmente en la esfera de dolor preoperatorio, evaluado mediante la escala WOMAC, se asocia a mayor índice de fracaso terapéutico.
In some cases, pain in non-arthritic hips is associated to anatomical alterations of the acetabulum (pincer type deformity), the femoral neck (cam type deformity) or both (mixed deformity), which added to cyclical mechanical loads or lesions caused during physical activity derive in damage to the labrum or cartilage.1–3 This condition, known as femoroacetabular impingement (FAA), is probably the main cause of osteoarthritis (OA) in non-dysplastic hips.4–6 The association between labral lesions and a history of FAA in 90% of cases has led to early interventions in order to avoid the progression of degenerative changes.7,8
The etiology of the typical anatomical deformities of FAA is still controversial.9 The theories put forward include evolutionary changes,10 predisposing diseases, like proximal femoral epiphysiolysis,11,12 and genetic factors,13 among others.
Despite the presence of anatomical deformities typical of FAA, some epidemiological studies have determined that the onset is not associated to symptoms in nearly 4.3% of males and 3.6% of females.14 The absence of studies which clearly associate OA with asymptomatic FAA is the reason why the current trend is to intervene patients only when they present pain, related or not to physical activity.9 In 2013, Agricola et al. found an association between OA and an alpha angle over 60°, with a greater association as the measurement increased, and finding the greatest association among patients with 83°.15 Nevertheless, all the patients in that study were symptomatic, so the scenario of patients with anatomical configurations compatible with FAA but without symptoms and developing OA remains unexplored.
Conservative treatment is currently accepted as the initial intervention for all patients. However, its effectiveness in terms of functional improvement or modification of the natural history of the degenerative changes has not been proven so far. Therefore, surgical treatment in patients with symptoms acquires great relevance in order to alleviate pain, improve functional condition, shorten the return to physical activity and prevent degenerative changes on the labrum and cartilage.9
The correction of the alterations described can be carried out through open, arthroscopic or mini-anterior arthroscopy-assisted surgery. Open surgery involves a controlled dislocation of the hip, which makes the procedure technically demanding and, due to factors inherent to the technique, may entail complications such as nonunion of the trochanteric osteotomy, osteonecrosis of the femoral head, heterotopic ossification and persistent weakness of the abductor musculature.16,17
Arthroscopic and assisted mini-anterior treatments avoid the need to dislocate the hip, but they also require maneuvers, like prolonged traction and liquid infusion, that can cause transient neuropraxias and extravasation of fluid to the abdominal cavity in some cases.18 Nevertheless, both with the open technique and arthroscopic and assisted procedures, the rates of complications are increasingly low due to the increasing experience of surgeons, as well as an improved selection of patients.18
Recent studies have proven that these techniques have similar rates of effectiveness,19,20 with reduction of pain and improvement of function in between 68 and 96% of patients,21 but with an advantage for arthroscopic or assisted treatment regarding the rate of return to activity among high-level athletes.19 These studies have assessed treatment failure in two ways: through the need for a new surgical procedure in the affected hip and through the use of different scoring scales intended for this purpose.
Some studies of effectiveness have shown as a secondary result that patients with advanced age and OA prior to the procedure were associated with poor results. However, no published studies have determined other anatomical or functional factors related to failure of the surgical treatment, which can reach up to 32% of cases9 after controlling for confounding factors. One study demonstrated failure in 12% of patients with no presence of OA,22 thus indicating the existence of other characteristics determining failure of arthroscopic treatment, in addition to the previously identified variables.
Elucidating these characteristics would enable a reduction in the frequency of surgical treatment failure, establishing predictive variables which helped to select patients for arthroscopic hip treatment, due to the clarity obtained in terms of patients who would truly benefit from the intervention.
The objective of this study was to evaluate the association of anatomical and functional characteristics with therapeutic failure of arthroscopic surgery in patients suffering FAA.
Materials and methodsWe conducted a predictive study which included 179 patients with FAA, who were intervened at Clínica Las Américas (Medellín, Colombia), by one of the authors (WM), between the years 2004 and 2012, to assess the association of anatomical and functional characteristics with therapeutic failure of arthroscopic surgery in patients with FAA.
SubjectsWe included patients with ages between 17 and 66 years with a diagnosis of FAA, who underwent arthroscopic hip surgery, with at least 1 year of postoperative follow-up. We excluded patients with a history of congenital or acquired hip disease other than FAA (Perthes disease, hip dysplasia, fracture and epiphysiolysis), those with a prior history of hip surgery and those who presented radiographic findings compatible with hip OA greater than grade i in the Tonnis scale.23
DiagnosisThe diagnosis of FAA was established in patients with hip pain who did not respond to nonsurgical treatment and had positive findings for pincer or cam type FAA.
All patients included presented the typical clinical manifestations and radiographic findings of FAA, which were identified through hip radiographs and arthrography by magnetic resonance.
Hip radiographRadiographic findings were determined through anteroposterior projection of the pelvis and axial Johnson projection of the proximal femur, supervised by the same surgeon (WM) and conducted according to the standards recommended by the literature, similarly to the measurement of the alpha angle and center edge angle (CE),24 assessing the deformity of the femoral head and acetabular overcoverage, respectively, which in turn determined the type of impingement.
Arthrography by magnetic resonance (arthro-resonance)The arthrographies were conducted at 3 different centers in the city by similar processes; injection of the intraarticular contrast medium enabled the intraarticular hip components to be delimited, as well as the condition of the labrum and acetabular cartilage to be established. These were interpreted by the radiologists at each of the centers and verified by the surgeon (WM) so as to determine the condition of the structures examined.
Surgical procedureArthroscopic hip interventions were conducted by the same surgeon on an outpatient basis, under general anesthesia. In addition, a femoral block was carried out to control postoperative pain. An orthopedic table was used in all cases, with the patient in the supine position and a large perineal post (standard for protected hip traction). The intervened hip was positioned at 25° abduction, extension and neutral rotation. A traction test was conducted prior to creating the portals.
After verifying the arthroscopy equipment and the 30° and 70° lenses (Arthrex®, Florida, USA), as well as the irrigation system, the anterolateral and anterior portals were created using the inside-out technique. The diagnosis of intraarticular lesions was established initially, and then corrected according to their indication.
Anatomical characteristicsThe lesions of the joint cartilage and labrum were assessed through arthro-resonance according to the McCarthy classification.25 Presence of chondral lesion was determined by stages 3 b and 4 of this classification.
The findings in the arthroscopic procedure, as well as the interventions conducted during the procedure, were considered as exposure variables; the presence of an acetabular cyst, microfractures, chondroplasty, resection or reinsertion of the labrum, osteoplasty, acetabuloplasty and tenotomy of the psoas were verified in the intraoperative records of patients.
The procedures were conducted by the same surgeon (WM) in all cases.
Functional characteristicsThe scores of the Western Ontario and McMaster Universities (WOMAC) scale in its total LK3.0 version and the different domains, validated for Spanish,27 were considered to determine the condition of the affected hip prior to the arthroscopic procedure.26 The overall result of this scale was scored from 0 to 100. In the WOMAC scale, a result of 0 is the best possible and 100 is the worst possible.
The scale was applied to patients by one of the authors (WM), between 1 and 4 weeks prior to the surgical procedure. Although the validation was conducted in patients with OA, who were excluded from our study, familiarity with this scale and the similar performance of other scales used to assess functionality among young patients, such as the modified Harris hip score (MHHS), non-arthritic hip score (NAHS) and hip disability and osteoarthritis outcome score,28–30 made the WOMAC scale an adequate option for the evaluation of these patients.
Follow-upFollow-up was started on the same date the arthroscopic procedure was performed, until the final assessment of the condition of each patient. All patients were monitored for at least 1 year and no additional controlled interventions were carried out during this period. All invasive procedures conducted on the intervened hip were approved by patients. The final evaluation verified the presence of a new surgical procedure on the intervened hip and other important clinical and sociodemographic characteristics through an instrument designed for this purpose. This questionnaire was completed through personal interviews, e-mail or telephone, between March 2012 and February 2013.
The outcome measured was failure of the arthroscopic treatment of the affected hip, defined as: (1) need for a new arthroscopic procedure, and (2) open surgery of the hip, or both.
When indicated, open surgery was conducted by a different surgeon, after consultation with the surgeon who conducted the arthroscopies (WM). The revisions of arthroscopies were always conducted by the same surgeon, author of this article. The indication was persistence of pain or limitation of movement.
Statistical analysisA sample size of 123 subjects was calculated, taking into account that exposure factors would be present in 25% of the subjects suffering failure of the arthroscopic treatment, an OR of 3.8, 95% confidence interval (CI), a 3:1 ratio and a power of 70%. The software package Epidat version 4.1, of the Pan American Health Organization (PAHO), was used for the analysis.
The description of the nominal variables was conducted through proportions, and of the quantitative variables through means and medians, according to the previously established type of distribution.
The differences in quantitative variables between patients who did or did not suffer failure of the arthroscopic treatment were evaluated using the Student t test or the Mann–Whitney U test, depending on the type of distribution. The chi squared test of independence for categorical variables or the Fisher exact test for dichotomous variables were used to evaluate the association of variables included with the presence of failure of the arthroscopic treatment.
We conducted a binomial logistic regression analysis to evaluate the association between the anatomical characteristics and the presence of failure of the arthroscopic treatment. We adjusted the model for age and gender, presenting the results in OR and their respective 95% CI. The association between the functional variables and the outcome was evaluated through analysis of covariance (ANCOVA) after verifying the statistical assumptions. We obtained the mean scores in the different categories of the WOMAC scale, adjusted by age and gender according to the result of the arthroscopic treatment (failure versus success).
The analyses were carried out with the software package SPSS, version 21.0, and with a level of statistical significance of 5%.
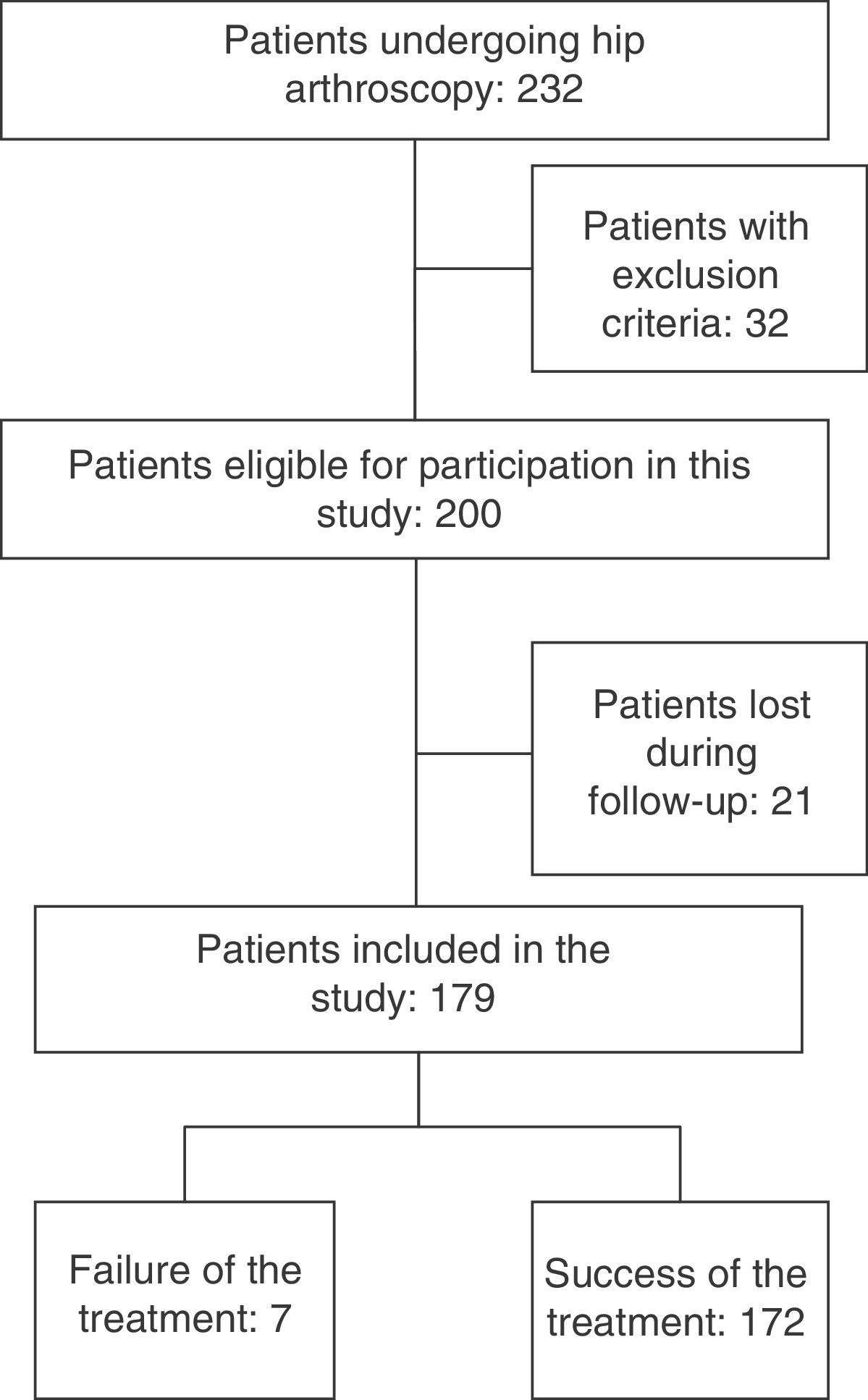
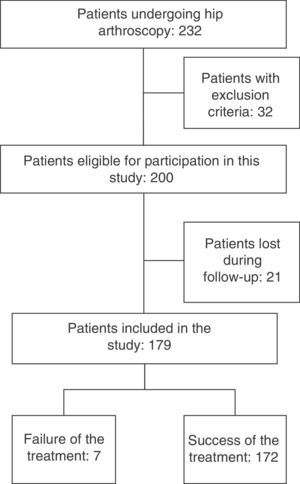
ResultsOut of a total of 232 patients who underwent hip arthroscopy between January 2004 and February 2012, we included 179 patients who fulfilled the criteria defined and who had a full follow-up. A total of 32 patients were excluded; 28 of them due to some grade of hip arthritis prior to the procedure, 1 due to prior fracture of the intervened hip and 2 due to avascular necrosis.
Out of the 179 patients included and with a full follow-up, 69 were evaluated through a telephone survey, 78 through a personal interview and 32 by e-mail. It was not possible to contact 21 patients (10.5%), so they were considered as losses for the study (Fig. 1). The final scores in the WOMAC scale were not taken into consideration in the final analysis of results.
Out of the patients included, 3.91% presented failure of the treatment. This corresponded to 7 patients, of which 3 presented pincer type, 3 cam type and 1 mixed. A total of 35.2% were males, the mean±standard deviation values for age were 43.7±10.4 years, for BMI 23.8±4.2kg/m2, and for overall score in the WOMAC scale prior to the procedure 50.7±19.1. The majority of patients were from a medium-high socioeconomic background, represented by levels 4 and 5, 23.3 and 30.5%, respectively. Regarding laterality of impingement, it appeared on the right side in 40.6% of cases, on the left side in 48.3% and was bilateral in 11% of patients. Depending on the type of impingement, 44.9% of subjects presented cam type, 13.5% presented pincer type and 41.5% presented a mixed type.
The median time of evolution of the symptoms was of 13 months (P25–P75: 8–30) and the mean time of postoperative evolution was 23.8±9.89 months. Regarding the radiographic characteristics of impingement, we found alpha angles and CE angles with mean values of 59.9±6.39° and 36.6±8.02°, respectively.
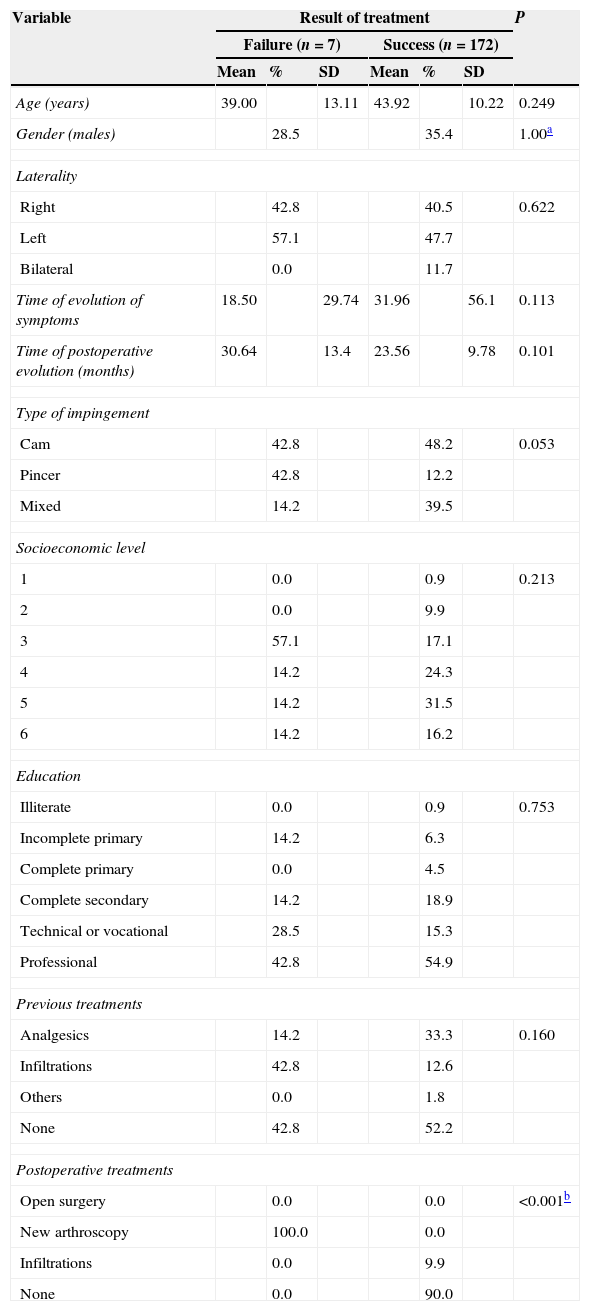
No differences were observed in the clinical and sociodemographic characteristics of patients included in the study, with the exception of presence of interventions subsequent to treatment, where the performance of a new arthroscopic procedure was more prevalent among the failure group (Tables 1a and 1b).
Description of the demographic and clinical characteristics according to the result of arthroscopic surgery obtained among patients with femoroacetabular impingement.
| Variable | Result of treatment | P | |||||
|---|---|---|---|---|---|---|---|
| Failure (n=7) | Success (n=172) | ||||||
| Mean | % | SD | Mean | % | SD | ||
| Age (years) | 39.00 | 13.11 | 43.92 | 10.22 | 0.249 | ||
| Gender (males) | 28.5 | 35.4 | 1.00a | ||||
| Laterality | |||||||
| Right | 42.8 | 40.5 | 0.622 | ||||
| Left | 57.1 | 47.7 | |||||
| Bilateral | 0.0 | 11.7 | |||||
| Time of evolution of symptoms | 18.50 | 29.74 | 31.96 | 56.1 | 0.113 | ||
| Time of postoperative evolution (months) | 30.64 | 13.4 | 23.56 | 9.78 | 0.101 | ||
| Type of impingement | |||||||
| Cam | 42.8 | 48.2 | 0.053 | ||||
| Pincer | 42.8 | 12.2 | |||||
| Mixed | 14.2 | 39.5 | |||||
| Socioeconomic level | |||||||
| 1 | 0.0 | 0.9 | 0.213 | ||||
| 2 | 0.0 | 9.9 | |||||
| 3 | 57.1 | 17.1 | |||||
| 4 | 14.2 | 24.3 | |||||
| 5 | 14.2 | 31.5 | |||||
| 6 | 14.2 | 16.2 | |||||
| Education | |||||||
| Illiterate | 0.0 | 0.9 | 0.753 | ||||
| Incomplete primary | 14.2 | 6.3 | |||||
| Complete primary | 0.0 | 4.5 | |||||
| Complete secondary | 14.2 | 18.9 | |||||
| Technical or vocational | 28.5 | 15.3 | |||||
| Professional | 42.8 | 54.9 | |||||
| Previous treatments | |||||||
| Analgesics | 14.2 | 33.3 | 0.160 | ||||
| Infiltrations | 42.8 | 12.6 | |||||
| Others | 0.0 | 1.8 | |||||
| None | 42.8 | 52.2 | |||||
| Postoperative treatments | |||||||
| Open surgery | 0.0 | 0.0 | <0.001b | ||||
| New arthroscopy | 100.0 | 0.0 | |||||
| Infiltrations | 0.0 | 9.9 | |||||
| None | 0.0 | 90.0 | |||||
Description of the demographic and clinical characteristics according to the result obtained after arthroscopic surgery in patients with femoroacetabular impingement.
| Variable | Result of the treatment | P | |||||
|---|---|---|---|---|---|---|---|
| Failure (n=7) | Success (n=172) | ||||||
| Mean | % | SD | Mean | % | SD | ||
| Preoperative assisted physical therapy | 42.8 | 41.4 | 1.00a | ||||
| Postoperative assisted physical therapy | 28.5 | 27.9 | 1.00a | ||||
| Posture at work | |||||||
| Sitting | 42.8 | 59.4 | |||||
| Standing | 57.1 | 36.9 | |||||
| Crouching | 0.0 | 2.7 | |||||
| Other | 0.0 | 0.9 | |||||
| Previous physical activity | 85.7 | 60.3 | 0.24a | ||||
| Previous competitive activity | 14.2 | 32.4 | 0.431a | ||||
| Weight (kg) | 59.43 | 9.03 | 67.28 | 12.18 | 0.067 | ||
| Height (cm) | 1.63 | 0.077 | 1.67 | 0.074 | 0.251 | ||
| Body mass index (kg/m2) | 22.35 | 2.83 | 23.94 | 4.27 | 0.210 | ||
| Internal snapping hip | 28.5 | 9.3 | 0.148a | ||||
| Retroversion | 14.2 | 6.9 | 0.416a | ||||
| Inguinal pain | 100.0 | 98.8 | 1.00a | ||||
| Sitting pain | 100.0 | 97.6 | 1.00a | ||||
| Pain when entering or exiting a car | 85.7 | 93.6 | 0.390a | ||||
| Block | 14.2 | 2.3 | 0.183a | ||||
| Locking | 0.0 | 23.2 | 0.351a | ||||
| Pain with rotational movement | 100.0 | 95.3 | 1.00a | ||||
| Logroll | 100.0 | 73.2 | 0.193a | ||||
| Impingement test | 100.0 | 96.5 | 1.00a | ||||
| Signs of apprehension | 0.0 | 2.9 | 1.00a | ||||
| Associated tendinitis | 28.5 | 6.9 | 0.095a | ||||
| “C” sign | 100.0 | 97.6 | 1.00a | ||||
| Cross over | 14.2 | 12.2 | 1.00a | ||||
| Alpha angle (degrees) | 54.14 | 10.18 | 60.23 | 6.052 | 0.143 | ||
| Center edge (degrees) | 38.57 | 9.21 | 36.57 | 8.14 | 0.525 | ||
| Trainee surgeon | 14.2 | 4.6 | 0.308a | ||||
| Neuropraxia of the pudendal nerve | 14.2 | 6.4 | 0.390a | ||||
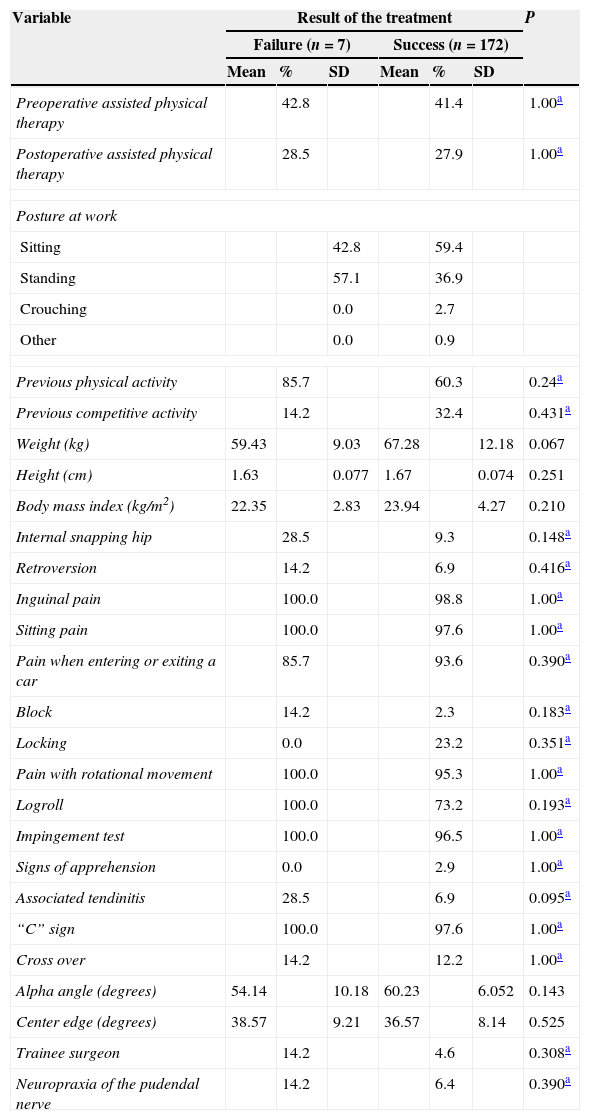
Out of the anatomical characteristics (radiographic and those observed and corrected during the arthroscopic procedure), osteochondroplasty was associated to the therapeutic failure, even after adjusting for age and gender (OR=0.07; 95% CI, 0.01–0.4; p=0.004) (Table 2).
Comparison between the anatomical findings and the procedures conducted based on the results of arthroscopic surgery obtained among patients with femoroacetabular impingement.
| Variable | Result of treatment | Raw OR | Adjusted OR | 95% CI of the adjusted OR | P | ||
|---|---|---|---|---|---|---|---|
| Failure (n=7) | Success (n=172) | Inferior | Superior | ||||
| % | % | ||||||
| Lesion of the acetabular cartilage | 14.3 | 40.1 | 0.2 | 0.2 | 0.2 | 2.1 | 0.200 |
| Chondroplasty | 14.3 | 17.4 | 0.78 | 0.78 | 0.8 | 6.9 | 0.827 |
| Resection of labrum | 14.3 | 33.1 | 0.33 | 0.37 | 0.04 | 3.2 | 0.369 |
| Reinsertion of labrum | 85.7 | 60.5 | 3.92 | 3.7 | 0.4 | 31.9 | 0.231 |
| Osteoplasty | 42.9 | 89.0 | 0.93 | 0.07 | 0.01 | 0.4 | 0.004a |
| Acetabuloplasty | 57.1 | 47.7 | 1.46 | 2.0 | 0.4 | 10.3 | 0.391 |
| Tenotomy of the psoas | 28.6 | 11.0 | 3.22 | 2.5 | 0.4 | 15.2 | 0.315 |
OR: odds ratio.
OR adjusted by age and gender.
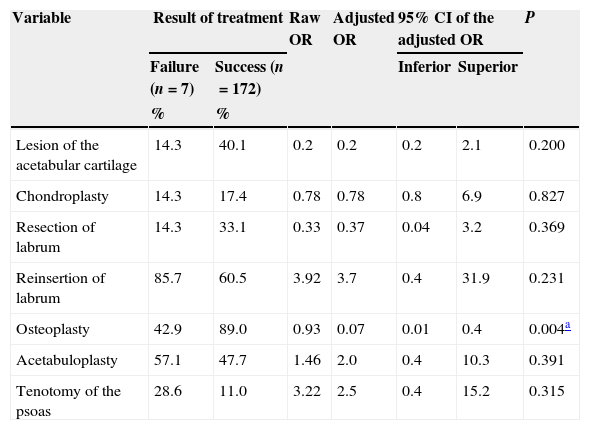
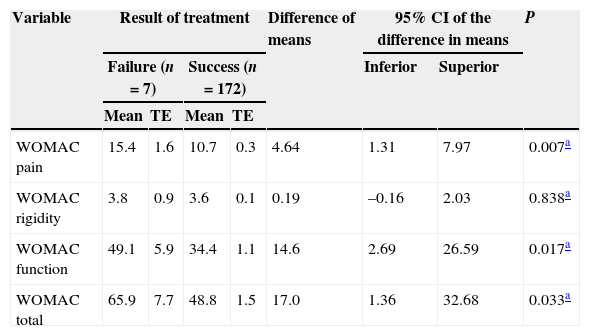
The mean preoperative WOMAC score was higher among the failure group compared to the success group in the domains of pain and functional capacity after adjusting for age and gender. For the pain domain, the mean value was 15.4 in the failure group compared to 10.7 in the success group (difference of 4.6; 95% CI, 1.3–7.9; P=0.007) and for functional capacity 49.1 compared to 34.4, respectively (difference of 14.6; 95% CI, 2.6–26.5; P=0.017). The mean preoperative WOMAC total score was also higher among the failure group compared to the success group, 65.9 versus 48.8, respectively (difference of 17.0; 95% CI, 1.3–32.6; P=0.033) (Table 3).
Comparison of the preoperative score in the WOMAC scale according to the results of arthroscopic surgery obtained among patients with femoroacetabular impingement.
| Variable | Result of treatment | Difference of means | 95% CI of the difference in means | P | ||||
|---|---|---|---|---|---|---|---|---|
| Failure (n=7) | Success (n=172) | Inferior | Superior | |||||
| Mean | TE | Mean | TE | |||||
| WOMAC pain | 15.4 | 1.6 | 10.7 | 0.3 | 4.64 | 1.31 | 7.97 | 0.007a |
| WOMAC rigidity | 3.8 | 0.9 | 3.6 | 0.1 | 0.19 | –0.16 | 2.03 | 0.838a |
| WOMAC function | 49.1 | 5.9 | 34.4 | 1.1 | 14.6 | 2.69 | 26.59 | 0.017a |
| WOMAC total | 65.9 | 7.7 | 48.8 | 1.5 | 17.0 | 1.36 | 32.68 | 0.033a |
TE: typical error.
The main finding of our study was the association between the scores in the preoperative WOMAC scale (in the domains of functional capacity, pain and overall score) and the failure of arthroscopic treatment in patients with FAA. Patients in whom the treatment failed had higher scores in the WOMAC scale than those in whom the treatment was successful.
To date, there are no reports in the literature of studies finding an association between high scores in the WOMAC scale and a poor subsequent arthroscopic result. Nevertheless, the study conducted in 2010 by Gedouin et al. revealed that patients with radiographic findings compatible with hip OA obtained higher scores in the WOMAC scales and worse postoperative results. As in our study, the differences in the pre- and postoperative scores between patients in whom the treatment failed or was successful were statistically significant.31 In 2012, Philippon et al. published a study on patients older than 50 years, in whom the modified Harris hip score (MHHS) was used before and after surgery to measure the results of the intervention. After adjusting by days of evolution of the lesion and by gender, the study reported that preoperative scores lower than 50 in the MHHS were associated to the need for total hip joint replacement.32
In our study we did not find an association between the anatomical characteristics, specifically those related to the arthroscopic procedure, and the result of the treatment. Within the anatomical characteristics we included repairs and modelings to guarantee hips which were as similar as possible to a normal hip. On the other hand, a study conducted in 2012 compared 2 cohorts of patients with pincer type and mixed FAA, one undergoing resection and debridement of the labrum and the other undergoing repair, using the MHHS, a quality of life questionnaire (SF-12) and an analog visual scale (VAS) for pre- and postoperative pain, and found statistically significant differences in some of these scores: MHHS (p=0.01), SF-12 (p=0.41) and VAS (p=0.04) favoring the labral repair group. Follow-up of these patients lasted for 3.5 years and it is worth noting that the results were not adjusted for any confounding factors.33
Prior to this work, a German study conducted in 2009 evaluated the performance of a minimally invasive approach through NAHS and described in detail the surgical procedure conducted on patients. This included 100 hips with a mean follow-up of 54 months. Like in our study, labral reinsertion was not correlated with the NAHS scores (87±11 versus 82±19, p=0.13) at the end of the follow-up period.34
Another German study, which assessed the usefulness of a minimally invasive approach, proceeded according to the findings in patients with all types of FAA. The authors measured the results through the WOMAC scale and the Oxford hip index after a mean follow-up of 15 months. The Oxford index showed an improvement from 34.3±9.8 points prior to the procedure to 16.3±11.0 points after it, whilst the WOMAC scale varied from 60.8±23.1 points to 84±15.1 points at the time of the last assessment.35 This study did not evaluate the specific characteristics of the arthroscopic procedure.
In 2000, a prospective study with a follow-up period of 2 years found an association between the time of onset of pain and poor results in hip arthroscopy.36 It is worth noting that this work evaluated patients undergoing hip arthroscopy regardless of the baseline diagnosis and that the subsequent assessment was carried out using the Harris scale, which is not the same as the one used in our work. This study also reported an association with patient age, unlike our results, which showed no significant differences between the ages of patients in whom the treatment failed or succeeded. Findings differing from ours have also been reported by other studies, where patients over 40 years of age were associated to worse postoperative outcomes, like the grade of acetabular lesion and femoral head deformity.37
Other studies have found an association between established hip OA and poor postoperative results.22,38 Due to the consistency of this association evaluated in other studies, we decided to exclude these patients to avoid any confusion bias that this variable could cause. Another factor that has been associated to poor postoperative results is greater cartilage damage39; however this association was not observed in our study.
It is important to highlight that the literature contains no evidence of an association between the interventions conducted in the arthroscopic procedure and failure of treatment. In our study we found no association between microfractures, chondroplasty, resection and reinsertion of the labrum, acetabuloplasty and tenotomy of the psoas and the result of treatment; however, osteoplasty showed an association with better treatment results.
The WOMAC scale is a valuable tool for the functional assessment of patients with hip pathologies; it has widespread international recognition and has been translated and validated in various countries, including Spain and Peru. This widespread recognition enables its use for preoperative approximation, despite the fact that its original development was conducted on patients with arthritic hips. The scores should be correlated with the clinical symptoms of patients and we must bear in mind that its original aim was not specific for clinical hip conditions.
The WOMAC scale comprises 3 domains of great importance in quality of life of patients and carrying out activities of daily life. This enables physicians to identify the main needs and ailments of patients requiring intervention for their daily lives. Based on the results of this study, the systematic application of this scale to patients with FAA candidates for hip arthroscopy will enable physicians to identify with greater accuracy those patients who would benefit from this procedure and offer different alternatives to subjects with high scores in the overall WOMAC scale and, specifically, in the functional capacity domain, taking into account other clinical and social characteristics to guarantee that the treatment selected fulfills the expectations.
Bearing in mind the results of our study, we suggest paying greater attention to the functional and pain characteristics of patients, since these are the domains with greater contributions to the scale. It appears that placing greater emphasis on these variables would enable better patient discrimination and detection of those with high or low probabilities of success after arthroscopic treatment.
LimitationsThe main limitation of our study lied in the loss of some follow-up variables, despite complying with the estimated sample size. The follow-up losses corresponded to 10.5% of the sample and we acknowledge that they could influence the final estimation of results. However, there were no differences between included and lost patients. The varying characteristics of our population made the retrieval of all patients for subsequent evaluation more laborious, and even impossible in some cases, despite the efforts to this effect.
The lack of agreement in the literature regarding the definition of treatment failure, associated to an absence of scales validated in our medium which enabled a better assessment of the surgical outcome of patients, hindered the evaluation of results and patient prognoses. Further efforts should be aimed toward subsequent development.
The low frequency of the outcome led to difficulties for the statistical methods employed in the comparisons. Nevertheless, this could be explained by the experience of the treating surgeon, who has improved his technique over the years, thus leading to highly satisfactory results in the majority of patients. A proof of this is the low frequency of neuropraxia of the pudendal nerve (6.7%), one of the most common complications in this procedure. On the other hand, despite the low frequency, the outcome evaluated was objective and defined treatment failure with no risk of varying interpretations by patients and examiners.
Further studies are required in order to identify the association with other variables which were not considered in this work, so as to establish eligibility criteria for arthroscopic treatment among patients with FAA.
ConclusionsA poor functional condition prior to arthroscopic treatment of FAA, mainly as regards preoperative pain assessed by the WOMAC scale, was associated to a higher rate of therapeutic failure.
Level of evidenceLevel of evidence iii.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Martínez D, Gómez-Hoyos J, Márquez W, Gallo J. Factores asociados al fracaso terapéutico de la cirugía artroscópica en pacientes con choque femoroacetabular: un estudio de cohorte. Rev Esp Cir Ortop Traumatol. 2015;59:112–121.